Prosthetic Disc Nucleus: Treatment with the Anterior Approach
Peter Donkersloot
Chronic low back pain is a common problem in our society. Where does conservative treatment end and surgical therapy begin? The idea of treating patients with pain caused by the initial stage of degenerative disc disease (DDD) is attractive, because it is surgically possible to stabilize the affected motion segment with a nucleus prosthesis only. Contrary to treatment with a total disc replacement, the surgical procedure could be less extensive as only a minimally invasive nucleotomy is required.
The selection of proper candidates for surgical treatment is still controversial, especially because the correlation between the morphologic and radiologic changes in the initial degenerated disc with the patient’s complaints has until now not been fully clear.
The optimal indication for treatment with a prosthetic disc nucleus (PDN) is a patient with a more than 6-month history of low back pain with or without leg pain, not responding to conservative treatment, due to the initial degree of disc degeneration. It is possible to treat more than one level (1,2).
The Prosthetic Disc Nucleus
The PDN is a hydrogel core that can absorb up to 80% of its weight in water and so it expands when it is implanted in a surgically prepared disc nucleus cavity. Water absorption allows the device to swell and to maintain the disc height, resulting in stabilization of the motion segment. The hydrated core mimics the biomechanical features including cushioning of a healthy disc nucleus. The polymer core is encased in a polyethylene jacket that helps to preserve the device shape during heavy loading in the motion segment (2).
The PDN device passed biomechanical tests, showing that the device is able to maintain disc height, structural integrity, and burst strength up to 50 million cycles, with loads ranging from 200 to 800 N with no significant wear debris (3). The biocompatibility, systemic toxicity, genotoxicity, and carcinogenicity have also been successfully tested (4,5).
Eysel et al. (6) published the results of the biomechanical behavior of the PDN device on 11 cadaveric lumbar spinal motion segments. Physiologic testing of intact lumbar segments, nucleotomized segments, and segments with two implanted PDN prostheses were performed to analyze changes in segmental mobility. Removal of the major part of the disc nucleus led to an increase in mobility ranging from 38% to 100%. The insertion of two PDN implants restored disc height and reconstituted the mobility of the implanted segment similar to the prenucleotomized level (6,7). Note that these studies
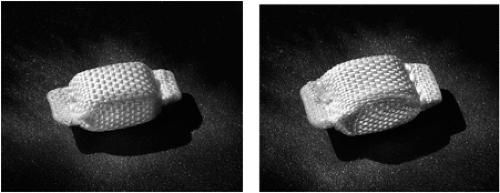
report on the first generation of PDN (duo) implants, which were smaller than the present ones. Nowadays two types of single-unit devices are available: the PDN-solo for discs with an anteroposterior (AP) diameter of less than 35 mm and the PDN-solo XL for those with an AP diameter more than 35 mm (Fig. 13.1).
report on the first generation of PDN (duo) implants, which were smaller than the present ones. Nowadays two types of single-unit devices are available: the PDN-solo for discs with an anteroposterior (AP) diameter of less than 35 mm and the PDN-solo XL for those with an AP diameter more than 35 mm (Fig. 13.1).
Disc Degeneration—Magnetic Resonance Imaging Discography
The very initial stage of disc degeneration was described by Crock (8) as internal disc disruption (IDD). At about 30 years of age the nucleus begins to dehydrate and shrink, resulting in a loss of function and therefore more mechanical stress on the annulus fibrosus (9). The nucleus itself is not innervated; nerve structures are found in the outer part of the annulus fibrosus. These have their origin in the disc surrounding plexus of interlacing nerve fibers localized around the anterior and posterior longitudinal ligament (10). The dorsal part of this plexus is supplied by the recurrent sinuvertebral nerve, which consists of branches of the sympathetic trunk, the rami communicantes, and the dorsal root ganglion. The innervation is not monosegmental, but one or more segments above and below can contribute to the innervation of one single disc level (11,12,13).
The clinical implication is that more load leads to a small disruption of the annulus fibrosus, which causes pain. Because of the multisegmental innervation of the interver-tebral disc, the determination of the source of the pain could be difficult if there is more than one affected level.
The magnetic resonance imaging (MRI) examination is the gold standard for the detection of DDD. It is widely available and noninvasive and has been shown to be very sensitive in detecting abnormalities in disc morphology. T1 and T2 weighted sequences in the sagittal and axial direction are clinically used. More sophisticated use of MRI, such as magnetic resonance spectroscopy, functional and dynamic imaging, is so far not available in daily routines (14).
In the initial stage of DDD, the MRI shows a “black disc,” sometimes in combi-nation with a slight loss of disc space height and a small rupture of the posterior part of the annulus. Although there is significant controversy as to whether discography adds any diagnostic data greater than those provided by the noninvasive MRI (15), others
think that because discogenic pain is caused by internal disruption of the normal structural integrity of the symptomatic disc, discography is necessary to establish and confirm this diagnosis. This means that the primary indication for lumbar discog-raphy is chronic low back pain with or without radicular pain in the absence of MRI-documented neural compression (16).
think that because discogenic pain is caused by internal disruption of the normal structural integrity of the symptomatic disc, discography is necessary to establish and confirm this diagnosis. This means that the primary indication for lumbar discog-raphy is chronic low back pain with or without radicular pain in the absence of MRI-documented neural compression (16).
It is believed that the pain generated by discography occurs when annular fissures or nuclear herniations extend into the outer third of the annulus fibrosis (17). In 1990, Walsh et al. (18) performed a controlled prospective study to establish the specificity of lumbar discography by comparing the results of 10 asymptomatic volunteers with those of 7 patients with chronic low back pain. In this study, the discogram only was defined as “positive” when, with an accurately placed injection in the center of the nucleus, the typical pain could be induced (positive pain provocation). Based on this criterion, there were no positive discograms demonstrated in the asymptomatic individuals (a false-positive rate of 0% and a specificity of 100%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree