Fig. 1
One-time pretreatment, 1 day prior to surgical brain injury: (a) postoperative brain water content; (b) modified 21-point sensorimotor score; (c) left-sided (contralateral to injured area) percentage of correct vibrissae-elicited forelimb placements, from total attempts; (d) right-sided percentage of correct vibrissae-elicited forelimb placements, from total attempts. *p < 0.05 when compared with sham group. Thrombin intracerebral ventricular (ICV) or intranasal (IN) administration did not differ significantly from vehicle
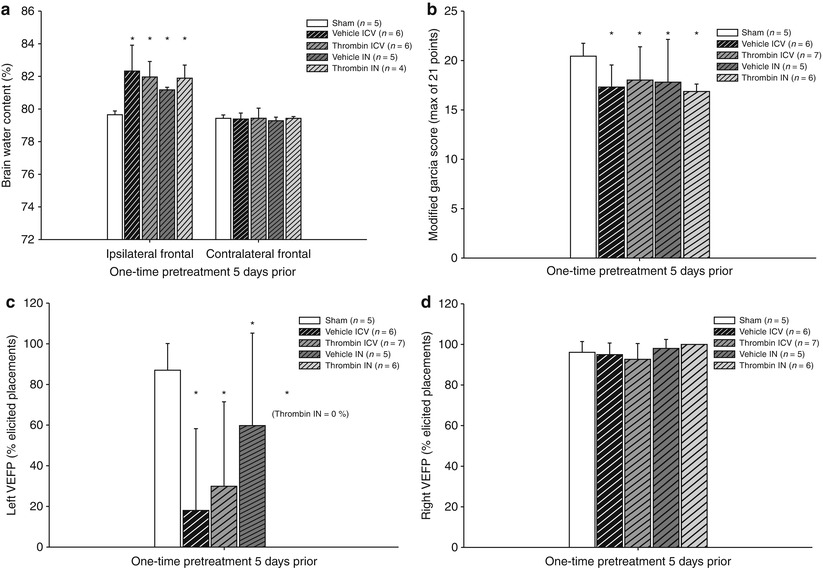
Fig. 2
One-time pretreatment, 5 days prior to surgical brain injury: (a) postoperative brain water content; (b) modified 21-point sensorimotor score; (c) left-sided (contralateral to injured area) percentage of correct vibrissae-elicited forelimb placements, from total attempts; (d) right-sided percentage of correct vibrissae-elicited forelimb placements, from total attempts. *p < 0.05 when compared with sham group. Thrombin intracerebral ventricular (ICV) or intranasal (IN) administration did not differ significantly from vehicle. Thrombin IN left vibrissae-elicited forelimb placement had zero correct placements
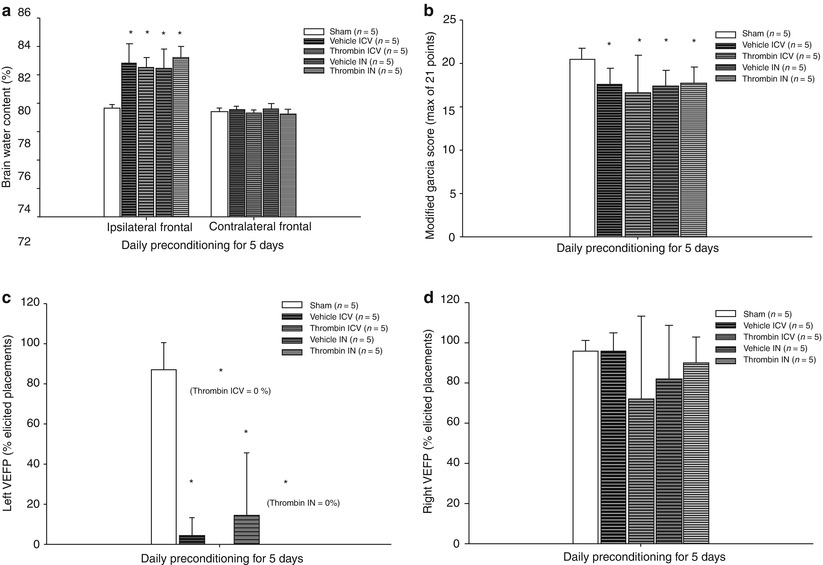
Fig. 3
Daily preconditioning for 5 days prior to surgical brain injury: (a) postoperative brain water content; (b) modified 21-point sensorimotor score; (c) left-sided (contralateral to injured area) percentage of correct vibrissae-elicited forelimb placements, from total attempts; (d) right-sided percentage of correct vibrissae-elicited forelimb placements, from total attempts. *p < 0.05 when compared with sham group. Thrombin intracerebral ventricular (ICV) or intranasal (IN) administration did not differ significantly from vehicle. Thrombin ICV and IN left vibrissae-elicited forelimb placements had zero placements
Pretreatment or Preconditioning with Thrombin Does Not Improve Neurological Scores
There also was a significant difference between all groups of animals in the vibrissae-elicited forelimb placement test (p < 0.001). Sham and treatment groups were significantly different (p < 0.05), but thrombin- and vehicle-treated animals were not, regardless of route or timing of administration (Figs. 1, 2, and 3; p > 0.05). Statistical analysis of the modified 21-point sensorimotor test results showed no difference between all groups (p = 0.8).
Discussion
This study was designed to assess the outcome impact of thrombin pretreatment and preconditioning via intranasal and ICV administration routes in a model of surgical brain injury in rats as either reduction in brain edema or improvement in neurological function 24 h after surgical brain injury. Although thrombin preconditioning via ICV or intracerebral injection has been shown to effectively decrease brain edema in models of ischemic brain injury in rodents [6, 17], in the present study pretreatment or preconditioning with thrombin did not change any of these outcomes in comparison with control groups. Several factors could have contributed to this.
In addition to testing whether the benefit of thrombin pretreatment could be obtained in a surgical brain injury model, this study was designed to find a clinically relevant way to deliver the therapy. We chose the intranasal route to the cerebral spinal fluid (CSF) paired with ICV injections to compare the two methods of delivery for efficacy. However, because no significant result was seen from deliberate placement of thrombin into the CSF via the ICV route, or by presumed transport to the CSF via the IN route, we found it unnecessary to ascertain whether IN administration of thrombin was as effective as ICV. The fact that no improvement in outcomes was found likely is attributable to the type of injury. The injured area in the surgical brain injury model is very large, and areas further away from the cerebral ventricles may never interact with the thrombin. In this model, the blood-brain barrier is mechanically disrupted, exposing brain parenchyma directly to blood and irrigation fluids across a sizable area. Any intracellular change that may improve localized disease from edema could be masked by the magnitude of injury caused in this model. Our goal was to find a clinically relevant therapy, and therefore the cohort size was powered to find only large treatment effects as in previous studies [1].
The lack of a significant difference between any of the treatment groups and the sham group in the modified 21-point sensorimotor exam was a confounding result. This test has been shown to give consistent results even between different observers, which correlate to the amount of diseased tissue [12]. Two experienced observers were used for this test and both were blinded to the groups, so it is unlikely that bias could have been inadvertently introduced. There were several outlying scores in the 1 day prior thrombin ICV and IN pretreatment groups that could have distorted the data. Also, although all the other treatment groups show a significant difference when compared with sham in the sensorimotor exam, that difference is still relatively small. In a previous study, it was shown that increased brain water content in this model correlated with worsened neurological outcome [1]. The vibrissae-elicited forelimb placement test demonstrated that in this study, and it may be better suited for demonstrating the degree of injury for comparison.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








