|
|
Noradrenergic (NE), γ-aminobutyric acid (GABA), serotoninergic (5-HT), and other neurotransmitter systems have been implicated
Brain areas thought to be involved include limbic system (amygdala), hippocampus, locus ceruleus, and cortical regions
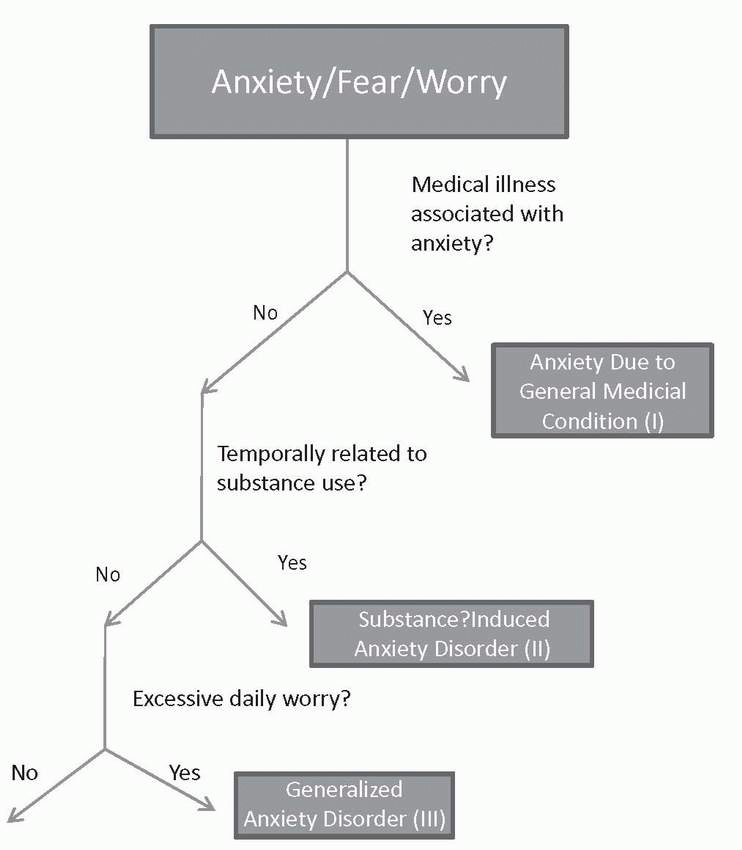
TABLE 3-1 Differential Diagnosis of Anxiety | |||||
|---|---|---|---|---|---|
|
Onset after age 35 years
No personal or family history of anxiety disorder
No childhood history of debilitating anxiety, separation anxiety, or phobias
Lack of significant life events leading to or exacerbating anxiety symptoms
Lack of avoidance behavior
Poor response to anxiolytic medications
TABLE 3-2 Approach to the Evaluation of Anxiety | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Prominent generalized anxiety, panic attacks, or obsessive-compulsive disorder (OCD) in the setting of substance intoxication or withdrawal
Need confirmation from clinical history, laboratory results, or physical examination that either:
Anxiety developed during or within 1 month of substance intoxication or withdrawal
Substance use is etiologically related to anxiety symptoms
Not occurring exclusively during delirium
Diagnosis should only be made if anxiety exceeds symptoms usually seen in substance intoxication or withdrawal
The person has chronic, excessive worry or anxiety that occurs most days for at least 6 months
It is associated with somatic symptoms, including fatigue, muscle tension, restlessness, sleep disturbance, difficulty concentrating, and irritability
Anxiety is hard to control and causes significant impairment
The person is seen as chronic “worrier” or “nervous person” by others around him or her
3%-8% prevalence rate
2:1 female-to-male ratio
50%-90% have comorbid psychiatric illness
Development of nervousness or worry occurring within 3 months of onset of psychosocial stressor
Remits within 6 months after termination of stressor
Not attributable to bereavement
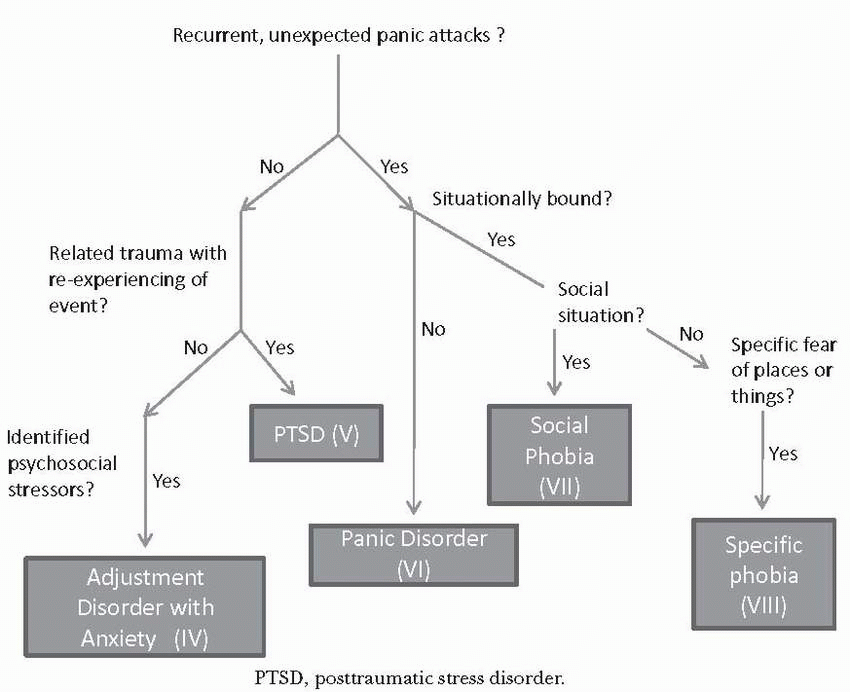
Intense fear, horror, and helplessness experienced after a traumatic event
Trauma was such that patient directly witnessed, experienced, or was confronted with an event that involved actual or threatened death, injury, or threat to physical integrity
Persistent reexperiencing of the event through distressing recollections, dreams, dissociative flashbacks, physiological reactivity, and psychological distress to stimulus cues of event
Persistent avoidance of stimuli associated with the traumatic event and numbing of general responsiveness (e.g., detachment or sense of estrangement)
Symptoms of hyperarousal are present, including:
Difficulty falling or staying asleep
Irritability or angry outbursts
Difficulty concentrating
Hypervigilance
Exaggerated startle response
Symptoms present for more than 1 month (for symptoms <1 month, consider acute stress disorder)
Recurrent, unexpected panic attacks
Symptoms of panic attacks: overwhelming anxiety or fear that comes on acutely (<10 min) and is accompanied by four or more of the symptoms below:
Chest pain
Palpitations
Derealization or depersonalization
Fear of dying, losing control, or losing one’s mind
Paresthesias
Dizziness or lightheadedness
Shortness of breath
Many individuals may experience limited symptom attacks (e.g., only experiencing one or two of panic symptoms)
Attacks come on suddenly and peak within 10 minutes
Accompanied by more than 1 month of more than one of following:
Anticipatory anxiety (so-called “fear of the fear”)
Corresponding change in behavior (e.g., avoidance)
Worrying about consequences or outcomes of panic attacks
May occur with or without agoraphobia
Agoraphobia
Anxiety caused by being in places or situations from which escape may be difficult or embarrassing or from which help may not be readily available in case of a panic attack
Typically involves clusters of situations outside the home, including being in a crowd; standing in line; being on a bridge; or traveling in a bus, train, or automobile
Situations are avoided or endured with marked distress or anxiety about having panic
The first panic attack must occur unexpectedly (e.g., uncued)
The person may become phobic of particular situation in which panic occurred, but anxiety is from fear of another panic attack. not the situation itself
3% of the general population
Female > male
Average age of onset: 24 years
Potentially increased rate of suicidal ideation and attempts
Excessive anxiety or fear triggered by social situations causing marked impairment
Fear of being publicly scrutinized or humiliated
Panic attacks are a common feature
The patient recognizes that fear is excessive or irrational
The phobic stimulus is avoided or lived through with significant anxiety
Should specify if subtype “performance anxiety” is present
3%-15% prevalence rate
Onset peaks in adolescence
Often comorbid with depression and substance abuse
Irrational, overwhelming fear of a specific situation or object
Fear is recognized as irrational
Avoidance of phobic stimulus is common
Exposure to phobic stimulus can trigger panic attacks
Causes marked impairment
Types of phobias include animals (dogs), natural environment (heights), blood injection, situational (airplanes), and other (fear of choking)
5%-10% of US population
Most common psychiatric disorder among women; second among men
Bimodal distribution of situational phobias: childhood and early adulthood
Start slow: patients with anxiety are very sensitive to somatic side effects
Selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) are first-line agents for most of the disorders
Antidepressant doses used for depression may need to be higher
Older agents such as tricyclic antidepressants (TCAs) and monoamine oxidase inhibitors (MAOIs) are effective but typically have more side effects
TCAs are not effective for social anxiety disorder
Benzodiazepine are efficacious, fast-acting, and generally well tolerated but have abuse liability
There is a potential concern that benzodiazepines administered in aftermath of trauma may interfere with recovery after trauma
Beta-blockers are sometimes used to reduce autonomic arousal in patients with panic attacks
Beta-blockers are helpful in reducing the performance anxiety subtype but not the generalized subtype of social phobia
Anxiety disorders are effectively treated by many forms of psychotherapy, especially cognitive behavior therapy (CBT)
Cognitive restructuring: restructures catastrophic thinking
Relaxation training: anxiety management strategies
Slow breathing
Muscle relaxation
Behavioral exposure: repeatedly exposing the patient to fearful stimuli to extinguish the conditioned fear response
Supportive therapy is particularly helpful for acute management immediately after the trauma of PTSD
Problems with information recall or learning
One or more of the following problems with cognition:
Aphasia (problems with language)
Agnosia (difficulty recognizing objects)
Apraxia (difficulty executing voluntary movements without motor impairment)
Executive functioning problems (poor planning, abstract reasoning)
May also be associated with:
Poor judgment; disinhibition; hallucinations; delusions; anxiety, mood, or sleep disturbance
TABLE 3-3 Dementia Diagnosis Categories and Representative Examples | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3-4 Clinical Features of Delirium, Depression, and Alzheimer’s Dementia | ||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||
Safety of the patient and others takes priority. Use physical restraints or one-on-one supervision when necessary
Consider behavioral interventions
Reorient to environment
Simplify communication
Reassure, distract, and redirect
Identify if delirium is also present
Minimize polypharmacy
Identify and avoid drugs with cognitive side effects
Assess for and treat comorbid medical problems, especially delirium
Start with low doses (one quarter to one half that for normal adults) and increase slowly while monitoring for side effects
Older patients may be more sensitive to medication side effects such as sedation, orthostatic hypotension, anticholinergic side effects, and extrapyramidal side effects (EPS)
No pharmacologic treatment exists for wandering behavior
TABLE 3-5 Approach to the Evaluation of Dementia | ||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 3-6 Dementia Subtypes | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
TABLE 3-7 Suggested Pharmacologic and Somatic Treatments for Symptoms Occurring with Dementia | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
Hallucinations, paranoia, and delusions may not require treatment unless they are causing great distress to the patient or potential harm to others
When using atypical antipsychotics, consider the risk-benefit ratio for each patient and talk with patients and their families about the Food and Drug Administration (FDA) black box warning regarding a possible increased risk of death from medication use
Patients with dementia with Lewy bodies (which often co-occurs with Alzheimer’s dementia) are often very sensitive to antipsychotics. (Recall that antipsychotics may cause akathisia and agitation)
TABLE 3-8 Differential Diagnosis of Depression | ||||||
|---|---|---|---|---|---|---|
| ||||||
MDE is defined by five or more of the following symptoms, one of which must be depressed mood or anhedonia. All symptoms must occur in the same 2-week period, be present a minimum of most of the day on most days, and result in clinically significant social, occupation, or interpersonal impairment
Depressed mood
Profound loss of interest or pleasure in all or almost all activities (anhedonia)
Profound increase (atypical feature) or decrease in appetite
Insomnia or hypersomnia (atypical feature)
Objective psychomotor hyperactivity or retardation
Decreased energy
Indecisiveness or decreased concentration
Worthlessness or guilt
Recurrent thoughts of death, recurrent suicidal ideation (SI) without a plan, SI with a plan, or suicide attempt (SA)
TABLE 3-9 Approach to the Evaluation of Depression | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Presence of at least one depressive episode
Rule out a history of manic, mixed, or hypomanic episodes; psychotic disorder; and delusional disorder
Modifiers include:
For active MDE: mild, moderate, severe with or without psychotic, melancholic, atypical, or postpartum features
If full criteria for MDE are not present: partial vs. full remission with or without psychotic, melancholic, atypical, or postpartum features
Two thirds of people with MDE contemplate suicide; 10% to 15% commit suicide
There is a 50% recurrence rate after the first episode, a 70% recurrence rate after the second episode, and a 90% recurrence after the third episode
Lifetime risk: women: 20%-25%; men 7%-12%
No socioeconomic or racial correlation
Increased in single people
Circumstances that may increase risk: being single, living in a rural area, divorced, losing a parent before age 11 years, experiencing the death of spouse, unemployment
Defined by depressed mood most of the day for more days than not for 2 years with symptom-free periods not exceeding 2 months during the 2-year period
While the patient is depressed, two of the following must be present:
Increased or decreased appetite
Insomnia or hypersomnia
Fatigue or low energy
Low self-esteem
Indecisiveness or decreased concentration
Hopelessness
Depression resulting in significant clinical impairment but not meeting the criteria for major depression
Occurs within 3 months of a stressful life event and does not persist longer than 6 months after termination of the stressor
Depressive symptoms occurring within 2 months of the death of a loved one are considered normal grief
Certain symptoms after the death may be associated with MDD:
Guilt (not including guilt regarding actions taken or not taken by survivor at the time of death)
Thoughts of death (not including patient feeling he or she would be better off dead or should have died with the deceased person)
Morbid preoccupation with worthlessness
Marked psychomotor retardation
Substantial, prolonged functional impairment
Hallucinations (not including transient seeing or hearing of the deceased person)
There is a 40% remission rate with an adequate single trial with an antidepressant; the majority of the rest of patients show some improvement, but 15% to 30% of patients do not improve after a single adequate trial
The most common reasons for failure are inadequate dosing and inadequate duration
Suggested pharmacotherapy guidelines:
No single antidepressant is universally accepted as more effective than another
Therapy should be chosen based on side effects, drug interactions, dosing schedule, discontinuation symptoms, cost of treatment, and history of effective response (including history of response in a first-degree relative)
Before declaring treatment failure, ensure maximum titration and minimum of 4 to 6 weeks of treatment after achieving the maximum dose (full response is gauged at 8-12 weeks)
Duration of treatment for depression maintenance:
Single episode: treat for a minimum of 6 months after resolution of symptoms or for the length of previous depressive episode, whichever is longer
Multiple episodes: indefinite maintenance
Addressing inadequate treatment response (treatment failure or partial response, defined as a 20% to 25% reduction in depressive symptoms):
Ensure proper dosing and duration of medication
Consider the accuracy of the diagnosis
If there is no response, switch the class of medication
If there is a less than desired response: augmentation with lithium or thyroid hormone (T3)
TABLE 3-10 Suggested Treatment by Depressive Subtype | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||
TABLE 3-11 Differential Diagnosis of Disordered Eating Behaviors | ||||||
|---|---|---|---|---|---|---|
|
Significantly low weight (≥15% below expected body weight) in combination with resistance to weight gain, often motivated by excessive concern with thinness or control overeating
Low weight is maintained by dietary restriction but is frequently accompanied by purging and exercise (see Bulimia nervosa)
Lifetime prevalence: 0.9% in women; 0.3% in men
Characterized by regular episodes of binge eating followed by a variety of purging, exercise, and dietary behaviors to prevent weight gain
Lifetime prevalence: 1.0%-1.5% in women
TABLE 3-12 Approach to the Evaluation of Disordered Eating | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Aberrant eating patterns and weight management habits not meeting criteria for AN or BN
The most common presentation of eating disorders
Occurs in 3% to 5% of women age 15 to 30 years
Episodic binge eating without purging, exercise, and dietary behaviors to prevent weight gain
Eating not linked to cues (social, hunger, satiety) that conventionally drive eating
Episodes may be associated with distress and other negative affect
At least three of the following must be present:
Eating more rapidly than normal
Eating until feeling uncomfortably full
Eating large amounts of food when not feeling hungry
Eating alone because of embarrassment of how much one is eating
Feeling disgusted with oneself, depressed, or guilty of overeating
Lifetime prevalence: 3.5% in women; 2% in men
Evaluate the patient’s medical and nutritional compromise
Treat the medical sequelae of undernutrition, purging behaviors, and obesity
Watch for refeeding syndrome caused by low phosphorous (gastric bloating, congestive heart failure (CHF), edema; can lead to respiratory failure, coma, seizures, or death)
Surveillance for and treatment of common and life-threatening complications, such as medical sequela of BN (tooth enamel decay, esophagitis, blistered knuckles) or emergencies such as arrhythmias or hematemesis
Management of obesity-related complications in patients with BED (diabetes, sleep apnea, dyslipidemia, cardiovascular disease)
Determine energy and micronutrient deficits and protocol for nutritional rehabilitation
The patient may safely gain 0.5 to 2.0 lb per week as an outpatient or up to 3 to 4 lb as an inpatient
Provide vitamin supplementation
Section 12 criteria for admission to inpatient psychiatric facility after medical stabilization: the patient must demonstrate him- or herself to be unable to care for him- or herself, as evidenced by weight below 75% of ideal body weight, electrolyte disturbance (K <3.2), electrocardiographic changes, abnormal vital signs (i.e., bradycardia, low blood pressure, significant orthostatic changes, hypothermia), or indications of suicidality
Patients under 20% of expected weight for their height should be enrolled in inpatient programs
Treatment initially supports nutritional goals and medical and psychiatric stabilization
Family therapy is the treatment of choice for adolescents with AN
CBT and interpersonal therapy (IPT) have been demonstrated effective for BN
Treat common comorbid psychiatric conditions, such as depression and anxiety
Medications that modify appetite: mirtazapine: increase appetite; topiramate: decrease appetite; Meridia: appetite suppressant
Monitor for potential weight gain as a medication side effect (i.e., with atypical antipsychotics)
There are no FDA-approved medications for the treatment of AN
Fluoxetine is FDA approved for treatment of BN (higher dosing, 60-80 mg)
Antidepressant use should not be initiated until weight gain has been achieved because side effects can be more severe in malnourished patients
Bupropion is contraindicated in patients with BN because of an increased risk of seizures
Some data suggest that atypical antipsychotics may have benefits for some AN patients, but this use is off label and has no established efficacy
Use with caution because of the risk for idiopathic and hypokalemiarelated QT prolongation
Antiepileptics have shown some effectiveness anecdotally in patients with BED
Zinc (50-100 mg) has been shown to more rapidly improve weight restoration in patients with AN
primary defense and occur chronically in response to reminders of the original traumatic event or even to relatively minor stressors of everyday living (Howell, 2005).
Daydreaming
Becoming absorbed in a movie or a book
Meditation
“Highway hypnosis” (e.g., being briefly lost in a trance while driving)
Fantasy
Formal or self-induced hypnotic state
Numbing: feeling detached from one’s emotions
Flashback: intrusive immersion in sensory components of a past traumatic experience
Depersonalization: feeling detached from one’s self or looking at one’s self as an outsider would
Derealization: feeling detached from one’s environment or a sense that the environment is unreal or foreign
Amnesia: inability to account for a specific and significant block of time that has passed
Identity confusion: feeling uncertain, puzzled, or conflicted about who one is
Identity alteration: shifting of one’s role or identity, accompanied by changes in behavior
TABLE 3-13 Differential Diagnosis of Dissociative Experiences | |||||||
|---|---|---|---|---|---|---|---|
|
TABLE 3-14 Approach to the Evaluation of Dissociation | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Requires experience of a traumatic event, occurrence of three to five dissociative symptoms, one reexperiencing symptoms, and marked avoidance and arousal at the time of or shortly after the event
Occurs within 1 month of the traumatic event and persists for at least 2 days
Recognizes dissociative symptoms as frequent sequelae to traumatic exposure
See page 56 for more information
Requires experience of a traumatic stressor, occurrence of one reexperiencing symptom, three avoidance symptoms, and two arousal symptoms for duration of more than 1 month after the event
Does not require dissociative symptoms for diagnosis; however, several dissociative symptoms fall under PTSD diagnostic criteria, including flashbacks, numbing, detachment, restricted affect or absence of emotional responsiveness, and amnesia
One or multiple episodes of memory loss typified by inability to recall important personal information (e.g., one’s identity or significant elements of one’s past)
Occasionally seen in adult-onset traumatic events
The unrecalled personal information is often of a stressful or traumatic nature
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree