Fig. 14.1
Proximal junctional failure with fracture through the upper instrumented vertebra. A sharp transition of rigid proximal end fixation using two pedicle screws at the same level predisposes to failure. (a) Failure at distal thoracic region (below the apex of thoracic kyphosis) usually occurs in the form of compression fracture (b)

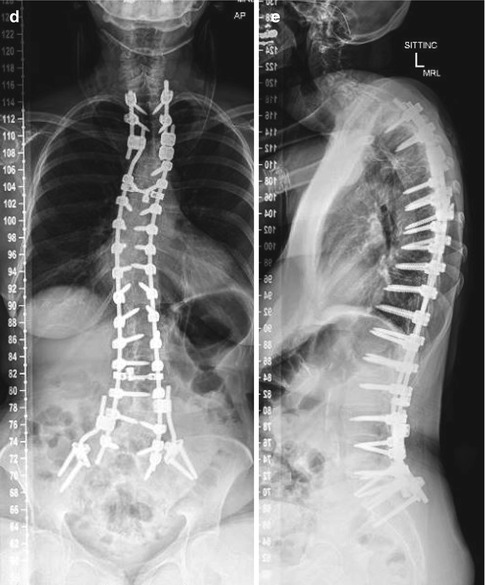
Fig. 14.2
The mode of proximal junctional failure in the upper thoracic region (above the thoracic kyphosis) (a) usually occurs due to ligamentous disruption leading to subluxation of the motion segment (b) and may lead to spinal cord compression (c). This was promptly revised by removal of the proximal hook and extension of fusion to further cranial level (d, e) (Reproduced with modification from Sengupta [18])
Therefore, strategies to avoid PJK in patients with UIV in distal thoracic region may include vertebral augmentation to prevent fracture. In contrast, when the UIV is selected at the upper thoracic region, it may be more appropriate to adopt a mechanical means to prevent vertebral subluxation, like minimizing implant density, softer transition, etc., as described in the subsequent section [16].
14.2.4 Strategies and Planning of Proximal Junctional Fixation to Prevent PJF
14.2.4.1 Selection of Level for Proximal End of Fixation (UIV)
The apex of thoracic kyphosis is normally at T7-T8, but it can vary in individual cases. It is generally agreed that the proximal end of fixation should not end at the apex of thoracic kyphosis; fixation should preferably be stopped caudal to, or extended cranial to the apex of kyphosis [18]. (Fig. 14.3)
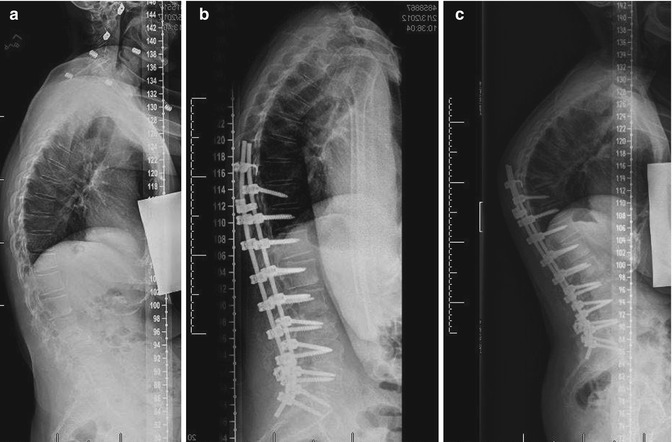
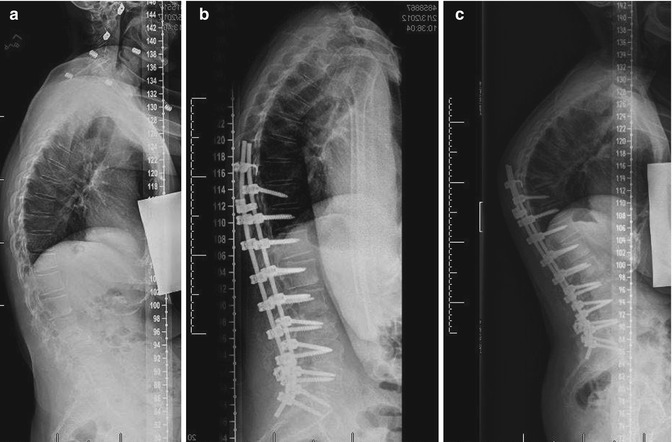
Fig. 14.3
Upper instrumented vertebra at the level of apex of thoracic kyphosis (T9 in this case, a and b) predisposes to PJK (c)
There is a general perception that stopping proximal fixation at the thoracolumbar junction may predispose to PJK because of increase in stress at the junction of rigid thoracic spine and rigid lumbar spine after instrumentation; therefore it is generally recommended that the fixation should be extended proximally to T10 or higher. However, there is no evidence in the literature to support that fusion ending at T11, T12, or L1 makes any difference in the incidence of PJK, provided there is no preexisting focal kyphosis at these levels [12]. Presence of any bridging anterior osteophyte at the thoracolumbar junction may provide additional protection against PJK if the fixation stopped at this level.
The proximal-end fixation cranial to the apex of thoracic kyphosis, which is usually at T7-T8, may be selected between T1 and T6 levels. The preference between T1-T3 vs. T5-T6 remains open to debate. Some authors believe T1-T3 is preferable to T5-T6, with lesser incidence of symptomatic PJK. However, stopping at the cervicothoracic junction may pose a similar concern of a sharp transition between a relatively mobile cervical and rigid thoracic spine, as in the thoracolumbar junction. Treatment of subsequent PJK at the cervicothoracic junction may be more difficult than at T5-T6. In either case, proximal thoracic failure mode usually involves ligament disruption leading to subluxation of the vertebra and may involve neurological deficit [16, 19]. Therefore, it is important to protect the ligament complex during proximal-end instrumentation.
14.2.4.2 Extent of Fusion
Most authors agree that extension of fixation to sacrum or pelvis predisposes to PJK [12–14]. Stopping the caudal fixation at L5 or higher may protect the proximal-end fixation to some extent. But presence of significant disc/facet degeneration at the caudal end of fixation may lead to early distal junctional failure.
Comparing a long-fusion “T3-sacrum” (PT or proximal thoracic group) to a short-fusion “T10-sacrum” (DT or distal thoracic group) in primary surgery for adult scoliosis, O’Shaughnessy et al. [19] reported that the PT group experienced an increased number of perioperative complications (30.0 % vs. 15.8 %), more pseudarthrosis (20.0 % vs. 5.3 %), and a higher prevalence of revision surgery (20.0 % vs. 10.5 %); the DT group had more proximal junctional kyphosis (18.4 % vs. 10.0 %). The authors concluded that short fusions may result in a more proximal junctional kyphosis, but only rarely require revision surgery.
14.2.4.3 Restoration of Proper Sagittal Balance
Postoperative hyperkyphosis and hypokyphosis of the thoracic spine can both predispose PJK [13]. Kim et al. [20] reported that higher post-op lumbar lordosis and larger sagittal balance corrections may lead to an increased incidence of PJK. Proximal junctional kyphosis developed in those patients in whom the thoracic kyphosis remained greater in magnitude relative to the lumbar lordosis [9]. Therefore the magnitude of postoperative thoracic kyphosis should match the LL. In addition, the magnitude of normal lumbar lordosis (LL) in an individual is strongly influenced by pelvic incidence (PI) [21]. Schwab et al. [22] suggested a method to estimate an ideal LL from the PI of the individual by a formula: normal LL = PI +/−10°. Persistent pelvic retroversion following surgery, which indicates an attempt to compensate a hidden sagittal imbalance, may also predispose to PJK [9].
14.2.4.4 Execution of Appropriate Techniques of Proximal Junctional Fixation to Prevent PJF
The surgical techniques for proximal junctional fixation to prevent PJF should be aimed at: (a) reduction of the rigidity of fixation, (b) increasing the strength of the anchor point, and (c) increasing the strength of the ligament–bone complex which holds the anchor point.
Rigidity of Cranial-End Fixation
This is the most important technical point for successful proximal junctional fixation. Finite element analysis (FEA) study showed that there is abnormally high stress at the cranial-end of fixation due to sudden change in the rigidity of the instrumented to the cranial mobile segment of the spine, which may manifest by increased nucleus pressure in the motions segment and the stress at the implant itself. [23] Several strategies have been suggested in another biomechanical model to reduce the stress at the proximal-end implant and implant–bone junction [24].
The rigidity of the fixation can be reduced by the following methods:
(i)
Avoiding any correction of kyphosis between the terminal implanted segments
Correction of the kyphotic deformity may be achieved by applying a compression force between the adjacent implants in the thoracic spine. Application of such correcting force between the proximal-end screw and the adjacent screw significantly increases the stress at the proximal junction, predisposing to PJK. It is therefore important not to apply any compression force across the proximal-end fixation points.
(ii)
Avoiding pedicle screws on both sides at the end vertebra; instead using a hook at the cranial end
In a biomechanical study, Cammarata et al. [24] found 26 % reduction in the stress factors at the proximal junctional fixation by using transverse process hooks as compared to pedicle screws. In a review article, Helgeson et al. [11] reported increased incidence of PJK in an all-screw construct compared to a hybrid (hook-screw) or all-hook construct at the cranial-end fixation [11] (Fig. 14.1).
(iii)
Reducing implant density at the proximal end
It may be advantageous to leave some segments free without any pedicle screws, close to the end of the instrumentation, so that the rod keeps its elastic movement and the whole construct [12] (Fig. 14.4).
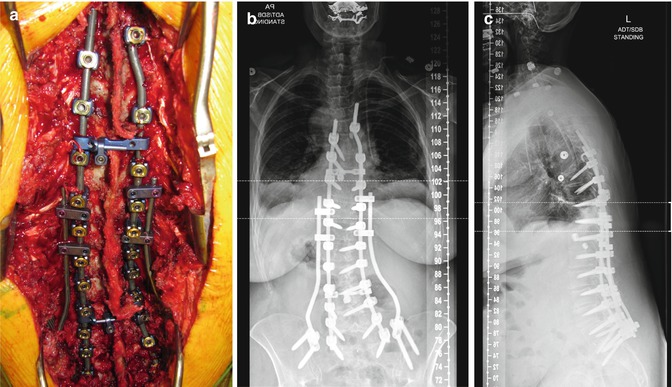
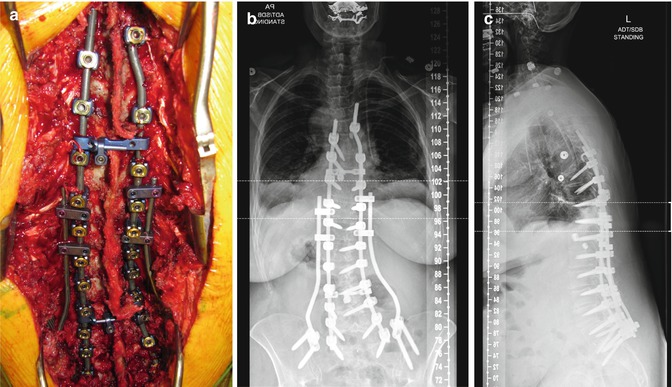
Fig. 14.4
Author’s preferred technique for proximal junctional fixation. (a) Clinical photograph – note on the right a claw construct between a supralaminar hook at the cranial end fixation and a pedicle screw placed at the second lower vertebra, skipping a vertebra to reduce the implant density. On the left side, the cranial end fixation ended one segment lower than on the right side. This reduces the rigidity of cranial end fixation. (b, c) AP and lateral radiograph. The rod on the right side is bent in medial direction to align against the pedicle screw and the supralaminar hook. Note that the cranial end pedicle screws are placed caudally, directed to be more efficient against a direct pull-out force, as opposed to the remaining pedicle screws placed conventionally, parallel to the superior end plate
(iv)
Use of a tapered rod at the proximal end
Cammarata et al. [24], in a biomechanical study, reported that the use of proximal transition rods with reduced proximal diameter from 5.5 mm to 4 mm decreased the proximal junctional stress significantly. In another finite element analysis, Cahill et al. [23] reported significant reduction of nucleus pressure in the immediate cranial adjacent segment with the use of a tapered transition rod compared to a standard rod. No clinical experience with such rods has been reported as yet.
(v)
Use of a dynamic stabilization system at the cranial-end fixation
The author reported a pilot clinical study with the use of a dynamic stabilization system (Transition™ Globus Medical Inc., Audobon, PA, USA) for cranial-end fixation in adult deformity, with no incidence of PJK in 5 years follow-up (Fig. 14.5). The authors also reported a biomechanical study on a spine model using the same system and reported that the dynamic stabilization system reduced the stress at the proximal-end screw, and also the nucleus pressure at the cranial adjacent segment, compared to the use of a standard rigid rod fixation (Fig. 14.6).
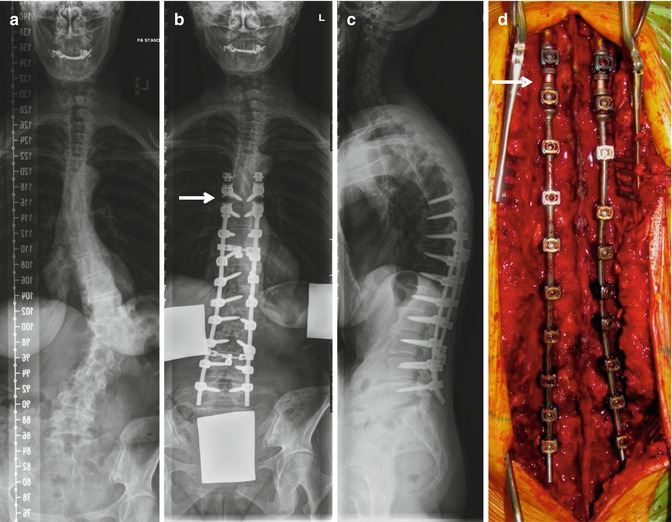
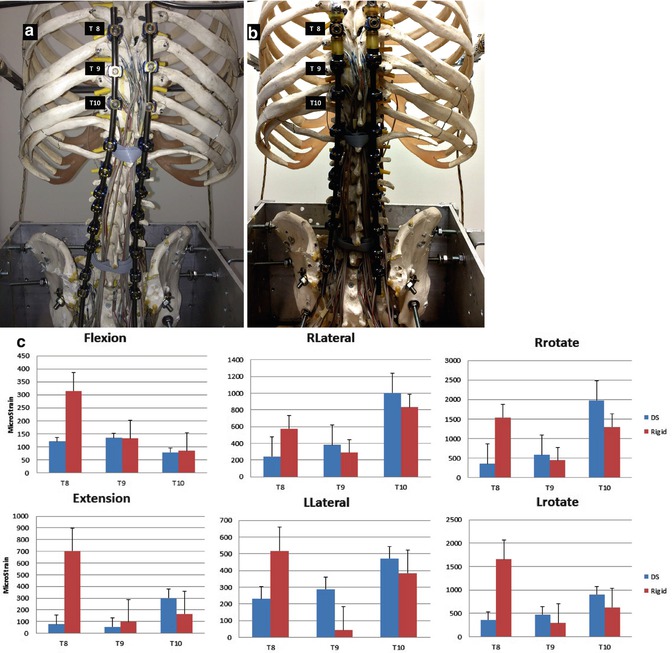
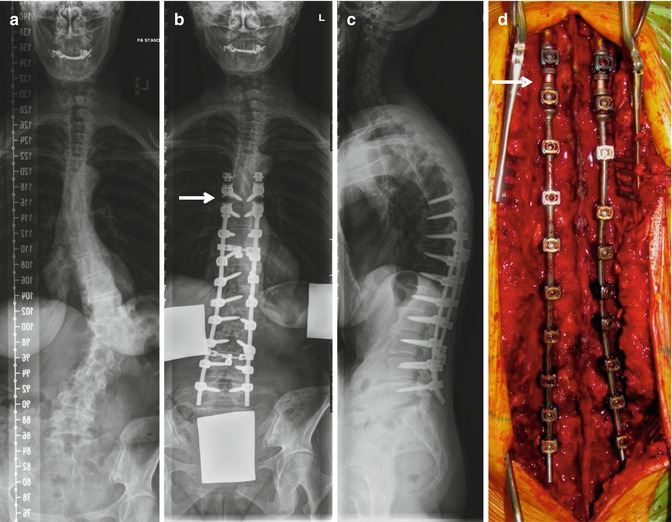
Fig. 14.5
AIS in adult thoraco lumbar scoliosis (a), corrected with posterior instrumentation from T8-L5. (b–d). Note the dynamic stabilization between T8 and T9 (arrow) using Transition™ system (Globus Medical Inc. Audobon, PA) at the cranial end for smooth transition of the rigidity of fixation between the instrumented and uninstrumented segment to prevent PJK (Reproduced with modification from Sengupta [18])
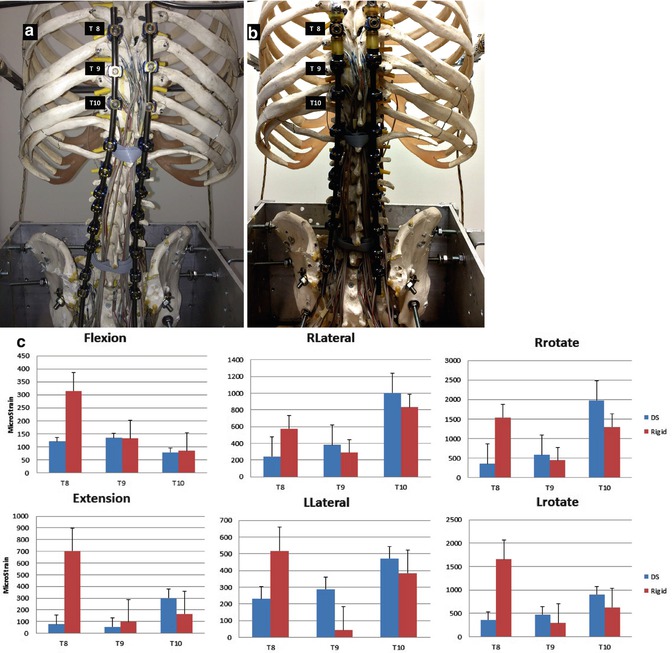
Fig. 14.6
Biomechanical study of the pedicle screw strain at the proximal junctional fixation (T8, T9, T10) comparing standard rigid rod fixation (a) to dynamic stabilization using Transition™ system (b) between the cranial pedicle screw at T8 and T9, loading the cranial end of the spine model in different directions. (c) The strain at the proximal end pedicle screw (T8) is significantly higher with rigid rod fixation (red) compared to dynamic stabilization (blue) in flexion, extension, left and right lateral bending (Llateral and Rlateral respectively), and left and right rotation (Lrotate and Rrotate respectively). The strains at T9 and T10 (second and third pedicle screws from the end fixation) are slightly higher with dynamic stabilization (blue) compared to standard rigid rod fixation (red), indicating that dynamic stabilization significantly dampens the strain at the end fixation and transmits the load to the next pedicle screws
Increasing the Strength of the Anchor Point or Pull-Out Strength
This may prevent screw pull-out or hardware failure. This is more important in distal junctional failure, as has been discussed in the later section.
(vi)
Use of a claw–construct
Generally, pedicle screws offer a better anchor point strength compared to hooks against pull-out. However, a claw-construct, with combination of a supralaminar hook cranially and pedicle hook caudally, produced a superior pull-out strength compared to pedicle screw alone in a biomechanical study on the cadaveric thoracic spine [25]. The present author prefers to use a claw-construct between a supralaminar hook and a pedicle screw (Fig. 14.5).
(vii)
Use of a caudally directed thoracic pedicle screw
Thoracic pedicle screws are generally inserted parallel to the superior endplate of the corresponding vertebra. The author described a technique to insert the thoracic pedicle screws, particularly the cranial-end screws directed caudally, starting at the cranial edge of the pedicle and aiming at the inferior endplate of the vertebra [26]. Intuitively, a pedicle screw inserted parallel to the superior endplate of the vertebra may be less efficient to resist a direct pull-out force parallel to the superior endplate, that is, in line with the screw shaft, as compared to a caudally directed screw, where the screw shaft is at an angle to the pull-out force (Fig. 14.5).
Increasing the Strength of the Ligament–Bone Complex Which Holds the Anchor
This is no less important factor in the prevention of the PJF.
(viii)
Avoiding damage to the ligament complex
Biomechanical analysis or finite element analysis in a long thoracic spine instrumentation model indicated that damage to the supraspinous and interspinous ligament immediately cranial to the instrumented segment may increase the nucleus pressure by more than 50 %, and angular displacement by 19–26 % against a compression load leading to kyphosis [23]. In another biomechanical study, Cammarata et al. [24] reported that the bilateral complete facetectomy, the posterior ligaments resection, and the combination of both increased the proximal junctional kyphotic angle by 10 %, 28 %, and 53 %, respectively, against similar flexion force. Therefore, during placement of the implant, damage to the ligament complex and the facet joints should be avoided. This is particularly necessary during placement of a supralaminar hook for making a claw-construct.
(ix)
Cement augmentation to strengthen the cranial-end fixation
In the presence of osteopenia, cement augmentation of the pedicle screw has been a popular method. The disadvantage of cementing the pedicle screw at the top is that it creates a very stiff UIV and may be responsible for fracture and even subluxation at cranial levels, and may lead to spinal cord injury [27]; to avoid such problems some authors advocate the need to cement additional vertebra above the UIV so there is a strong and mobile transition between the instrumented and uninstrumented spine. In a biomechanical study on cadaveric spine, Kebaish et al. [28] reported that prophylactic vertebroplasty at the upper instrumented level and its supra-adjacent vertebra reduced the incidence of junctional fractures after long posterior spinal instrumentation against an axially directed load. Preliminary clinical study was reported by the same group of authors [29] (Fig. 14.7).
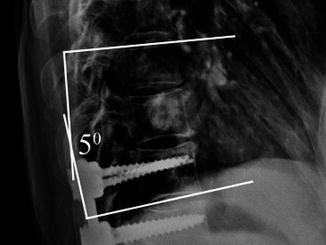
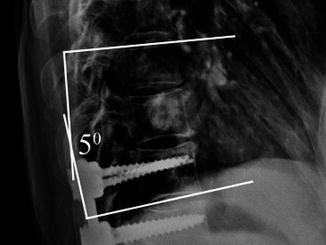
Fig. 14.7
Cement augmentation of the proximal instrumented vertebra and the adjacent cranial segment to prevent PJK (Reproduced with permission from Martin et al. [29])
Authors Preferred Proximal Junctional Fixation Technique
The use of a dynamic stabilization system is still considered experimental. But the present author has achieved reasonable success by using a combination of techniques described above. On the one side the proximal-end fixation is done using a caudally directed pedicle screw. No pedicle screw is inserted on the opposite side at the same vertebra. Instead, a supralaminar hook is inserted on the opposite side at the immediate cranial level, avoiding damage to the ligament complex and facet joints. This hook is used to make a claw-construct with the screw placed at the second caudal vertebra. This reduces the implant density at the proximal end. No compression force is applied at the cranial-end vertebra on either side toward correction of thoracic kyphosis (Fig. 14.5).
A salvage strategy would be to leave a section of the rod beyond the cranial-end anchor fixation (Fig. 14.3). If the patient develops a PJK despite all the above methods, a revision can be easily done by extension of the instrumentation to the upper thoracic spine using simple connectors to the rods left long. However, one disadvantage of leaving extra-length of rod cranially is that when the patient develops a PJK, the rod may project under the skin prominently, risking skin break down.
14.3 Distal Junctional Fixation
The goal of distal junctional fixation is to prevent failure of fixation. DJF is common because of the long lever arm of the fixed spinal segment cranially, together with the body weight, working against the strength of distal-end fixation. The failure may involve either the motion segment or the hardware.
14.3.1 Incidence of DJF
The literature report on the incidence of DJF in adult spinal deformity surgery is sparse, but it is generally believed that the incidence is more frequent compared to pediatric population. In adolescent idiopathic scoliosis, the incidence of DJF is reported as 6.8 %, but the fixation rarely needs to be extended to the sacro-pelvis [30]. In neuromuscular scoliosis the distal fixation is more frequently extended to sacro-pelvis, and the incidence of DJF has been reported to vary widely, between 15 and 44 % [31]. In adult spinal deformity surgery, the distal fixation is frequently required to be extended to the lower lumbar spine or sacro-pelvis, and DJF appears to be common, and the incidence rises with the duration of follow-up. In a retrospective study with 2 year follow-up on 190 patients, the incidence of DJF was reported as 34 % of cases [32]. Major failures included rod breakage between L-4 and S-1, failure of S-1 screws (breakage, halo formation, or pull-out), and prominent iliac screws requiring removal, etc., and were found in 12 % of cases. Minor failures, which did not require revision surgery, included rod breakage between S-1 and iliac screws and failure of iliac screws, and were found in 22 % of cases [32].
14.3.2 Predisposing Factors for DJF
The general risk factors are similar to those for PJF and include old age, increased BMI, osteoporosis, etc. The mechanical risk factors include a large pelvic incidence, large preoperative sagittal imbalance, and failure to restore lumbar lordosis and sagittal balance. Revision deformity surgery also has a higher incidence of DJF because of the weakened posterior elements and/or fatty degeneration of the posterior muscles from previous multiple surgeries.
14.3.3 Mode of DJF
The distal junctional fixation may fail at the distal motion segment, or there may be hardware failure at the distal anchor point.
14.3.4 Distal Motion Segment Failure
This is more common when the fixation ends in the lower lumbar spine or lumbosacral junction.
Progressive kyphoscoliosis, with or without degenerative listhesis and stenosis may occur due to degenerative changes with loss of disc height and facet arthrosis, secondary to excessive stress generated at the motion segment caudal to the instrumentation. A slow progressive degeneration is seen more often in younger adults, with fixation ending at mid or lower lumbar spine. A rapid loss of disc height is more common at the thoracolumbar junction, typically seen in Scheuermann kyphosis, with fixation ending at a segment with preexisting kyphosis. Acute loss of disc height is more typical in adult spine deformity surgery where the fixation is stopped at L5 vertebra, with well-maintained disc height at the lumbosacral junction (Fig. 14.8).
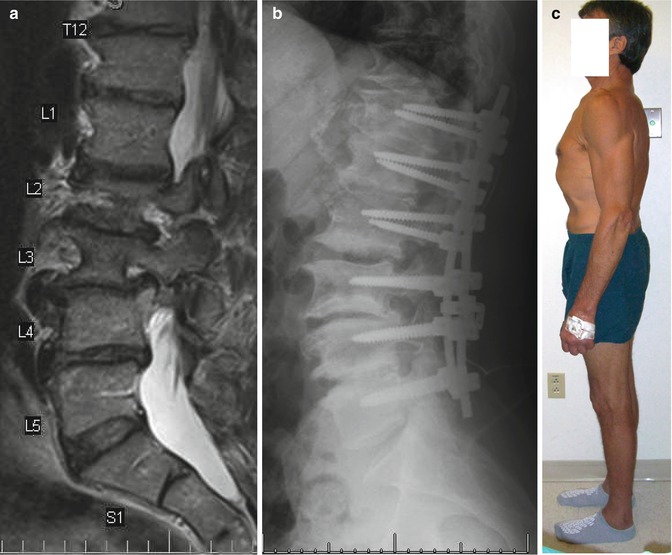

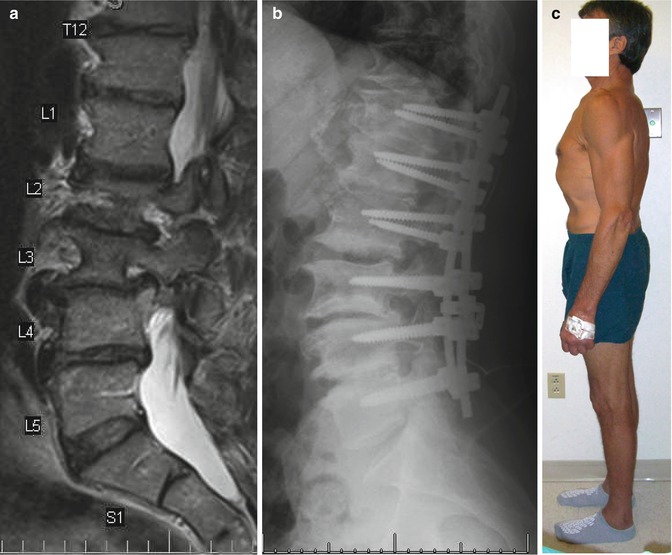

Fig. 14.8




(a) 56 M, Degenerative lumbar scoliosis, with healthy disc at the lumbo sacral junction. T12-L5 fusion with good correction of the deformity (b) and restoration of the sagittal balance (c). In 9 months follow-up, he developed significant degeneration of the L5-S1 disc with complete collapse of the disc height (d, e) and loss of sagittal balance (f) (Reproduced with modification from Sengupta [18])
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








