Fig. 11.1
A 37-year-old male presents with fever, expressive aphasia, and altered mental status. (a) CT brain shows subcortical white matter hypodensities involving the anterior frontal lobes. Brain MRI: (b) axial T2, (c) FLAIR, and (d) enhanced T1-weighted images demonstrate sheetlike area of high T2 signal in the subcortical white matter of the anterior frontal lobes. There is no evidence of abnormal parenchymal or meningeal enhancement following contrast administration (d). DSA was performed to rule out vasculitis and was normal (not shown here). (e) Follow-up MRI: axial FLAIR, 5 months after treatment, demonstrates complete resolution of the previous abnormal signal in the subcortical white matter
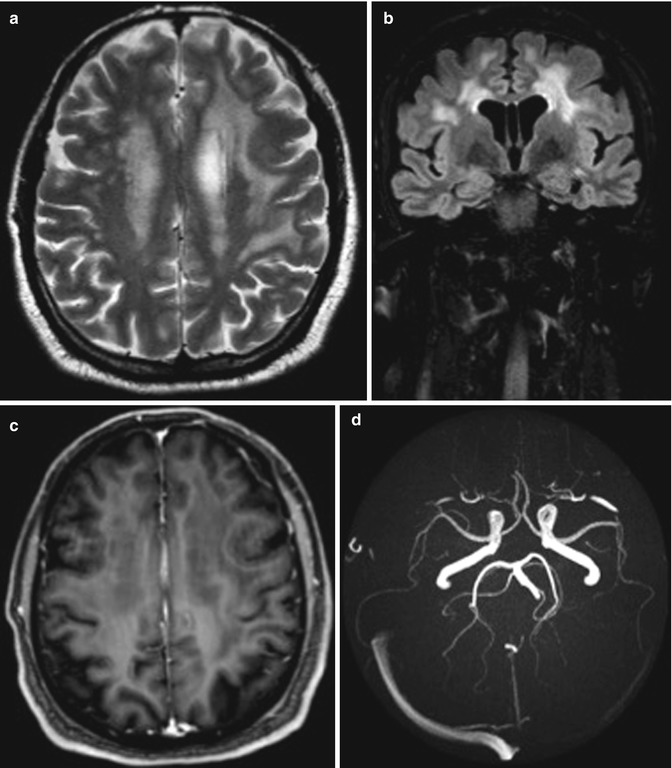
Fig. 11.2
A 55-year-old male previously healthy, presenting with right-sided acute transient numbness. Brain MRI: (a) axial T2 and (b) coronal FLAIR images of the brain show extensive abnormal high signal intensity lesions in the cerebral white matter predominately subcortical involving the U-fibers (arrow) (a) as well as the centrum semiovale. (c) Axial T1 after gadolinium administration: These lesions show no enhancement after contrast administration. (d) Brain MRA shows normal intracranial vessels with no evidence of significant obstructive pathology or aneurysmal formation
11.2.4 Vascular Lesions
Vasculopathic change owing to brucellosis is a very rare entity. Although rare, it is well known that Brucella can cause vasculitis of the cerebral vasculature with no predilection to size or location of vessels. Brucellosis can also cause deep venous thrombosis probably through an immune mechanism causing pseudotumor cerebri-like symptoms [1].
Ischemic stroke and transient ischemic attacks may be observed in CNS brucellosis. The pathogenesis may be caused by cerebral vasospasm, infectious vasculitis, or embolism. There are two types of cerebrovascular involvement in brucellosis, the first being mycotic aneurysm that can rupture with secondary subarachnoid hemorrhage. The second mechanism is inflammation of the vessels causing arteritis with subsequent infarcts, hemorrhage, or venous thrombosis. The mycotic aneurysm is most likely secondary to embolus from Brucella endocarditis [9].
CT scan may demonstrate intraparenchymal hemorrhage and perivascular enhancement after contrast material administration. MRI is superior in showing acute lacunar infarcts. FLAIR- and T2-weighted images reveal multiple hyperintense foci in the white matter compatible with vasculitis. Diffusion-weighted imaging is useful in acute ischemia where it shows restricted diffusion in acute infarct. The lacunar infarcts are mainly seen in the distribution of perforating vessels in the basal ganglia, brainstem, and the white matter of the brain. On the other hand, magnetic resonance angiography and digital subtraction angiography (DSA) may be normal, but DSA is superior in resolution and can demonstrate stenosis, occlusion of intracranial vessels, or vascular wall irregularities.
In patients with venous thrombosis, CT shows venous infarct as cortical and subcortical hypodensity in a venous territory with or without hemorrhage. On MRI, venous infarct appears as subcortical high T2 signal with mild mass effect. The diffusion is heterogeneous, most of the time not reduced. In some cases, there is small hemorrhage or hematoma. As a rule, MRI and CT venography are reliable techniques to make the diagnosis of venous sinus thrombosis. In the acute phase, the thrombus appears hyperdense on non-enhanced CT scan. In the subacute and acute phases, CT with contrast shows the filling defect within the sinus. On MRI, in the acute phase, the thrombus is hypointense on T2 and isointense on T1 and may be missed. Magnetic resonance venography 2D phase contrast can demonstrate the filling defect and make the diagnosis; when the thrombus is subacute, it appears hyperintense on T1 and T2 and it is easy to identify [4, 6, 10].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








