Fig. 17.1
The role of Halo-gravity traction primarily in treating severe pediatric spinal deformity
The halo ring is placed using 6–8 pins, pins are spaced around the skull; our institutional experience has shown that using this number of pins decreases the incidence of any one pin experiencing loosening or infection. Pins are tightened to a torque equaling the age of the child up to the adult torque limit of 8–10 in.-pounds; for example, a 4-year-old patient’s pins are tightened to 4 in.-pounds of torque using a calibrated torque wrench. Pin care involves inspection and cleaning of each pin site daily – cleaning solution is simply soap and water – and leaving to air dry. If crusting is noted at a pin site, a solution of 50 % sterile saline and hydrogen peroxide is used to clean the site. Infected pins are exchanged as necessary.
The day after halo ring placement, the patient is placed upright in overhead traction via a traction bale attached to a wheelchair or a standing frame, using a spring-loaded fish scale or other dynamic traction device, with an initial traction of 5–10 lb; at night the patient has a bed traction device that utilizes weights) [7]. The time in traction and the amount of weight are increased to tolerance, with careful neurologic monitoring. All patients need cranial nerve testing once during each shift while upright in traction, and in patients with preexisting neurologic signs, lower extremity strength and reflexes are monitored as well during the phase of increasing traction (Fig. 17.2). Eventually, a traction force exceeding 50 % of body weight may be achieved in smaller children. The traction is increased so that the patient’s buttocks are lifted slightly off the wheelchair seat while sitting; in the standing frame, the patient should be up just on tiptoes. The safety of this method is ensured by the patient’s ability to easily relieve the traction by pushing up on the wheelchair arms or walker hand rails in response to pain or neurologic symptoms. Typically, treatment with traction requires a hospital stay of 4–8 weeks, although some patients are allowed to continue as outpatients after adequate in-hospital caregiver education with the traction device. In our series of more than 100 patients treated with traction at Texas Scottish Rite Hospital for Children, only 2 neurologic complications related to traction have occurred. One patient with Klippel–Feil syndrome and multiple cervical synostoses developed mouth and facial numbness when a C3–4 distraction occurred at the only nonfused level in the neck. This resolved after traction was discontinued and converted to a halo vest for 6 weeks. Another patient with incomplete resection of an intrathecal ganglioneuroma and pre-traction hyperreflexia developed paraparesis, necessitating that traction be discontinued. Another report of 33 patients treated in traction noted two possible neurologic complications: nystagmus and dizziness [8].
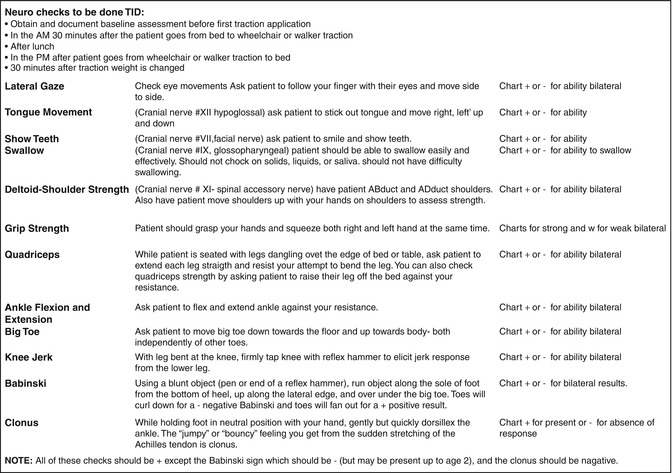
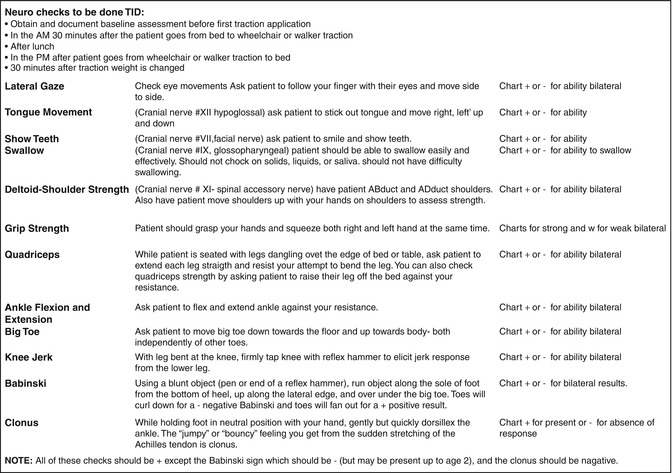
Fig. 17.2
Cranial nerve testing
17.5 Postoperative Care
Most surgeons will monitor the patient in an intensive care unit (ICU) or step down unit for the first 2–3 days, with additional monitoring (arterial pressure line, and/or central venous pressure line) for the first 1–2 days; some patients may require use of a ventilator during this time. Pain management may be epidural analgesia, patient-controlled analgesia pump, or sliding scale intravenous pain medication. Oral narcotic analgesia can be resumed usually by day 2 or 3. Prophylactic prevention of deep vein thrombosis (DVTs) may involve frequent logrolling in bed and the use of thrombo-embolism deterrent hose (TEDs) and sequential compression devices (SCDS), particularly in patients over 60 years of age. Activity is advanced from sitting up in the chair 24 h after surgery to being able to walk a few laps around the nursing unit by day 3 or 4. Some facilities continue the use of supplemental nutrition through a gastrostomy tube or paraenteral alimentation, in more complex deformity patients. The surgical dressing placed intraoperatively is usually reinforced unless excessive drainage is present; most surgeons change the original dressing on postoperative day 3 or 4. Surgeon preference may include the use of a Jackson–Pratt/Hemovac drain inserted into the wound; typically these drains are removed postoperative day 2 or 3; however, if excessive drainage is present, the drain may be left in till the output decreases. Some patients will experience gastrointestinal complications such as an ileus or constipation, despite being treated with routine postoperative stool softeners and oral laxatives; often use of a suppository or enema is needed. Resumption of activities such as walking, increasing water intake, and eating a high fiber diet should help with slow return to normal gastrointestinal function. Pediatric patients are typically discharged between postoperative day 5–7, and adults between day 6–8, by this point they will be ambulating 2–3 times a day, will have resumed a normal diet, have had a bowel movement and have all drains and catheters removed. Patients are discharged with a 1–2 week supply of narcotic pain medication as well as stool softeners. They are educated regarding modified activity and how to advance it until first postoperative visit; they may shower anywhere from 1 to 2 weeks after surgery, depending on surgeon preference. In cases where a selective fusion is performed or limited implants are placed due to difficult anatomy or osteopenic bone, a cast or brace may be utilized for 3–6 months postoperatively. Most patients will return for their first postoperative visit 2–4 weeks after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







