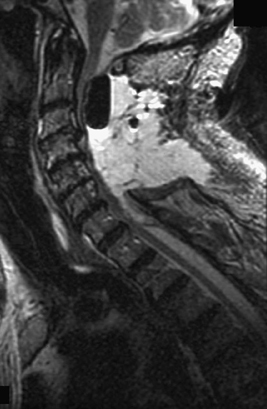
32 An 82-year-old man presents with a cervical pseudomeningocele, discovered 2 years after multilevel posterior cervical laminectomy. Neurologically, he has been stable. He has a significant cardiopulmonary history. A cervical magnetic resonance imaging (MRI) demonstrates postsurgical changes from C2 to C7, as well as a large intradural fluid collection with cerebrospinal fluid (CSF) signal intensity in the operative bed (Fig. 32-1). Iatrogenic pseudomeningocele No treatment is needed. The patient is asymptomatic with an intact wound and stable neurologic status. His surgery was done 2 years ago, and he has significant medical comorbidities. In this case, there is no need for surgical intervention. If he had an active CSF leak or was experiencing cord compression, one might consider further investigation or surgical repair of this likely pseudomeningocele, all the while keeping in mind his medical history. Pseudomeningocele is not an uncommon occurrence following spine surgery in the elderly, particularly in redo cases. The use of power tools, such as the drill, has likely contributed to a higher frequency of this pathology. One needs to take meticulous care with dural closure in case of durotomy, using direct repair, fibrin glue, and a watertight fascial closure. The skin should be closed meticulously, and one may consider using interrupted vertical mattress sutures. The head of the bed should be elevated for the first24 hours in the case of a cervical leak, and flat in the case of a lumbar leak (Figs. 32-2 and 32-3). The wound should be frequently checked, and patients need to be observed for signs of low-pressure headache. MRI and computed tomography (CT) myelogram are the imaging tests of choice. Revision surgery may be required.
Pseudomeningocele
Presentation
Radiologic Findings
Diagnosis
Treatment
Discussion
Pseudomeningocele
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








