Chapter 3 Psychogenic Neurologic Deficits
The Neurologists’ Role
Within the framework of this potential oversimplification, neurologists reliably diagnose psychogenic nonepileptic seizures (PNES) (see Chapter 10), diplopia and other visual problems (see Chapter 12), and tremors and other movement disorders (see Chapter 18). In addition, they acknowledge the psychogenic aspects of headache (see Chapter 9), pain (see Chapter 14), sexual dysfunction (see Chapter 16), posttraumatic headaches and whiplash injuries (see Chapter 22), and many other neurologic disorders.
Patients often have mixtures of neurologic and psychogenic deficits, disproportionately severe posttraumatic disabilities, and minor neurologic illnesses that preoccupy them. As long as serious, progressive physical illness has been excluded, physicians can consider some symptoms to be chronic illnesses. For example, chronic low back pain can be treated as a “pain syndrome” with empiric combinations of antidepressant medications, analgesics, rehabilitation, and psychotherapy, without expecting either to cure the pain or determine its exact cause (see Chapter 14).
Psychogenic Signs
What general clues prompt a neurologist to suspect a psychogenic disturbance? When a deficit violates the laws of neuroanatomy, neurologists almost always deduce that it has a psychogenic origin. For example, if temperature sensation is preserved but pain perception is “lost,” the deficit is nonanatomic and therefore likely to be psychogenic. Likewise, tunnel vision, which clearly violates these laws, is a classic psychogenic disturbance (see Fig. 12-8). The caveat is that migraine sufferers sometimes experience tunnel vision as an aura (see Chapter 9).
Motor Signs
Deficits that are intermittent also suggest a psychogenic origin. For example, a “give-way” effort, in which the patient offers a brief (several seconds) exertion before returning to an apparent paretic position, indicates an intermittent condition that is probably psychogenic. Similarly, the face–hand test, in which the patient momentarily exerts sufficient strength to deflect her falling hand from hitting her own face (Fig. 3-1), also indicates a psychogenic paresis.

FIGURE 3-1 In the face–hand test, a young woman with psychogenic right hemiparesis inadvertently demonstrates her preserved strength by deflecting her falling “paretic” arm from striking her face as the examiner drops it.
Another indication of unilateral psychogenic leg weakness is Hoover sign (Fig. 3-2). Normally, when someone attempts to raise a genuinely paretic leg, the other leg presses down. The examiner can feel the downward force at the patient’s normal heel and can use the straightened leg, as a lever, to raise the entire leg and lower body. In contrast, Hoover sign consists of the patient unconsciously pressing down with a “paretic” leg when attempting to raise the unaffected leg and failing to press down with the unaffected leg when attempting to raise the “paretic” leg.
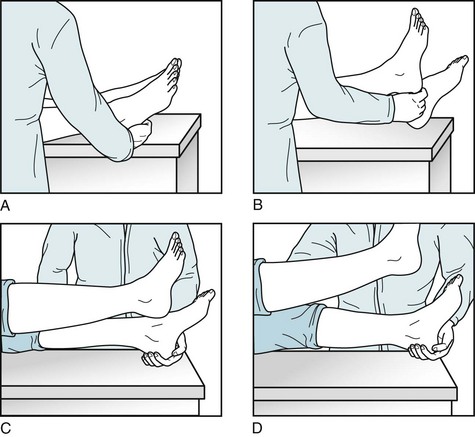
FIGURE 3-2 A neurologist demonstrates Hoover sign in a 23-year-old man who has a psychogenic left hemiparesis. A, She asks him to raise his left leg as she holds her hand under his right heel. B, Revealing his lack of effort, the patient exerts so little downward force with his right leg that she easily raises it. C, When she asks him to raise his right leg while cupping his left heel, the patient reveals his intact strength as he unconsciously forces his left “paretic” leg downward. D, As if to carry the example to the extreme, the patient forces his left leg downward with enough force to allow her to use his left leg as a lever to raise his lower torso.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








