16Radiology
A Radiation necrosis
Radiation necrosis typically presents with higher apparent diffusion coefficient (ADC) values compared with tumor recurrence, which tends to show restricted diffusion and therefore lower signal in the solid enhancing components. On perfusion MRI, radiation necrosis demonstrates decreased relative cerebral blood volume (rCBV) in contrast to high-grade tumors. Finally, this patient is 1 year from his radiation therapy, which is a peak time for radiation necrosis to appear (usually between 12 and 24 months). (B) A recurrent glioblastoma would tend to have a low ADC signal and increased perfusion on rCBV maps. (C) Secondary malignancies following temozolomide (an alkylating agent) have been reported but are a rare occurrence. These malignancies usually are hematologic. Glioblastoma would be much more likely than a secondary malignancy, given its aggressive nature and expected eventual recurrence. (D) Encephalomalacia would be apparent by parenchymal volume loss and should not show nodular enhancement or restricted diffusion. Some (usually nonnodular) enhancement may be present around the resection cavity due to granulation tissue.
D Esthesioneuroblastoma
Esthesioneuroblastomas (olfactory neuroblastomas) are rare, malignant tumors of the superior nasal cavity and anterior skull base. Treatment strategies vary widely and include surgery, radiotherapy, and/or chemotherapy. The ideal treatment modality has yet to be determined. Esthesioneuroblastomas tend to exert mass effect on the orbits, optic nerves, and optic chiasm, and may result in proptosis. They can occur in the frontal sinus and have variable intracranial extension. They homogeneously enhance on contrasted T1 sequences and appear moderately hyperintense on T2 sequences. (A) An optic nerve glioma would infiltrate and expand the optic nerve. As seen in the second image, there is stretching of the optic nerve due to mass effect and proptosis, but the tumor itself does not involve the optic apparatus. (B) Anterior skull base meningiomas also demonstrate avid enhancement and occasionally can extend into the olfactory recess. They may present with a dural tail and hyperostosis; however, the epicenter of the mass in this case is in the sinonasal cavity without a significant intracranial dural component. This makes a meningioma unlikely. Esthesioneuroblastomas often do extend intracranially, in which case a “waist” at the level of the cribriform plate and cysts at the brain–tumor interface are strongly suggestive of such diagnosis. (C) Skull base chordo-mas usually are located in the anterior clivus but rarely may extend to the nasal cavity. Primary chordomas in the nasal cavity and maxilla without clival involvement are extremely rare. Chordomas usually demonstrate more heterogeneous enhancement than esthesioneuroblastomas on contrasted T1 sequences and are very hyperintense on T2 sequences.
D Long bone fractures
Long bone fractures can result in fat embolism, which appears as tiny foci of susceptibility artifact that preferentially may be located at the gray matter–white matter interface or diffusely distributed as in this case. Fat embolism may be accompanied by scattered foci of restricted diffusion. (A) Diffuse axonal injury is due to shearing forces from rotational acceleration. Areas of hemorrhage can be detected on susceptibility-weighted imaging (SWI) sequences and tend to be located in the gray matter-white matter junction, corpus callosum, and brainstem. Linear SWI signal loss often can be seen along the white matter tracts. (B) β-amyloid peptide deposits are related to cerebral amyloid angiopathy (CAA). SWI may show multiple foci of signal loss located peripherally in a cortical/subcortical distribution rather than diffusely as in this case. Patients also can have superficial siderosis and present with subarachnoid hemorrhage. (C) Mutations in the CCM1, CCM2, and CCM3 genes can be seen in familial cavernous malformation syndromes. Lesions usually are more randomly distributed and not as evenly sized as in the current case.
A Astrocytoma
Astrocytomas in the spinal cord are most common in children but also may occur in adults. The majority of them are histologically low grade and slow growing, and may result in bone remodeling. Half of astrocytomas are of the pilocytic subtype and are relatively well defined, whereas the remainder are infiltrative. They commonly present as expansile masses with variable degrees of ill-defined enhancement, although some tumors may not enhance. (B) Ependymomas are more common in adults. Compared with astrocytomas, their enhancement more frequently is well defined, and they more commonly are associated with cystic changes or hemorrhage. They are located more centrally, as they arise from the ependyma, but such distinction becomes difficult in larger tumors. (C) Metastases to the cervical spine typically are more focal than and not as expansile as the demonstrated lesion. It would be highly unusual for a patient of this age to present with a spinal cord metastasis without a known primary malignancy. (D) Tumefactive demyelination is more common in the brain. Demyelinating lesions may be seen in the spinal cord and may be related to acute disseminated encephalomyelitis (more common in the cervical spine), neuromyelitis optica (which may result in longitudinally extensive transverse myelitis), and multiple sclerosis (usually with small lesions centered in the peripheral white matter and only rarely extending over long segments when confluent). The appearance of the lesion in question is too expansile and is not compatible with a demyelinating or inflammatory process.
A Interhemispheric cysts
The image accompanying the question shows dysgenesis of the corpus callosum with incomplete formation of the cingulate gyrus. Dorsal or occasionally anterior interhemispheric cysts are a common finding. (B) Colpocephaly (dilatation of the atria and occipital horns of the lateral ventricles) is a characteristic secondary finding in dysgenesis of the corpus callosum. (C) Patients with dysgenesis of the corpus callosum can have a “high-riding” third ventricle. Additional findings include bundles of Probst (white matter that failed to cross the midline) and incomplete rotation of the hippocampi. (D) Tubulonodular lipomas have a significantly increased incidence of associated anomalies compared with curvilinear ones.
A Results from premature disjunction of the cutaneous ectoderm from the neuroectoderm during neurulation
Postcontrast sagittal T1 and short tau inversion recovery (STIR) images show a large lobulated mass that appears to be intradural and at least partially intramedullary. Although most of the mass is hyperintense on T1, these areas fully suppress on STIR images, indicating that this signal is related to fat rather than contrast enhancement. Spinal lipomas follow fat signal on all sequences, and subcutaneous fat can be used as an internal control. Embryologically, these lesions result from premature disjunction of the cutaneous ectoderm from the neuroectoderm during neurulation, whereby the open neural tube becomes exposed to the ingrowth of mesodermal tissues. Patients may experience slowly progressing paresis, spasticity, or sensory loss depending on the extent and location of the lesion. (B) An infiltrative hypercellular lesion with variable degrees of mitosis/atypia would describe a neoplastic process such as an astrocytoma, which may or may not show enhancement. (C) Clonal transformation of cells of B-cell origin would result in lymphoma (e.g., Hodgkin). These lesions are rare in the spinal cord and usually enhance. (D) Hemangioblastomas are very vascular and avidly enhance. They can occur in the spinal cord or leptomeninges. They may be associated with endolymphatic sac tumors, renal cell carcinomas, retinal angiomas, pheochromocytomas, and cystic lesions.
A Enhancing lesion involving the brainstem
Manifestations of Behçet disease in the central nervous system are varied. The brainstem is the most commonly affected, and lesions can be focal or multifocal. There usually is associated edema and contrast enhancement, particularly in the acute phase. Patients also can present with meningoencephalitis and nonspecific white matter lesions. (B) T2/FLAIR hyperintensity in the brainstem sparing the red nuclei and substantia nigra commonly is described in Wilson disease. (C) A leading edge of restricted diffusion can be seen in large or new lesions in progressive multifocal leukoencephalopathy. (D) Lesions involving the pulvinar and dorsomedial thalamic nuclei are characteristic of variant Creutzfeldt-Jakob disease. (E) Active demyelination can present with an incomplete rim of enhancement.
D Meningioma
The demonstrated homogeneously enhancing dural-based mass along the left ventral aspect of the spinal canal at the level of C2 is most consistent with a meningioma. It is more common in females and, when in the spine, it most frequently occurs in the thoracic region. It nearly always is completely intradural, but also may protrude through the neural foramina, resulting in a “dumbbell” configuration and thus may look similar to schwannomas. (A) Leptomeningeal metastases usually develop along the pial surface of the cord and spinal nerves. The lesion in question is dural based. (B) Neurofibromas may be indistinguishable from schwannomas by imaging. They may show a so-called target sign with central hypointensity on T2-weighted sequences due to a fibrocollagenous core. (C) Schwannomas tend to enhance more avidly and heterogeneously than meningiomas, particularly due to the presence of cystic changes and hemorrhages in larger lesions. They follow the course of the involved nerve and do not show a dural base. Although not entirely specific, they can extrude through and expand the neural foramina, resulting in a “dumbbell” configuration.
A Central tegmental tract
The axial FLAIR image accompanying the question demonstrates hyperintensity of the left inferior olivary nucleus in a patient with hypertrophic olivary degeneration. This can be caused by a lesion involving the triangle of Guillain-Mollaret, a circuit connecting the dentate, red, and inferior olivary nuclei. Efferent fibers from the dentate nucleus ascend via the superior cerebellar peduncle and decussate to the contralateral red nucleus, from which fibers project inferiorly to the ipsilateral inferior olivary nucleus through the central tegmental tract. Patients characteristically present with palatal tremors. (B) The lateral lemniscus is not part of the Guillain-Mollaret triangle. Bilateral lesions are associated with hearing loss. (C) The spinothalamic tract is a sensory pathway that transmits pain and temperature sensation from the spinal cord to the thalami. (D) The reticulospinal tract transmits information from the reticular formation in the pons and medulla to the spinal cord. It is not part of the Guillain-Mollaret triangle.
B Epidural scar
The axial T2 images accompanying the question show hypointense tissue projecting into the right paracentral zone. This tissue shows diffuse enhancement on the postcontrast image, and therefore is most consistent with scar. Note the evidence of a prior right-sided laminotomy. (A, C, E) A disk protrusion or extrusion or a sequestered disk should not enhance. (D) There is no fluid collection with peripheral enhancement to suggest an epidural abscess.
B Deep venous thrombosis
The sagittal noncontrast T1-weighted image (right) accompanying the question shows increased signal in the straight sinus, vein of Galen, and internal cerebral veins due to thrombosis. Also note the profound hypointensity of the thalami compared with the brain. The axial FLAIR image (left) shows marked swelling of the basal ganglia and thalami bilaterally due to venous infarction. Risk factors for deep venous thrombosis include severe dehydration and other hypercoagulable states such as pregnancy, malignancy, and sepsis. Venous infarction occurs in a nonarterial distribution and may be complicated by hemorrhage. (A) Cortical venous thrombosis may lead to lobar infarctions sparing the deep gray structures. (C) Leigh disease is a mitochondrial encephalopathy that may affect the basal ganglia, periaqueductal gray, and cerebral peduncles. Changes in the putamina seem to be a consistent feature. (D) Hypoxic ischemic encephalopathy can occur following hypoxia, such as in cardiorespiratory arrest, drowning, or various forms of asphyxiation. In older children and adults, the watershed zones initially may be affected after mild insults, with more severe cases involving gray matter structures, particularly the cerebral cortex, basal ganglia, and hippocampi. Perinatal hypoxic ischemic injury preferentially may affect the thal-ami, brainstem, and perirolandic cortex. There may be white matter involvement in the setting of global ischemia. (E) The imaging abnormalities in this case do not follow an arterial distribution.
C Intracranial hemorrhage
There is a hemispheric subdural hematoma along the right convexity that is isodense to the cortex. This appearance can occur depending on when the patient is imaged, as the density of blood decreases over time and, at some point, will have the same attenuation as cortex. The best way to recognize such hematomas is to identify their associated mass effect and the displacement of the darker white matter, which can be seen medial to the hematoma. (A) An infiltrative tumor would involve the cortex and white matter more diffusely. The demonstrated process is centered in the extra-axial space and is subdural due to its overall crescentic shape and the fact that it crosses sutures. (B) A noncon-trast head CT in acute infarct may be normal, particularly in the first 6 hours after ictus. Early findings include a hyperdense middle cerebral artery territory, loss of gray matter-white matter distinction in the basal ganglia or peripheral brain, and loss of the insular ribbon. (D) The majority of noncontrast head CT studies in meningitis are normal, and patients sometimes may present with hydrocephalus as an isolated finding. Areas of edema due to cerebritis or intra- and extra-axial abscesses may be seen in complicated meningitis. Contrast studies, in particular MRI, may be able to show the presence of leptomeningeal disease.
B Rhombencephalosynapsis
Rhombencephalosynapsis is characterized by an absent vermis and midline continuation of the dentate nuclei, cerebellar hemispheres, and superior cerebellar peduncles. It can be seen in isolation or associated with other malformations such as the VACTERL spectrum and Gomez-Lopez-Hernandez syndrome. (A) Pontine tegmental cap dysplasia is a rare hindbrain malformation that includes dysplasia of the cerebellar vermis, lateral-ized superior cerebellar peduncles, ectopic dorsal transverse pontine fibers (tegmental cap), flattened ventral pons, absence of the inferior olives, and absence or near absence of the middle cerebellar peduncles. (C) Joubert syndrome is characterized by vermian hypoplasia or aplasia and lack of decussation of the superior cerebellar peduncles, resulting in a “molar tooth” appearance. (D) A Dandy-Walker malformation can result in cystic enlargement of the posterior fossa in communication with the fourth ventricle. The vermis is hypoplastic, but there is no continuation of the cerebellar structures.
C Bullet tract crossing the deep midline structures
Various studies consistently have shown that bullet tracts crossing the midline (i.e., bihemi-spheric involvement) are associated with increased mortality and worse functional outcomes in those patients who survive, although there are recent data suggesting that individuals with isolated bifrontal involvement may have a relatively better prognosis. Other significant negative prognostic factors include brainstem involvement, posterior fossa injuries, transventricular injuries, low Glasgow Coma Scale score, nonreactive pupils, and older age. (A) The presence of both entry and exit wounds is not a significant predictor of worse outcomes. (B) Involvement of the inner and outer tables of the calvaria is not a significant predictor of worse outcomes. (D) The presence of bullet fragments is not a significant predictor of worse outcomes. (E) The presence of an open comminuted fracture is not a significant predictor of worse outcomes.
A Globus pallidus interna
The image accompanying the question shows bilateral deep brain stimulator leads terminating in the globus pallidus interna (GPi) that are used to treat motor fluctuations in advanced medication resistant Parkinson disease or levodopa induced dyskinesia. (B) The subthalamic nuclei are an alternative target for deep brain stimulation in Parkinson disease. They are located at a lower level superior to the substantia nigra, lateral to the red nuclei, and medial to the internal capsule. (C) The ventral intermediate nuclei are located in the ventral thalami just lateral to the red nuclei. They are a common target for the treatment of essential tremors. (D) The red nuclei are paired, round T2 hypo-intense structures located in the rostral midbrain.
C Fibromuscular dysplasia
The medial type of fibromuscular dysplasia is by far the most common and can show a “string of pearls” appearance on angiography. The same descriptor also is sometimes used for cerebral vasculitis, which can show areas of alternating segmental vascular stenoses and dilatation. (A) A “string sign” sometimes is described with severe carotid artery stenosis due to a very thin column of contrast flowing through the narrowed segment. (B) The “buzz” term for a dural arteriovenous fistula is “retrograde cortical venous drainage” or “cortical venous reflux,” which is associated with more aggressive behavior and an indication for emergent treatment. (D) Arteriovenous malformations display early draining veins and the presence of a nidus sometimes with venous or arterial aneurysms. (E) Carotid artery dissections can show a “string sign” in the narrowed segment; however, dissection of the internal carotid artery typically is associated with a “flame shape” configuration when it occurs just above the level of the carotid bulb.
C Secondary to premature disjunction of the neural ectoderm
Lipomyelomeningoceles, lipomyeloceles, and lipomas are secondary to premature disjunction of the neural ectoderm from the cutaneous ectoderm. (A) Studies have not found a decreased incidence of lipomyelomeningoceles following folic acid supplementation, suggesting that the pathogenesis is different from that of other neural tube defects. (B) Open myelomeningoceles are the sine qua non of Chiari 2 malformations. Closed defects covered by skin such as this one do not result in Chiari 2 malformations. (D) The vast majority of lipomyelomeningoceles are sporadic. A few familial cases have been reported, but they are exceedingly rare.
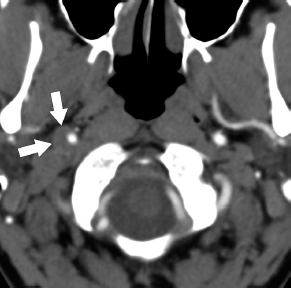
A Facial nerve
There is an avidly enhancing mass involving the right geniculate ganglion as well as the labyrinthine and canalicular segments of the right facial nerve compatible with a schwannoma. The vast majority of intracranial schwannomas arise from the vestibular nerve followed by the trigeminal and facial nerves. (B) A vestibular schwannoma would not involve the facial nerve canal or geniculate ganglion. (C) An aberrant internal carotid artery is seen more inferiorly as a more lateral extension of the internal carotid artery beyond the cochlear promontory. It may appear as a pulsating “mass” on clinical exam. (D) The inferior petrosal sinus is located along the inferior aspect of the petrous bone. It drains blood from the cavernous sinus into the jugular vein.
A Meningohypophyseal trunk
The tentorial artery (of Bernasconi and Cassi-nari) is the most constant branch of the meningohypophyseal trunk, which in turn arises from the cavernous internal carotid artery. It is an important structure due to its vascular supply to lesions in the region of the tentorium cerebelli, such as vascular malformations and meningiomas. (B) The inferolateral trunk arises along the lateral aspect of the cavernous internal carotid artery and projects inferiorly. It usually has three or four branches and multiple anastomoses with branches of the external carotid artery. (C) The neuromeningeal trunk is a branch of the ascending pharyngeal artery and consists of jugular and hypoglossal divisions. (D) The posterior cerebral arteries most commonly arise as bifurcations of the basilar artery.
D Flexion-distraction injury
The fracture demonstrated is a classic case of a severe flexion-distraction injury with a teardrop-type fracture of the anteroinferior C4 vertebra as well as distraction of the C4–C5 facets and posterior elements as can be seen on the CT images. The STIR image shows extensive edema in the posterior soft tissues including the interspinous ligaments, which are disrupted. These are highly unstable fractures associated with acute anterior cervical cord syndrome. (A) A hangman (or more correctly “hangee”) fracture involves both pedicles or both partes interarticulares of C2 and is secondary to hyperextension and distraction. (B) A clay-shoveler fracture is a stable fracture involving a lower cervical vertebra (usually C7) and sometimes the upper thoracic spine. The fracture is a type of hy-perflexion avulsion injury. (C) A Jefferson fracture is a burst fracture of the C1 vertebra. It is considered unstable if the combined offset of the lateral C1 masses measures more than 7 mm or if the atlantodental distance measures more than 3 mm. (E) Locked facets may be a result of a flexion-distraction injury and can result in listhesis. The C4–C5 facets in this case are mildly distracted.
B Convex posterior vertebral margins
Convex posterior vertebral margins are suggestive of metastatic disease. Other features that would support this etiology are epidural or paravertebral masses or the presence of vertebral metastases at other levels. Metastases tend to involve the pedicle and posterior elements more commonly, but these sites also can show edema related to benign fractures. (A) Horizontal low signal intensity bands can be seen on both T1- and T2-weighted images and are more common in benign osteoporotic fractures. (C) Areas of spared vertebral marrow (best seen as high signal on noncontrast T1 images) are seen more commonly in benign compression fractures. (D) Retropulsion of a bone fragment is more suggestive of a benign compression fracture. (E) Both benign and pathological compression fractures can be accompanied by significant enhancement.
A Trinucleotide repeat expansion
The CT shows atrophy of the heads of the caudate nuclei bilaterally, resulting in abnormal ballooning of the frontal horns of the lateral ventricles, which is consistent with Huntington disease, given the patient’s clinical presentation. Huntington disease results from trinucleotide (CAG) repeat expansion in the huntingtin gene, which is located on chromosome 4. (B) Point mutations are modifications of a single nucleotide base and include substitutions, deletions, and insertions. (C) Frameshift mutations result from insertions, deletions, or duplications that alter the normal trinucleotide reading frame. (D) Deletions indicate of loss of genetic material and can involve individual bases or an entire gene.
E Blood products
Gradient echo (GRE) sequences generate images that particularly are susceptible to magnetic field inhomogeneities such as those produced in the presence of paramagnetic blood degradation products (e.g., hemosiderin and ferritin). The presence of these products manifests as signal loss and can be used to detect hemorrhage. Dynamic susceptibility contrast MRI and functional MRI are different techniques based on GRE sequences. (A) Myelin injury is difficult to demonstrate on conventional MRI unless there is clear disruption of the white matter. Certain metrics based on advanced MRI techniques such as radial diffusivity (RD) in diffusion tensor imaging (DTI) may serve as indicators of primary myelin injury. A different technique called magnetization transfer can provide a measure of the contribution of protons that are bound to macromolecules (e.g., myelin) and has been employed in the evaluation of demyelinating disorders. (B) Diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) maps is very sensitive for the detection of purulence within abscesses, cavities, or the ventricular system. (C) Acute ischemia is best demonstrated with DWI and ADC maps. (D) Glucose metabolism can be assessed with positron emission tomography (PET) by using fluorodeoxyglucose (FDG).
A It may be related to connective tissue disorders.
The image on the left shows somewhat crescen-tic and nearly circumferential mural thickening of the left vertebral artery in a patient with a spontaneous dissection (compare with the normal dark vascular flow void on the right). The image on the right shows cerebellar infarcts. Minor or sometimes unrecalled trauma may account for some cases of “spontaneous” dissection, and there is an increased incidence in patients with connective tissue disorders. (B) Vertebral artery dissection occurs in young and middle age adults with a mean age of presentation of 40 years of age. (C) Extra-dural vertebral artery dissections are more common than intradural ones. (D) Rupture is more common in intradural vertebral dissections because of a lack of external elastic lamina, fewer elastic fibers in the media, and a thinner adventitial layer.
C It is associated with Morquio syndrome and multiple epiphyseal dysplasia.
An os odontoideum is a rare anomaly of the cervical spine characterized by a deformity of the odontoid process that appears as a smooth and well-corticated ossicle separated from the body of C2. There may be hypertrophy of the anterior C1 arch, as seen in this case. It may be orthotopic where the ossicle is in a relatively anatomic location with a gap between it and the body of C2, or dystopic where the ossicle is located in any other position. An increased frequency of os odontoideum has been reported in patients with multiple epiphyseal dysplasia and in Morquio, Down, and Klippel-Feil syndromes. (A) The ossicle above the body of C2 is round and features smooth, well-corticated margins; therefore, the abnormality shown is not an acute fracture. (B) Failure of fusion of the ossiculum terminale usually results in a much smaller ossicle above an overall normal-appearing odontoid process (except for a small notch at the tip). The ossiculum terminale normally fuses with the body of the dens around age 12. When persistent, it usually is asymptomatic and rarely associated with instability. (D) An os odontoideum usually is asymptomatic and, in many instances, is discovered incidentally; however, it may be associated with instability due to hypermobility of C1 over C2. This immobility may lead to spinal cord or, less frequently, vertebral artery compression. Dystopic lesions are more likely to be unstable than orthotopic lesions.
A Dural venous sinus stenosis
The axial T2 image shows distention of the optic nerve sheaths and prominence of the optic cups bilaterally due to an increased intracranial pressure and papilledema in a patient with idiopathic intracranial hypertension (pseudotumor cerebri). The sagittal CISS image on the right shows an expanded and partially empty sella turcica. Additional findings in these patients include dural venous sinus stenosis, enlargement of the Meckel caves, and cerebrospinal fluid arachnoid pits in the sphenoid bones. (B) Venous sinus engorgement is seen in intracranial hypotension, not hypertension, due to decreased cerebrospinal fluid volumes (and in keeping with the Monro-Kellie doctrine). (C) Brainstem sagging is a feature of intracranial hypotension. (D) Decreased mammil-lopontine distance is a sign of brainstem sagging in intracranial hypotension.
D Cranial nerve XII
The hypoglossal canals course along the medial and superior aspects of each occipital condyle between the basiocciput and the jugular process. They transmit cranial nerve XII, which is at high risk of injury in the presence of condylar fractures. (A) Cranial nerve IX courses through the pars nervosa of the jugular foramen along with the inferior petrosal sinus. (B, C) Cranial nerves X and XI course through the pars vascularis of the jugular foramen along with the jugular bulb.
A Has a tendency for leptomeningeal spread
The axial T2 image shows a T2 hypointense mass involving the left posterior globe and left optic nerve extending posteriorly to the level of the chi-asm. There are foci with even lower signal intensities within the globe consistent with hemorrhage. Although an optic glioma may cause enlargement of the optic nerve, involvement of the eye and deletion of chromosome 13q (which contains the RB1 gene locus) indicates a diagnosis of retinoblas-toma. This is a highly malignant tumor that has a tendency for leptomeningeal spread. (B) Anterior eye segment enhancement generally represents reactive angiogenesis. (C) Retinoblastomas, as with other primitive neuroectodermal tumors, commonly have profoundly low apparent diffusion coefficient values due to high cellularity and restricted diffusion. (D) The lesion shown likely has areas of low signal intensity on susceptibility-weighted imaging due to calcifications and hemorrhage.
A Usually heals well with traction and immobilization
This is a type 3 fracture of the odontoid process extending from its base into the body of C2. These fractures are unstable, as they allow the odontoid process to move with the occiput as a unit; however, they have the best prognosis of all odontoid fracture types. They usually heal well with traction followed by bracing. (B) Although type 3 odontoid fractures have the best prognosis of all odontoid fracture types, they are considered unstable. (C) Type 2 odontoid process fractures are the most common. They occur across the base of the odontoid process at its junction with the body of C2. (D) Type 3 odontoid fractures occur inferior to the level of the transverse band of the cruciform ligament. (E) Type 2 odontoid process fractures are the most likely to progress to nonunion.
B Carotid-cavernous fistula
The axial precontrast T1 image on the left shows a round, mixed signal intensity lesion in the left cavernous sinus. Note a subtle horizontal band at the level of the lesion propagating in the phase-encoding direction compatible with pulsation artifact. The T2 image on the right shows areas of profound hypointensity. Findings are indicative of an aneurysm, which probably is partially throm-bosed. Compared with anterior and posterior circulation aneurysms, cavernous carotid aneurysms have the lowest rate of rupture (posterior circulation aneurysms have the highest). Rupture of cavernous carotid aneurysms may result in direct carotid-cavernous fistulae. (A) Malignant transformation may be seen in certain neoplasms. The lesion in this case is an aneurysm. (C) Subarach-noid hemorrhage can occur from rupture of an intradural aneurysm. (D) Posterior circulation infarcts can be the result of embolic phenomena from aneurysms located more proximally in the posterior circulation.
C Deep venous drainage connotes increased surgical risk
With arteriovenous malformations, deep venous drainage, involvement of eloquent cortex, and larger nidal sizes connote an increased surgical risk and are part of the Spetzler-Martin grading system. (A) Cortical venous reflux is associated with an increased bleeding risk in patients with dural arteriovenous fistulas. The patient in this case has a pial arteriovenous malformation with a large nidus supplied from branches of the anterior and middle cerebral arteries. (B) Most arteriovenous malformations (98%) are solitary, but they rarely may be multiple particularly in patients with certain syndromes such as Osler-Weber-Rendu (who also can have microaneurysms), Wyburn-Mason, and craniofacial arteriovenous metameric syndromes (CAMS). Klippel-Trenaunay-Weber syndrome is characterized by capillary, venous, and lymphatic malformations as well as soft tissue and osseous hypertrophy. (D) Most arteriovenous malformations (75%) have a primary pial blood supply from the internal carotid artery; 15% have dual supply from the external carotid artery; 10% receive blood from both the internal and external carotid arteries.
B Frequently associated with diving head first into shallow water
This is a burst fracture of C1 (also known as Jefferson fracture) that develops due to axial loading transmitted through the occipital condyles into the C1 vertebra and is seen frequently after diving head first into shallow water. Jefferson fractures tend to be stable, and neurologic deficits are infrequent unless there is disruption of the transverse ligament, fractures at other levels, or injury to the vertebral arteries. Disruption of the transverse ligament is suspected if there is widening of the atlantodens interval (normally less than 3 mm in adults and 5 mm in children) or if the combined offset of the lateral masses of C1 relative to the lateral C2 pillars measures greater than 6 mm. If the transverse ligament is disrupted, stability depends on the alar ligaments connecting the dens with the medial aspect of the occipital condyles. (A) Combined offset of the lateral C1 masses relative to C2 greater than 6 mm suggests disruption of the transverse ligament and raises concern about an unstable fracture. (C) Jefferson fractures have a low frequency of neurologic injury unless there is disruption of the transverse ligament, fractures at other levels, or injury to the vertebral arteries. (D) Jefferson fractures are extremely rare in infants and young children, probably due to the plasticity of their bones and the presence of soft synchon-droses. (E) These fractures usually are managed conservatively unless they are unstable.
C Remote injury
The area of hypoattenuation in the left frontal lobe is consistent with encephalomalacia. It demonstrates very low attenuation and is associated with volume loss, as can be seen by ex vacuo expansion of the frontal horn of the left lateral ventricle. This likely is secondary to remote trauma, infarction, or other injury. This patient also has an acute, right frontal, extra-axial hematoma. (A, B) Acute or subacute infarction or cortical contusion would not be associated with volume loss, and the lesion margins would likely be less well defined. (D) A neoplasm would show some degree of mass effect and may have surrounding edema. (E) There is no fluid collection or evidence of vasogenic edema to suggest an abscess.
C Subacute combined degeneration
Subacute combined degeneration is caused by vitamin B12 deficiency, and leads to demyelination and vacuolization of the dorsal columns of the spinal cord with or without involvement of the lateral columns. It most commonly occurs in the upper thoracic and cervical cord. MRI shows T2 signal hyperintensity with rare contrast enhancement. Subacute combined degeneration can be exacerbated or caused by nitrous oxide toxicity, which temporarily interrupts metabolism of B1 2. (A) There is no evidence of a space-occupying lesion to suggest a neoplasm. Ependymomas tend to occur centrally within the spinal cord, and cysts, hemorrhage, and calcifications are common findings. (B) Neuro-myelitis optica results in greater cord expansion than demonstrated in the image and usually is more central and not confined to the dorsal columns. (D) Infectious myelitis is rare, and imaging may show edema that is not confined to the dorsal columns.
B Invasive fungal infection
The “black turbinate” sign refers to nonenhancing nasal mucosa due to tissue infarction, and has been described in angioinvasive fungal infections. The skull base findings in this case are secondary to fungal osteomyelitis. (A) Bacterial infection can lead to osteomyelitis of the skull base but does not result in a “black turbinate” sign. (C) Nasopharyn-geal carcinoma can invade the skull base but does not produce a “black turbinate” sign. (D) Osseous infarctions can present with mixed signal intensities on T2-weighted MRI sequences due to areas of edema and sclerosis and irregular enhancement. Skull base infarcts are rare but occur more commonly in patients with sickle cell disease, in which case they can be complicated by osteomyelitis.
B Failure of diverticulation
These images show nonseparation of the frontal lobes and an azygous anterior cerebral artery in a patient with lobar holoprosencephaly. These occur secondary to the failure of diverticulation and cleavage of the prosencephalon during embryonic life. Holoprosencephaly represents a spectrum of abnormalities, with the alobar form being the most severe and commonly presenting with a mono-ventricle, thalamic fusion, and facial anomalies. (A) Failure of closure of the rostral neuropore leads to anencephaly. (C) Nondisjunction of the neural tube can result in open spinal dysraphisms. (D) Premature disjunction of the neural tube can lead to lipomyeloceles, lipomeningoceles, and lipomyelo-meningoceles.
A Atypical teratoid rhabdoid tumor
Atypical teratoid rhabdoid tumors and other embryonal tumors as well as medulloblastomas are highly malignant and typically show the lowest apparent diffusion coefficient (ADC) values due to their high cellularity. (B) Juvenile pilocytic astrocy-tomas are WHO grade I tumors that do not show significant restricted diffusion. (C) Ependymomas may show variable degrees of restricted diffusion, but their ADC values typically are higher than those of embryonal tumors. (D) Dysembryoplastic neu-roepithelial tumors are benign glioneuronal neoplasms (WHO grade I) that do not show restricted diffusion; therefore, their ADC values are high. (E) Diffuse astrocytomas are WHO grade II lesions that do not show significant restricted diffusion.
D It is typically a monophasic process.
Acute demyelinating encephalomyelitis (ADEM) usually is a monophasic process, but some patients are at an increased risk of recurrence (defined as a new event after 3 months) or the development of multiple sclerosis. (A) Approximately 75% of cases of ADEM occur after viral and less commonly bacterial (e.g., Campylobacter) infections. (B) The deep gray nuclei (particularly the thalami) are involved in 60% of patients with ADEM. These structures are involved less commonly in multiple sclerosis. (C) Only 25% of ADEM lesions show contrast enhancement. There usually is no mass effect except for cases of tumefactive demyelination, which also may be accompanied by a leading edge of restricted diffusion.
A Adrenoleukodystrophy
The presentation and imaging findings are consistent with X-linked adrenoleukodystrophy. This disease typically occurs in 4- to 6-year-old boys and is caused by mutations in the ABCD1 gene, leading to accumulation of very long chain fatty acids. Death or progression to a vegetative state usually occurs 2 years after symptom onset. (B) Canavan disease is caused by mutations in the ASPA gene on chromosome 17. It results in macrocephaly, with imaging showing sequelae of white matter demyelination and signal abnormalities in the globi pallidi and thalami. (C) Alexander disease is caused by mutations in the GFAP gene on chromosome 17. It is characterized by demyelination that progresses from anterior to posterior. Patients have astro-cytic Rosenthal fibers and macrocephaly. (D Krabbe disease results from mutations in the GALC gene on chromosome 14 and leads to the deficiency of galactocerebroside β-galactosidase. The condition most commonly is diagnosed between the third and sixth months of life. Imaging shows abnormalities in the white matter, basal ganglia, cerebellum, and corticospinal tracts. (E) Pelizaeus-Merzbacher disease is an X-linked recessive disorder characterized by oligodendrocyte dysfunction leading to hypomyelination. Patients usually are males and present with nystagmus, seizures, hypotonia, and ataxia. On MRI, there is diffuse T2 signal hyper-intensity in the white matter due to hypomyelination (myelinated white matter is dark on T2 and bright on T1 sequences).
D Subacute combined degeneration
Subacute combined degeneration can be caused by vitamin B12, copper, or vitamin E deficiencies. It results in an abnormal signal within the dorsal columns of the spinal cord in an inverse V-shaped configuration with variable involvement of the lateral columns. Abuse of nitrous oxide can produce the same syndrome through inactivation of vitamin B12. Neurosyphilis (tabes dorsalis) is also known to involve the dorsal columns. (A) Poliomyelitis may show an abnormal signal and enhancement of anterior horn cells as well as ventral roots of the cauda equina if accompanied by radiculitis. (B) Amyotrophic lateral sclerosis preferentially involves the anterior and lateral columns of the spinal cord, which may show increased T2 signal. (C) Guillain-Barré syndrome presents with preferential pial enhancement of the conus medullaris and dorsal roots of the cauda equina. It should not be associated with intramedullary signal abnormalities.
D Capillary telangiectasia
The imaging description of this lesion and its location are characteristic of capillary telangiecta-sias. Low signal on gradient echo (GRE) sequences is thought to be related to slow flow and increased deoxyhemoglobin content. These lesions sometimes can have areas of gliosis, and they nearly always are asymptomatic and found incidentally. (A) A demyelinating plaque does not show the constellation of features described, which are characteristic of capillary telangiectasias. (B) Capillary telangiectasias should be differentiated from metastases. The latter usually have surrounding edema (except for small lesions) and do not show signal loss on GRE sequences unless they are hem-orrhagic, melanotic, or calcified. (C) Cavernous malformations may show various signal intensities depending on the stage of their blood products. They typically are described as having a “popcorn” or “berry” appearance with a surrounding rim of hemosiderin.
A Between meningeal branches of the external carotid artery and cavernous sinus
Carotid cavernous fistulas can be direct or indirect. Direct fistulas (Barrow type A) develop between the cavernous internal carotid artery and cavernous sinus and are therefore high flow. They are more frequent in younger males and occur secondary to trauma or rupture of a cavernous internal carotid aneurysm. Types B, C, and D occur between meningeal branches of the internal or external carotid arteries, are slow flow, and are most frequently seen in women older than 50 years of age. A type C carotid cavernous fistula occurs between meningeal branches of the external carotid artery and cavernous sinus. (B) A Barrow type B fistula occurs between meningeal branches of the internal carotid artery and cavernous sinus. (C) A Barrow type A fistula occurs directly between the cavernous internal carotid artery and cavernous sinus. (D) A Barrow type D fistula occurs between meningeal branches of both the external and internal carotid arteries and cavernous sinus.
E Associated with a risk of malignant transformation
T2, FLAIR, and diffusion-weighted imaging (DWI) MRI sequences are presented showing an epider-moid cyst. These lesions are characterized by very bright DWI signal (presumably a combination of restricted diffusion and T2 shine-through effect), lack of contrast enhancement, and nonsuppression on FLAIR. Epidermoid cysts arise from ectodermal inclusions during neural tube closure and rarely can degenerate into squamous cell carcinomas. (A) Arachnoid cysts and not epidermoid cysts are lined by arachnoid cells, resulting in accumulation of cerebrospinal fluid. (B) Up to 50% of epidermoid cysts are located in the cerebellopontine angle, although they uncommonly may arise within the ventricles. (C) Although signal in epidermoid cysts may resemble cerebrospinal fluid on T2, they do not suppress on FLAIR as demonstrated in the second image. The signal of epidermoid cysts on FLAIR sometimes has been described as “dirty” appearing and used to be the main imaging discriminator for diagnosis before DWI was available. This is in contradistinction to arachnoid cysts, which do suppress on FLAIR and follow cerebrospinal fluid signal on all sequences. (D) Although there sometimes can be minimal marginal contrast enhancement, epidermoid cysts should not show patchy or any significant enhancement, which would be suspicious for malignant transformation.
C Pilocytic astrocytoma
B Acute infarction
Noncontrast CT and diffusion-weighted images are presented, and the distribution of the abnormality and presence of restricted diffusion are most compatible with an acute posterior inferior cerebellar artery (PICA) territory infarct. PICA infarcts may be associated with significant mass effect in the posterior fossa and herniation with rapid deterioration and death. Although they can present with specific neurologic syndromes (such as lateral or medial medullary syndromes), symptoms can be vague and nonspecific, and sometimes may be confused with labyrinthitis or gastroenteritis. (A) Hemorrhagic or high-grade primary neoplasms may result in areas of restricted diffusion due to blood products or high cellularity, respectively; however, they would be expected to be more heterogeneous and would not preserve the cerebellar architecture as in this case (note that some of the folia still can be defined on the diffusion image). Additionally, the vascular distribution of the abnormality and the evolution of symptoms over a few hours are compatible with a PICA territory infarct. (C) Approximately 50% of intracranial metastases may be solitary; however, findings in this case argue against a metastatic lesion. (D) Although the lesion presented is hypodense on CT, it is intra-axial and demonstrates restricted diffusion, both of which rule out an arachnoid cyst. (E) Epider-moid cysts can show restricted diffusion, and some can be intra-axial; however, in this case, the vascular distribution is characteristic of a PICA infarct.
C Global anoxic injury
This is a case of diffuse cerebral edema/global anoxic injury. The noncontrast head CT shows effacement of the cerebral sulci, small ventricles, loss of the gray matter-white matter distinction, lack of definition of the deep gray nuclei, and effacement of the basal cisterns. (A) A ruptured intradu-ral cerebral aneurysm would result in subarachnoid hemorrhage. The hyperdense appearance of the suprasellar cistern in this case often is referred to as “pseudosubarachnoid hemorrhage” and is due to the relative hypodensity of the swollen brain parenchyma and cisternal effacement. (B) Acute arterial infarction would lead to edema and mass effect in a territorial distribution. (D) Venous thrombosis may or may not result in ischemia that sometimes can become hemorrhagic. Findings that can be seen on CT include a hyperdense clot within the dilated vein (cord sign), cortical/subcortical edema (when cortical veins are involved), and deep gray matter edema (when deep draining veins are involved and often occurring bilaterally).
A Glioma
This is a case of neurofibromatosis type 1. The provided images show dysplasia of the left sphenoid bone with ipsilateral proptosis as well as a diffuse, nodular, and trans-spatial lesion involving the left head, face, neck, and parapharyngeal tissues compatible with plexiform neurofibromata. A central T2 dark spot may be seen within some of these lesions (the “target sign”) and is considered highly suggestive of neurofibromas. Approximately 15% of children with neurofibromatosis type 1 develop optic nerve gliomas, and they are also at an increased risk of developing gliomas in other regions of the brain. In addition, 4% of patients with neurofibromatosis type 1 develop peripheral malignant nerve sheath tumors. (B, C) Multiple inherited schwannomas, meningiomas, and ependymomas (MISME syndrome) are features of neurofibromatosis type 2 and not type 1. (D) Endolymphatic sac tumors are very rare neoplasms that can occur sporadically and have been reported to develop in 10 to 15% of patients with von Hippel-Lindau syndrome. (E) Almost all subependymal giant cell tumors are seen in the setting of tuberous sclerosis.
D Less common cerebral edema
Epidural empyemas are associated less frequently with cerebral edema due to the presence of thick intervening dura between the collection and the brain. (A) Both epidural and subdural hematomas show restricted diffusion. (B) Similar to subdural hematomas, a crescentic shape is more consistent with a subdural hematoma, whereas epidural collections characteristically have a biconvex or lenticular shape. Note that subdural empyemas and hematomas sometimes can show a lenticular shape particularly if they are loculated. (C) Epidural collections including empyemas and hematomas do not cross sutures due to the firm dural attachments at these sites. (E) Both subdural and epidural empyemas enhance peripherally.
A Extension beyond the lateral intercarotid line
Extension beyond the lateral intercarotid line, as measured on coronal images, is highly suggestive of cavernous sinus invasion by a pituitary adenoma with a positive predictive value of 85%. Other findings include obliteration of the carotid venous sulcus compartment (the space between the sphenoid bone and the ipsilateral cavernous internal carotid artery) with a positive predictive value of 95% and internal carotid artery encasement of ≥ 67% (about 240 degrees) with a positive predictive value of 100%. (B) Carotid encasement of ≥ 67% has been associated with the highest likelihood of ipsilateral cavernous sinus invasion. (C) Obliteration of the superior venous compartment is not significantly associated with cavernous sinus invasion. (D) Obliteration of the inferolateral venous compartment is not significantly associated with cavernous sinus invasion.
A Fibromuscular dysplasia predisposes to an increased risk of direct-type lesions.
The angiogram shows early opacification of the cavernous sinus compatible with a carotid cavernous fistula. This is most evident on the left side, where the ophthalmic vein also can be seen. These lesions result from either a direct communication between the carotid artery and cavernous sinus (direct or high-flow fistulas; Barrow type A) or between the cavernous sinus and dural branches of the internal carotid artery, external carotid artery, or both (indirect, low flow, and dural fistulas; Barrow types B, C, and D, respectively). Other than trauma and aneurysmal rupture, conditions associated with direct carotid cavernous fistulas include fibromuscular dysplasia, Ehlers-Danlos syndrome, and pseudoxanthoma elasticum. (B) Spontaneous parenchymal or subarachnoid hemorrhage can be seen in direct fistulas, particularly when there is retrograde cortical venous flow, and occurs in about 5% of cases. Bruits and visual manifestations are much more common. (C) Direct (not dural type) fistulas commonly present with a subjective bruit (about 85% of cases) that sometimes also may be auscultated. (D) Venous thrombosis is a known mechanism in the development of some carotid cavernous fistulas; however, by far the most common etiologies of direct fistulas are trauma and aneurysm rupture. (E) Dural fistulas most commonly present in middle-aged and elderly women. Traumatic direct fistulas are more common in young males.
E Usually shows minimal to no contrast enhancement
A They are most common in basal ganglia and dentate nuclei.
The focal areas of signal intensity (FASI) or unidentified bright objects (UBOs) are thought to represent myelin vacuolization in patients with neurofibromatosis type 1. They are most common in the basal ganglia, dentate nuclei, and brainstem. (B–D) These lesions are not premalignant, and many regress in adulthood. They do not show contrast enhancement or mass effect, the presence of which should raise concern about a glioma.
B Diffusion weighted
The two most important sequences in the evaluation of a cerebral abscess are contrast-enhanced T1-weighted sequences and diffusion-weighted imaging (DWI). An abscess usually shows a relatively smooth and homogeneous enhancing wall that often (but not always) is thicker on the side of the gray matter and thinner toward the ventricles and white matter. Pus within an abscess almost always shows prominent restricted diffusion, which is reflected as bright signal on DWI and corresponding dark signal on apparent diffusion coefficient (ADC) maps. (A) Susceptibility-weighted imaging (SWI) is a gradient echo-based technique that is exquisitely sensitive for the detection of paramagnetic and diamagnetic substances such as ferritin, calcium, hemosiderin, and deoxyhemo-globin. The capsule of an abscess may appear dark on SWI or T2, presumably due to the presence of paramagnetic free radicals within macrophages. (C) Time of flight is an MR angiography technique that does not routinely require the administration of contrast material and is based on the flow-related enhancement of spins entering an imaging slice in one direction. (D) Constructive interference in steady state (CISS) is an MRI technique that is based on consecutive steady-state free precession (SSFP) sequences. It produces images that have very high T2 signal and therefore excellent contrast between fluid and parenchyma. (E) Fluid-attenuated inversion recovery (FLAIR) is a pulse sequence that uses an inversion recovery technique to null the signal of simple fluid.
C Hemangioma
These CT images show the characteristic imaging features of a vertebral hemangioma with vertical trabeculations on the sagittal image and a corresponding “polka dot” appearance on the axial image. Note the preservation of the cortex despite the presence of the trabeculations; however, also remember that hemangiomas can be aggressive and may present with extraosseous soft tissue extension and mass effect on the spinal cord or nerves. On MRI, they usually are bright on both T1 and T2 sequences due to the presence of a fatty stroma, although atypical (predominantly vascular) hemangiomas may be dark on T1 and simulate metastases. Approximately 30% of hemangiomas are multiple. (A) Metastasis would result in variable degrees of marrow replacement and osseous destruction without the vertical trabecular pattern of a hemangioma. (B) Paget disease is associated with expansion of the bone; in the spine, the involved vertebra often appears larger than the ones above and below it. Paget disease also presents with cortical thickening and would not show a uniform, vertical trabecular pattern. (D) Plas-macytomas cause osseous destruction and do not respect the trabeculae.
B Synovial cyst
The axial T2 image shows a well-circumscribed, cystic-appearing, extradural mass, with its base along a degenerated and hypertrophied left facet joint, which is compatible with a synovial cyst. In this case, the cyst impinges on the left descending nerve roots, which explains the patient’s symptoms. The morphology of the cyst and its anatomic relationship with a degenerated facet joint are more important than the signal of its contents, which may vary depending on the presence of hemorrhage or proteinaceous material. Synovial cysts can contain gas, and their walls may show enhancement or calcification. They most commonly develop in patients older than 60 years of age and are more common in females; 90% occur in the lumbar spine. (A) In this case, the open base of the lesion is centered along the facet rather than the disk, and the T2 bright contents also seem to communicate with the facet joint. Additionally, the lesion has a convex, well-circumscribed margin anteriorly. These features make a synovial cyst the right diagnosis; however, note that disk material can separate from the parent disk and migrate virtually anywhere within the epidural space. (C) Cysts also can originate from the ligamenta flava; however, the lesion in this case is centered along the facet joint. (D) The uncovertebral joints form between the uncus and uncinate processes of the cervical spine between C3 and C7. There are no uncovertebral joints in the lumbar spine. Additionally, hypertrophied bone and osteophytes would look dark on T2 and not bright as in this lesion.
B It is composed of radially arranged medullary veins emptying into a dilated draining vein.
This image shows radially arranged medullary veins in a “caput medusae” configuration emptying into a dilated draining vein compatible with a developmental venous anomaly (also known as a venous angioma). These lesions usually are benign and constitute an incidental finding in the majority of cases, although rarely they may thrombose. Some reports have described seizures, headaches, and hemorrhage, but the association of venous angiomas and these manifestations has not been established firmly. Approximately 20 to 30% of these lesions are associated with cavernous malformations, which may explain symptoms in at least some cases. The majority of developmental venous anomalies are isolated, but they also can be multiple particularly when associated with the blue rubber bleb nevus syndrome. Blood oxygen level dependent (BOLD) imaging sequences, such as susceptibility-weighted imaging (SWI), are the preferred modality for their detection, as these lesions may be missed on other sequences due to their slow flow. (A) Developmental venous anomalies have a characteristic appearance on angiography, showing exclusive enhancement in the venous phase, although sometimes a faint blush may be evident in the late arterial phase. Angiographically occult vascular lesions include capillary telangiec-tasias and cavernous malformations. (C) High flow from shunting may result in flow-related aneurysms in arteriovenous malformations. There is no arteriovenous shunting in developmental venous anomalies. (D) A larger nidus is associated with an increased surgical risk in arteriovenous malformations and upgrades these lesions in the Spetzler-Martin grading system.
D Renal cell carcinoma
The MRI shows a heterogeneously enhancing destructive lesion in the left petrous bone. There are areas of intrinsic T1 hyperintensity secondary to hemorrhage, proteinaceous contents, or cholesterol. The appearance and location are suggestive of an endolymphatic sac tumor, particularly in a patient presenting with spontaneous retinal detachment, which may be seen in von Hippel-Lindau (VHL) syndrome due to hemorrhage from retinal capillary hemangioblastomas; 15% of patients with VHL develop an endolymphatic sac tumor, and 40 to 70% of them ultimately develop renal cell carcinoma, the incidence of which increases with age. (A) Lisch nodules are the most common ocular lesions in neurofibromatosis type 1. They are not associated with VHL syndrome. (B) Bilateral ves-tibular schwannomas are diagnostic of neurofibromatosis type 2. (C) Subependymal giant cell astrocytomas occur in patients with tuberous sclerosis complex secondary to mutations in the TSC-1 or TSC-2 genes, although isolated tumors rarely have been described. These tumors are not associated with VHL. (E) Low levels of serum ceruloplas-min result in an abnormal accumulation of copper in Wilson disease.
B Frequently accompanied by microcephaly and other cerebral anomalies
B Chordoma
Skull base chordomas most commonly present in patients between 20 and 40 years of age, but 16% occur in patients younger than 18 years of age. Location in the lower clivus with associated osseous erosion is typical. On MRI, they demonstrate very bright T2 signal, presumably related to muci-nous contents along with thin T2 dark fibrous septations. They show moderate to marked enhancement often along the septations in a “honeycomb” configuration. Skull base chordomas carry a poor prognosis, worse than that for chondrosarco-mas. (A) Chondrosarcomas have imaging features similar to those for chordomas, but they more often occur off midline and centered at the petroclival fissure, and may be accompanied by calcified chondroid matrix. Chondrosarcomas are unusual at this age. (C) Nasopharyngeal carcinoma is rare at this age; it would have a more infiltrative appearance, and it is not as bright on T2 sequences. Additionally, the nasopharyngeal mucosa is preserved in this case, and the tumor is centered at the skull base, resulting in anterior deviation of the prevertebral muscles as seen on the axial images. (D) Meningio-mas can invade bone but tend to do so more diffusely. They also are not as bright on T2 sequences (unless there are areas of degeneration) and tend to show more homogeneous enhancement without the honeycomb appearance of this case. They are rare in children unless associated with a syndrome. (E) Lymphoma can arise from lymphoid tissue in the nasopharynx and extend to the skull base; however, the nasopharyngeal mucosa in this case is preserved. Lymphoma also usually enhances more avidly and homogeneously.
A Cholesterol granuloma
This is a well-circumscribed, expansile lesion centered in the left petrous apex. It does not enhance, and it shows intrinsic T1 brightness as well as T2 dark material within it, corresponding to blood products. There is no restricted diffusion as demonstrated by increased signal on the apparent diffusion coefficient (ADC) map. Findings are compatible with a cholesterol granuloma. These are benign lesions related to repeated middle ear infections. They contain cholesterol crystals, lipids, and fluid and are prone to recurrent hemorrhage. Cholesterol granulomas can occur anywhere in the temporal bone where there are mucosa-lined aerated cells, and rarely have been reported in the paranasal sinuses. (B) Cholesteatomas can occur in this location but show restricted diffusion (they would be dark on ADC and bright on diffusion-weighted imaging) and usually are not bright on T1. (C) Trapped secretions within pneumatized petrous cells sometimes can show intrinsic T1 brightness due to proteinaceous contents, but they would not result in an expansile mass. The normal trabeculae should be preserved, although this is difficult to visualize on MRI. (D) A trigeminal schwannoma would show enhancement and would follow the course of the cranial nerve sometimes with involvement of the Meckel cave.
E Flexion and distraction
The sagittal CT image shows a compression fracture involving a midthoracic vertebra with a fracture line extending posteriorly across the spinous process above. This is consistent with a Chance fracture, which features a horizontal fracture orientation through the entire spinal column and is a result of a flexion and distraction injury. These fractures usually are associated with lap belts. Neurologic injury is rare, but there is an increased frequency of intra-abdominal injuries. Up to 25% of Chance fractures may be purely ligamentous. (A) Extreme lateral bending can result in a lateral compression fracture or, potentially, a fracture of the transverse processes. Avulsion fractures of the transverse processes in the lumbar spine also can occur due to abrupt contraction of the psoas muscles. (B) Axial rotation can lead to facet dislocations, particularly in the cervical spine. (C) Abrupt extension of the neck can disrupt the anterior longitudinal ligament and result in an extension teardrop fracture, which is an unstable injury. (D) Axial loading can lead to burst or compression fractures of the anterior column if the injury occurs during flexion.
A Presence of lactate and amino acids on MR spectroscopy
The images in this case show an intra-axial lesion with peripheral enhancement and increased signal on diffusion-weighted imaging (DWI). Although apparent diffusion coefficient (ADC) maps are not presented, the degree of brightness in the center of the lesion on DWI is high enough that this is expected to represent restricted diffusion and would therefore look dark on ADC maps. These findings essentially are diagnostic of an abscess; a few rare cases of necrotic metastases with central restricted diffusion have been reported. Abscesses can show various amino acids on MR spectroscopy, including alanine, valine, leucine, and succinate as well as lactate and lipid peaks. Of note, necrotic primary or metastatic tumors also may show lactate and lipid peaks. (B) The capsule of a cerebral abscess usually is iso- to hypointense on T2-weighted sequences. This is attributed to the presence of collagen, blood products, or free radicals generated by phagocytosing macrophages. (C) The necrotic center of an abscess demonstrates significant restricted diffusion that manifests as very bright signal on DWI and low ADC values. (D) The capsule of an abscess typically has lower relative cerebral blood volume (rCBV) relative to white matter. Glio-blastomas, which may look similar to abscesses, have been associated with high rCBV ratios in the capsule.
D Paget disease
The etiology of Paget disease is not entirely certain. Its hallmark is excessive bone remodeling and overgrowth and is defined by three stages: lytic, mixed, and sclerotic. The spine and skull are the most common sites of involvement followed by the pelvis. The presence of pain or focal destructive lesions on imaging should raise concern for sarcomatous degeneration. (A) Multiple myeloma characteristically shows numerous lucent (lytic) lesions throughout the calvaria that may result in a “punched out” appearance. (B) Bone marrow hyperplasia in β-thalassemia can lead to significant skull thickening often showing a so-called hair-on-end appearance. It would not produce the lucent and sclerotic pattern of this case. (C) Prostate cancer metastases typically are osteoblastic (sclerotic) and can be diffuse; however, they do not result in the mixed lytic/sclerotic geographic pattern of this case. Note on the provided images that, despite the diffuse involvement of the calvaria, the inner and outer tables are relatively preserved.
B Posterior communicating artery aneurysm
The image shown is a lateral projection of a digital subtraction angiogram following a carotid artery injection. It shows a vascular outpouching projecting posteriorly from the dorsal aspect of the C7 (communicating or terminal) segment of the internal carotid artery at the expected origin of the posterior communicating artery. Aneurysms in this location represent about 30% of all ruptured intracranial aneurysms and may result in intra-parenchymal hemorrhage, typically in the mesial temporal lobe. Patients may present with subarach-noid hemorrhage or a third cranial nerve palsy due to mass effect. (C) This is a carotid injection and thus does not depict the posterior circulation and basilar tip. (D) The ophthalmic artery arises from the C6 (ophthalmic or supraclinoid) segment of the internal carotid artery and projects anteriorly.
B Increased relative cerebral blood volumes
Studies have shown that recurrent tumor has a higher relative cerebral blood volume (rCBV) normalized to the contralateral white matter compared with radiation necrosis, although there is some overlap. rCBV values greater than 2.6 have been suggested as a cutoff for the presence of recurrent tumor, and values lower than 0.6 suggest pseudo-progression. (A) Several studies show that recurrent tumor tends to have lower apparent diffusion coefficient (ADC) values compared with radiation necrosis. ADC ratios related to the contralateral white matter appear to be more accurate than absolute ADC values. (C) A “cut green pepper,” “soap bubble,” or “Swiss cheese” appearance has been described in radiation necrosis, although this usually does not allow reliable discrimination between these processes. (D) Decreased FDG uptake on PET favors radiation necrosis. False negatives may occur in the presence of a large area of necrosis.
C HIV encephalopathy
HIV encephalopathy is the most common central nervous system infection related to the HIV virus. Although the incidence of frank dementia has decreased substantially following the advent of highly active antiretroviral therapy, the prevalence of mild to moderate cognitive deficits in this population has increased and probably is at least partially related to longer survival. Note the prominent cerebral volume loss for the patient’s age, lack of mass effect, and symmetric confluent white matter signal abnormalities that spare the U fibers. (A) Lymphoma would have some degree of mass effect and would be more focal than the image demonstrates. Lymphoma in patients with HIV/AIDS commonly has central necrosis, whereas lymphoma occurring in the nonimmunocompro-mised population is diffusely solid and enhances homogeneously. (B) Progressive multifocal leuko-encephalopathy usually is bilateral but asymmetric. When there are subcortical signal abnormalities, they virtually always involve the U fibers; note that these are spared in this case and are seen as dark gray bands between the cortex and the bright white matter lesions. (D) Cerebritis would present with variable degrees of gray and white matter edema.
D Flexion/extension sequences
Flexion/extension sequences are important in the evaluation of Hirayama disease (monomelic amy-otrophy), as they would demonstrate detachment and anterior displacement of the dura on neck flexion, with resultant spinal cord compression and myelopathy. Hirayama disease is a benign and self-limiting disease that usually occurs in patients between 15 and 25 years of age. (A) Gradient echo sequences in the spine are useful to differentiate disks from osteophytes and to demonstrate foci of hemorrhage within the cord. These sequences also are less prone to cerebrospinal fluid pulsation artifact. (B) Routine postcontrast sequences help delineate the enhancing epidural space in Hirayama disease and may facilitate identification of the dura. Delayed contrast sequences are not particularly helpful. (C) Diffusion-weighted sequences are technically difficult to acquire in the spine. They may be useful in the evaluation of acute spinal cord ischemia and spinal infection.
B Tuberculous spondylitis
Tuberculous spondylitis (also known as Pott disease) originates in the end plates and typically spreads in a subligamentous fashion to involve the adjacent vertebrae, frequently, but not always, sparing the intervertebral disks, as seen in this case. The provided contrast-enhanced T1 image shows a dark lesion (presumably fluid/pus) with peripheral enhancement. There also is enhancement of the adjacent vertebra above with preservation of the intervening disk. Tuberculous spondylitis has a higher incidence of extensive paraspinal abscess formation compared with pyogenic infections. Its onset tends to be insidious and gradual, which not uncommonly leads to a delayed diagnosis. Constitutional symptoms including fever and weight loss are seen in less than 40% of cases. (A) Pyogenic osteomyelitis typically involves the intervertebral disks. In children, infection is thought to start in the disks, with secondary involvement of the adjacent vertebrae. In adults, the disease is thought to start in the end plates, with involvement of the disks in the majority of cases. (C) Degenerative disk disease would be centered in the intervertebral disk spaces and may result in secondary degenerative changes in the adjacent end plates. (D) Osseous metastases usually enhance and tend to involve the pedicles and posterior elements. They would not show the cystic appearance of the larger lesion seen in the provided image.
C Acute extravasation
The “swirl” sign is seen on noncontrast head CT and is defined as areas of low attenuation within an acute intracranial hematoma. It indicates freshly extravasated and unclotted blood and is associated with expansion of the hematoma and a worse prognosis. (A) Thrombosis can present as a hyper-dense clot on noncontrast head CT or a filling defect following the intravenous administration of contrast material. (B) Malignant transformation can occur in various neoplasms. It is not associated with a “swirl” sign. (D) An abscess presents as a fluid collection with an enhancing wall and surrounding edema. MRI shows central restricted diffusion. It is not associated with a “swirl” sign.
A Cytokine release and production of muco-polysaccharides
Thyroid orbitopathy can affect any extraocular muscle, but the most typical presentation is that of involvement of the inferior, middle, and superior rectus muscles, which are markedly enlarged in this case. Involvement of the lateral rectus muscle almost never occurs in isolation. The pathophysiology is thought to be related to lymphocytic infiltration and cytokine release, which stimulates fibroblasts to produce mucopolysaccharides and, in turn, leads to soft tissue edema due to a hyperosmolar shift. (B) The most common primary tumors to metasta-size to the orbit are breast, lung, prostate, and melanoma. It would be unusual for orbital metastases to result in this symmetric appearance of extraocular muscle enlargement. (C) IgG4-related disease of the orbit is being increasingly recognized as a cause of “idiopathic” inflammatory pseudotumor. It can be bilateral and involve any orbital structure, including the extraocular muscles, lacrimal sac, and optic nerve sheath complex. (D) Lymphoma may present as a soft tissue mass frequently related to the lacrimal gland or conjunctiva (MALT lymphoma). Other orbital structures also may be involved.
D Mediastinal deviation to the contralateral side
A tension pneumothorax is accompanied by shift of the mediastinal structures to the contra-lateral side due to a progressive mass effect. (A) The diaphragm typically is flattened and depressed on the side of the tension pneumothorax. (B) The ipsi-lateral (not contralateral) intercostal spaces increase secondary to increased intrathoracic volume and pressure on the side of the tension pneumothorax. (C) The “deep sulcus” sign may be seen in pneumo-thoraces on supine radiographs, as air collects basally and anteriorly rather than at the apex in an upright projection. It does not necessarily reflect a tension pneumothorax. (E) As with mediastinal structures, the trachea may be deviated to the con-tralateral side in tension pneumothorax.
A Paget disease
Paget disease is a disorder of uncertain etiology where there is excessive bone remodeling and overgrowth. It most commonly occurs in the spine, skull, and pelvis. In the osteosclerotic phase, there is cortical thickening and coarsening of the trabec-ulations, which often lead to expansion of the involved bone. In the spine, the vertebrae become squared, and a thick, sclerotic margin may be seen, resulting in the “picture frame” sign. (B) Vertebral hemangiomas can lead to increased vertical trabec-ulations that may be seen as dense dots on axial images. (C) Lytic metastases do not cause a “picture frame” appearance. (D) Blastic metastases can produce the “ivory vertebra” sign if they involve the entire vertebral body. Blastic metastases can be seen in various malignancies such as prostate and breast cancer, transitional cell carcinoma, and neuroendocrine tumors.
A Posterior limb of the internal capsule
The arrows point to the anterior choroidal arteries, which originate between the posterior communicating arteries and the carotid termination. The posterior communicating arteries can be seen immediately medial to these on the provided image. The anterior choroidal arteries supply the posterior limbs of the internal capsules, lateral geniculate nuclei, optic tracts and chiasm, hippocampi, amygdalae, and choroid plexus, among other structures. (B) The anterior limb of the internal capsule (lower half) is supplied by the recurrent artery of Heub-ner, which is a branch of the proximal anterior cerebral artery. The upper half is supplied by the lateral lenticulostriate arteries. (C) The anterome-dial caudate nucleus as well as the anterior portion of the lentiform nucleus are supplied by the recurrent artery of Heubner. (D) The external capsule is supplied by the lateral lenticulostriate arteries, which are branches of the proximal middle cerebral artery and also supply the lateral aspect of the putamen and upper half of the internal capsule. (E) The various vascular territories of the thalamus all are supplied by branches of the posterior cerebral and posterior communicating arteries.
B High incidence of neurovascular injury
The sagittal CT image shows too much space between the dens and tip of the clivus (basion-dens interval) consistent with atlanto-occipital dissociation. This is a severe craniocervical injury that results from sudden deceleration, with hyper-flexion or hyperextension of the head, which disrupts the alar, cruciate, and apical ligaments and tectorial membrane. The condition is fatal in the great majority of patients secondary to a high incidence of neurovascular injury. (A) Atlanto-occipital dissociations are two to three times as common in children as in adults, presumably due to their relatively large head sizes, small size of their occipital condyles, and near horizontal orientation of the atlanto-occipital joints. (C) Other less severe injuries such as the Jefferson fracture may occur secondary to axial loading. (D) Atlanto-occipital dissociation injuries may be identified by a basion-dens interval greater than 12 mm as originally measured on lateral cervical spine radiographs. One study suggest a lower cutoff value (8.5 mm) with CT imaging, due to the presence of magnification on plain radiography.
B Headache
Leptomeningeal carcinomatosis occurs in about 5% of patients with metastatic cancer and portends a poor prognosis. Half of these patients present with headaches, which represent the most common clinical manifestation. The incidence of leptomeningeal carcinomatosis is four times higher in autopsy studies. (A) Meningismus is present in 13% of patients with leptomeningeal metastases. (C) Ischemia is an uncommon complication of leptomeningeal carcinomatosis. In contrast, tuberculosis can manifest with leptomeningeal disease that characteristically results in cerebral infarcts. (D) Diabetes insipidus can occur in patients with infundibular involvement but is much less common than headache. It also is more frequently seen in leukemic patients rather than in patients with solid tumor leptomeningeal disease. (E) Dysarthria is an uncommon complication that occurs in 7% of patients with leptomeningeal metastases.
D Leptomeningeal cyst
The CT shows a cyst-like structure projecting through a calvarial defect. The T2 image better demonstrates that there is encephalomalacia in that area of the brain, and therefore findings are compatible with a leptomeningeal cyst. These findings develop from fractures with associated dural tears and herniation of the pia-arachnoid through the dural defect, with progressive osseous erosion (also known as a “growing” skull fracture) due to cere-brospinal fluid pulsations. (A) Langerhans cell his-tiocytosis is an important cause of a lytic calvarial defect in a child. Given the underlying encephalomalacia demonstrated, findings are more likely related to prior trauma. (B) An epidermoid can be primarily calvarial, but there is no evidence of it on the MRI shown in these images, which instead shows underlying encephalomalacia. (C) The T2 image demonstrates encephalomalacia and no evidence of an abscess or parenchymal edema. Additionally, an abscess would not result in a calvarial defect.
A Commonly produces a chondroid matrix
The CT image shows a destructive lesion involving the left petrous apex and petroclival junction, with contrast enhancement on the MRI study. There are small, calcific densities within it that could represent either chondroid matrix or eroded bone. Of the provided options, this lesion is most consistent with a chondrosarcoma, which comprises a heterogeneous group of malignant neoplasms characterized by the production of a chondroid matrix (sometimes seen as “rings” and “arcs” within a lytic lesion). About 1% of chondrosarcomas occurs at the skull base and commonly slightly off mid-line at synchondroses such as the petroclival and spheno-occipital sutures. (B) Cholesterol granulo-mas are thought to arise secondary to repeated episodes of hemorrhage within mucosa-lined air cells. They consist of granulation tissue and cholesterol crystals and typically are hyperintense on noncontrast T1-weighted images with areas of T2 hypointensity related to blood products. (C) In trapped secretions, the air cell septations are preserved, and there would not be erosive changes or an expansile enhancing lesion. (D) Aberrant ectoderm within petrous apex cells may result in a cholesteatoma, which does not enhance and usually is very bright on diffusion-weighted sequences due to a combination of restricted diffusion and T2 shine-through effects. (E) The vast majority of chondrosarcomas are slow-growing WHO grade I or II neoplasms that do not show significant restricted diffusion.
C Widening of the spinal canal on a midsagittal image
Anterior listhesis secondary to pars defects (but not due to facet hypertrophy) often results in widening of the spinal canal on a midsagittal image. (A) Small size or hypoplasia of the L5 vertebra may predict the presence of bilateral pars interarticu-laris defects and should prompt a search for them. (B) Sclerosis of the contralateral pars interarticu-laris can occur with a chronic unilateral pars inter-articularis defect. This patient likely has bilateral defects as indicated by significant listhesis of L5 over S1. (D) There may be variable degrees of neural foraminal narrowing depending on the severity of the listhesis, as can be seen on this image.
D Vasospasm
The reconstruction from the CT angiogram on the left shows marked vasospasm affecting the left greater than right middle cerebral and posterior cerebral arteries and bilateral anterior cerebral arteries. There are accompanying regions of decreased perfusion most evident in the left middle cerebral and bilateral anterior cerebral arteries, where there are acute infarctions. Clinically significant vasospasm after subarachnoid hemorrhage is seen in 30% of patients and is associated with increased mortality. (A) Embolic infarcts are a known complication of angiography, which likely was done in this patient with aneurysmal sub-arachnoid hemorrhage, but they tend to be small and usually are located peripherally at the gray matter-white matter junction. (B) Vasospasm following subarachnoid hemorrhage is thought to be related to the release of spasmogenic factors during lysis of subarachnoid blood clots and not due to cerebritis. (C) Venous thrombosis may result in ischemia but is not a primary complication of subarachnoid hemorrhage and would not result in the territorial arterial perfusion deficits seen in this case (primarily bilateral anterior cerebral and left middle cerebral arteries).
B It may show abnormal MRI signal in engorged pial vessels.
The MRA (left) demonstrates extensive collater-alization in the region of the proximal middle cerebral arteries due to bilateral intracranial carotid artery stenoses in a patient with (true or idio-pathic) moyamoya disease. The more distal middle cerebral arteries and visualized anterior cerebral arteries are abnormally narrowed in this case with preservation of the posterior circulation. Moyamoya disease may show abnormal signal in engorged pial vessels due to collateral flow through leptome-ningeal anastomoses (the “ivy sign”). Moyamoya syndrome or secondary moyamoya (different from moyamoya disease) is a nonspecific radiographic finding that can show a similar pattern of collat-eralization and may be seen in various entities including sickle cell disease, neurofibromatosis type 1, Down syndrome, and connective tissue disorders, among others. (A) Moyamoya disease has a bimodal age distribution with peaks between 5 and 9 years of age and 35 and 39 years of age. (C) The most common manifestations of moyamoya disease are ischemia and hemorrhage. There have been rare reports of dystonia and choreoathetosis. (D) Moyamoya disease much more commonly involves the anterior circulation, although the posterior circulation also may be affected.
B Commonly associated with focal cortical dysplasia
Dysembryoplastic neuroepithelial tumors (DNETs) are tumors of children and young adults who usually present with a long-standing history of intractable seizures. The lesions occur most commonly in the temporal followed by the frontal lobes, and these areas account for over 90% of cases. DNETs commonly are associated with focal dysplasia in the adjacent cortex. On imaging, they characteristically show a bubbly appearance, are cortically based, are bright on T2, and usually do not show contrast enhancement. Calcification is relatively common. (A) DNETs are WHO grade I lesions. (C) DNETs do not have restricted diffusion; therefore, they should not show low signal on apparent diffusion coefficient maps. (D) Only about 20% of DNETs show contrast enhancement in a nodular, heterogeneous, or ring-like fashion. (E) DNETs are slow-growing tumors that do not have a propensity for leptomeningeal spread.
The fornix is a white matter structure that connects the hippocampus and mammillary bodies. It features a blood-brain barrier and does not normally show contrast enhancement. (A, B, D, E) The circumventricular organs are small, highly vascu-larized, midline structures surrounding the third and fourth ventricles. They are devoid of a blood-brain barrier, which enables contrast enhancement to be demonstrated routinely in the larger organs. Enhancement of the smaller structures is more difficult to appreciate but has been documented to variable degrees in studies done on higher field magnets.
C Anterior inferior cerebellar artery
There is increased FLAIR signal along with restricted diffusion involving the anterior aspect of the right cerebellar hemisphere and middle cerebellar peduncle compatible with acute infarction. The abnormality follows the arterial distribution of the anterior inferior cerebellar artery, which also supplies the inferolateral aspect of the pons and flocculus. (A) The superior cerebellar artery supplies the superior cerebellum, superior vermis, dentate nuclei, and part of the midbrain. (B) The cerebellar parenchyma posterior to the infarcted area is supplied by the posterior inferior cerebellar artery (PICA) and is not involved. The PICA is the major artery of the cerebellum and supplies its posteroinferior portion, the inferior cerebellar vermis, and the lateral medulla. (D, E) The superior and inferior cerebellar veins drain their respective regions of the cerebellum and transmit blood to the dural sinuses and deep venous vasculature. The infarct in this case shows an arterial distribution.
D Capillary telangiectasia
The imaging description of the lesion and its location are characteristic of a capillary telangiectasia. Low signal on GRE sequences is thought to be related to slow flow and increased deoxyhemoglo-bin content. Capillary telangiectasias sometimes can have areas of gliosis and are nearly always asymptomatic and found incidentally. (A) A demyelinating plaque does not show the constellation of features described, which are characteristic of capillary telangiectasias. (B) Capillary telangiectasias should be differentiated from metastases. The latter usually have surrounding edema (except for small cortical lesions) and do not show signal loss on gradient echo (GRE) imaging unless they are hemorrhagic, melanotic, or calcified. (C) Cavernous malformations can show various signal intensities depending on the stage of their blood products. They typically are described as having a “popcorn” or “berry” appearance with a surrounding rim of hemosiderin.
E Joubert syndrome
Joubert syndrome is characterized by vermian hypoplasia or aplasia and a lack of decussation of the superior cerebellar peduncles. Thickening and a more horizontal configuration of the superior cerebellar peduncles leads to a “molar tooth” appearance. Diffusion tensor imaging studies show a lack of the expected “red dot” of pyramidal decussation. Most cases are autosomal recessive. (A) Rhombencephalosynapsis is characterized by an absent vermis and midline continuation of the dentate nuclei, cerebellar hemispheres, and superior peduncles. (B) A Dandy-Walker malformation can result in cystic enlargement of the posterior fossa in communication with the fourth ventricle. It does not lead to a “molar tooth” deformity. (C) A Blake pouch cyst develops due to the persistence of the embryonic Blake pouch. It can exert mass effect on the posterior fossa structures. (D) A mega cisterna magna is an incidental finding that presents as an increased subarachnoid retrocerebellar space in the lower posterior fossa. It may be asymmetric and mistaken for an arachnoid cyst.
A Histologically consists of balloon cells with prominent nucleoli
The patient’s history and clinical examination are compatible with tuberous sclerosis. The facial rash represents multiple angiofibromas, which tend to occur in the malar region. The nodular plaques on the lower back are Shagreen patches, which are considered highly specific for this entity. MRI shows a mixed cystic and solid mass centered in the left foramen of Monro (location is typical) compatible with a subependymal giant cell astro-cytoma (SEGA) in this clinical context. There is resultant obstructive hydrocephalus, which is why the patient presented with signs of increased intra-cranial pressure. Other MRI findings of tuberous sclerosis include cortical tubers, subependymal nodules, and various white matter lesions. Histologically, SEGAs consist of balloon cells with prominent nucleoli, although spindle cells may be encountered and predominate in some tumors. Pathologically, they are indistinguishable from subependymal nodules, and on imaging, the only reliable differentiating feature is an increase in tumor size over serial studies (both subependymal nodules and SEGAs can enhance). (B) SEGAs are categorized as WHO grade I lesions. (C) SEGAs become symptomatic between 10 and 30 years of age but have been reported in patients as young as 11/2 years of age. It is unusually rare for a SEGA to develop after the age of 20, and, in fact, patients without this tumor by age 25 do not need continued surveillance, as per the International Tuberous Sclerosis Complex Consensus recommendations. In contrast, SEGAs diagnosed early may become symptomatic later, and lifetime monitoring may be required for such lesions. (D) Spontaneous malignant transformation of SEGAs has been described but is unusually rare. (E) A bubbly appearance on MRI and attachment to the septum pellucidum is a description that would fit a central neurocytoma.
B Craniopharyngioma
A heterogeneously enhancing suprasellar mass with cystic components and calcifications in a child (note that the spheno-occipital synchondro-sis has not yet fused) is a craniopharyngioma until proven otherwise. These tumors most commonly occur in children between 5 and 14 years of age (adamantinomatous type), with a second peak in adults between the ages of 50 and 75 years (papillary type). They arise from remnants of the cranio-pharyngeal duct and are histologically benign but locally aggressive. These tumors are almost always sellar/suprasellar, although they rarely may present as purely intrasellar or even intrasphenoid, within the third ventricle, or in the optic apparatus without a sellar component. They have solid, enhancing components and show calcifications on CT in 90% of cases. (A) Epidermoid tumors are rare in the pediatric population. Except for FLAIR and diffusion-weighted sequences, they are homogeneous, usually have a cystic appearance, and should not show enhancing solid components. (C) The suprasellar region is the second most common location for germinomas, which also tend to present in the pediatric population. Calcification is rare. (D) Aneurysms, in general, are rare in children. Aside from vascular enhancement of the lumen, they do not show solid enhancing components. They may show a calcified rim corresponding to the aneurysm wall, but they do not demonstrate the coarse, scattered calcifications seen in this case. (E) Pituitary adenomas are rare before puberty. They can be heterogeneous in the presence of cystic or hemorrhagic changes and may resemble craniopharyngiomas; however, calcification is rare in adenomas.
A Absent body of the corpus callosum
Syntelencephaly is also known as the middle interhemispheric variant of the holoprosenceph-aly spectrum. In this entity, there is nonseparation of the midportion of the cerebral hemispheres (posterior frontal and anterior parietal lobes) and absence or hypoplasia of the body of the corpus callosum. (B) The frontal and occipital poles characteristically are separated in syntelencephaly. (C) The sylvian fissure is present in syntelencephaly but has an abnormally vertical orientation and crosses the midline in the majority of patients. (D) An interhemispheric fissure is present in syntelencephaly, but is interrupted or intercepted by the sylvian fissure crossing the midline.
C It is formed by sheets of small round blue cells.
These images show characteristic features of a medulloblastoma as an enhancing mass in the region of the cerebellar vermis projecting into the fourth ventricle. The lesion demonstrates restricted diffusion, as evidenced by increased signal on diffusion-weighted imaging (center) and corresponding low signal on the apparent diffusion coefficient (ADC) map (right). Of the most common posterior fossa tumors, medulloblastomas have the lowest ADC values. They are formed by sheets of small round blue cells with minimal cytoplasm, hyperchromatic nuclei, and are similar to pineoblastomas and retinoblastomas. (A) Ependymal rosettes are characteristic of ependymomas. These are “plastic” tumors that may extrude through the fourth ventricular outflow tracts in a “toothpaste” configuration. They usually show less restricted diffusion than medulloblastomas. (B) Hemangioblastomas are low-grade, capillary-rich neoplasms that can occur sporadically or in the setting of von Hippel-Lindau syndrome. They are very vascular, enhance avidly, and may show vascular flow voids. Two thirds of them may present as a cyst with an enhancing nodule (typically abutting the pial surface), and the rest are entirely solid. (D) Rosenthal fibers are characteristic of juvenile pilocytic astro-cytomas. They also may be present in reactive glial tissue surrounding vascular malformations and slow-growing tumors. Rosenthal fibers have been described in pleomorphic xanthoastrocytomas and Alexander disease. The solid enhancing component of pilocytic astrocytomas usually does not demonstrate much restricted diffusion.
A Lesions commonly occur at gray matter-white matter junctions.
Lesions in neurocysticercosis commonly occur at gray matter-white matter junctions due to he-matogenous spread. In the racemose form, there is proliferation of lobulated cysts without a scolex, which may spread throughout the subarachnoid space and ventriculoependymal surfaces. (B) Neurocysticercosis is acquired by ingesting Taenia solium eggs shed in the feces of carriers infected with the adult tapeworm. Ingestion of undercooked pork does not cause cysticercosis but may result in taeniasis with proliferation of the adult tapeworm in the small intestine. (C) Contrast enhancement is not seen in the vesicular stage, as the organism’s membrane still is intact. There also is no surrounding edema, and patients usually are asymptomatic. Once the cyst degenerates and dies, it incites an inflammatory reaction, edema, and contrast enhancement (colloidal vesicular stage) followed by involution in the granular nodular stage, where there may be a nodular or ring enhancing lesion with a thick capsule. In the final stage (nodular calcified), the lesions calcify, and there usually is no contrast enhancement. (D) Neurocysticercosis is the most common parasitic infection of the central nervous system in immunocompetent patients. Its incidence is not increased in AIDS. (E) Spinal cord involvement is rare and occurs in about 1% of cases.
A Can result in vasospasm after rupture
T1-weighted images without intravenous contrast (note that the choroid plexus does not enhance) demonstrate a lesion in the left frontal lobe, which is intrinsically bright due to fat and compatible with a dermoid cyst. A fat-fluid level is seen (left image), which is characteristic. There also are scattered bright subarachnoid fat droplets in the sulci as well as intraventricular extension with fat in the frontal horns. Dermoid cysts derive from the intracranial inclusion of cutaneous ectoderm during closure of the neural tube and may develop after traumatic/iatrogenic implantation. In contrast to epidermoid cysts, they contain dermal appendages (sebaceous and sweat glands and hair follicles). Rupture is a rare event, and may result in chemical meningitis, seizures, vasospasm, and ischemia. Fis-tulous tracts may lead to recurrent bouts of bacterial meningitis. (B) Dermoid cysts contain dermal appendages (absent in epidermoid cysts). (C) Dermoid cysts may show a lipid peak from 0.9 to 1.3 ppm. Meningiomas (not dermoid cysts) may show increased alanine on MR spectroscopy at short TE values. (D) Chemical meningitis may occur after rupture of a dermoid cyst, which is in itself a rare event. (E) Rarely, dermoid cysts may degenerate into squamous cell carcinomas but not into high-grade glial tumors.
A More common in women
Pineal cysts are more common in women than in men, by a ratio of 3:1. Most pineal cysts measure less than 1 cm but may be larger, with lesions greater than 4 cm reported in the literature. They typically do not enhance, but may show a thin rim of enhancement peripherally. Very rarely, nodular areas of enhancement have been reported, in which case pineal cysts cannot be distinguished from pineal region tumors on the basis of imaging. Gadolinium will diffuse slowly into pineal cysts, and, given enough time, a pineal cyst may show enhancement on delayed imaging. The majority are asymptomatic, but approximately 5% can compress the cerebral aqueduct and result in hydro-cephalus. Size tends to be stable in males, but pineal cysts may grow in young females with later regression, suggesting a hormonal role in their development. (B) Pineal cysts usually do not suppress fully on FLAIR sequences. (C) Pineal cysts do not show restricted diffusion. (D) The majority of pineal cysts are asymptomatic. (E) Pineal cysts are lined by a thin layer of glial cells, fibrous tissue, and pineal parenchyma with or without calcifications.
C Flow voids
As with paragangliomas occurring in the neck, lesions are highly vascular, enhance avidly, and may be associated with hemorrhage. Flow voids can be seen in and around the lesion. (A) The “target” sign has been described on T2 images in neurofibromas due to a dark fibrocollagenous core. It may be seen less commonly in schwannomas probably due to the relative distribution of Antoni A and Antoni B tissues. (B) Intrinsic T1 hyperintensity sometimes can be seen in myxopapillary ependymomas, which is the other major differential diagnosis in the lumbar spine. (D) Paragangliomas are extramedullary and usually occur in the region of the filum terminale and cauda equina; therefore, they do not expand the cord, although on occasion, there may be an associated intramedullary cyst.
C Gray matter heterotopia is present in 10 to 30% of cases.
The image accompanying the question shows the typical imaging features of a Chiari type 2 malformation, with descent of the brainstem through the foramen magnum, a small posterior fossa, beaking of the tectum, a flattened and elongated fourth ventricle, and a thinned/dysplastic corpus callosum. Gray matter heterotopia is seen in 10 to 30% of cases, predominantly in a periventricular distribution. (A) Virtually 100% of Chiari type 2 malformations are associated with “open” spinal dysraphism (not “closed” as with a skin-covered defect). The presence of a skin-covered myelome-ningocele essentially excludes the development of a Chiari type 2 malformation, and this is the reason why some myelomeningoceles are corrected in utero. (B) This option refers to a Chiari type 1 malformation, which presents with inferior herni-ation of peg-like cerebellar tonsils and is usually not clinically significant unless the tonsils are displaced more than 5 mm below the foramen magnum. (D) A “monoventricle” may be seen in holopros-encephaly depending on its severity. This is not a feature of a Chiari type 2 malformation.
D Peripheral nerve sheath tumor
The pathology shown in the images accompanying the question is an extramedullary neoplasm that is partially intradural and partially extradural. It extends to the paraspinal soft tissues through the left neural foramen, which is expanded and remodeled, indicating that this is a slow-growing process. Findings are most consistent with a nerve sheath tumor. The presence of a T2 dark center (i.e., the “target sign” due to a fibrocollagenous core) in the lower image suggests a neurofibroma, although schwannomas sometimes can show a similar appearance, depending on the relative distributions of Antoni A and Antoni B tissues. (A) Paragangliomas are rare in the spine. They tend to occur in the conus medullaris and filum terminale. (B) Ependymomas usually are parenchymal except for the myxopapillary type, which occurs exclusively in the filum terminale and sometimes involves the conus medullaris. (C) Meningiomas in the spine are much more common in females and more frequently occur in the thoracic spine. They are dural-based masses, but on occasion may extrude through a neural foramen.
C Increased risk of hemorrhage expansion
The “spot sign” indicates a focus of active extravasation and predicts the expansion of a parenchymal hematoma. It is seen as a single focus or multiple foci of enhancement within the hematoma, and is present in about one third of patients within the first 6 hours after symptom onset. Other factors that have been associated with increasing hemorrhage size include large initial volumes and the use of anticoagulants. (A, B, E) The “spot sign” does not indicate the presence of a neoplasm, arte-riovenous malformation, or arteriovenous fistula, although all of these may be associated with parenchymal hemorrhage. (D) The “spot sign” can be seen in, but is not exclusive to, hypertensive hemorrhage.
B Pulmonary edema
This constellation of radiographic findings is most consistent with pulmonary edema. Blunting of the costophrenic angles reflects the presence of pleural effusions. Kerley lines represent thickening of the interlobular septa and pulmonary inter-stitium, and may be seen with edema, lymphatic engorgement, or carcinomatosis. Potential causes of postoperative pulmonary edema are varied and can be related to over-administration of intravenous fluids, neurogenic edema, acute respiratory distress syndrome (ARDS), hyponatremia, sepsis, and other causes. (A) Pneumonitis is a general term with various etiologies indicating alveolar inflammation, which may or may not result in pulmonary edema. (C) Aspiration pneumonia most commonly occurs in the posterior segment of the upper lobes and the superior segment of the lower lobes in postoperative patients who usually are recumbent. (D) Pneumonia usually is focal but may be extensive and bilateral if it is severe.
A Leptomeningeal angiomatosis
The description of this case is consistent with Sturge-Weber syndrome, the hallmark of which is disorganized capillary vascular malformations involving the face, eye, and brain, typically on the same side. Leptomeningeal enhancement reflects the presence of a pial angiomatosis, which more commonly occurs in the parieto-occipital region and is thought to lead to cortical/subcortical calcifications due to a steal phenomenon and chronic ischemia. Patients may develop seizures, hemi-plegia, and visual deficits. The pial angiomatosis is bilateral in 20% of cases where the clinical presentation is more severe. (B) In Sturge-Weber syndrome, there is engorgement of the ipsilateral choroid plexus and often recruitment of ependymal collaterals. (C) The facial capillary malformation of Sturge-Weber syndrome (“port-wine” stain) typically involves the ophthalmic division and sometimes the maxillary division of the trigeminal nerve. It virtually never involves the mandibular division in isolation. (D) The ipsilateral frontal sinuses may be enlarged due to the compensatory growth of the calvaria, sometimes resulting in the Dyke-Davidoff-Masson phenomenon (compensatory thickening of the cranial vault with frontal sinus enlargement, elevation of the petrous ridge, ipsilateral falcine displacement, and capillary malformations). (E) There is compensatory thickening of the ipsilateral calvaria in chronic cases of Sturge-Weber syndrome due to the hemiatrophy.
C Pseudocysts
Gelatinous pseudocysts are a characteristic finding of cryptococcal meningoencephalitis and are filled with mucous exudates produced by the fungus. The pseudocysts commonly occur in the basal ganglia and medial cerebellum. Because they are not simple fluid, they do not suppress on FLAIR sequences. Patients also can have enhancing cryp-tococcomas and dilated perivascular spaces. (A) A concentric T2 FLAIR “target” sign is seen in one third of patients with toxoplasmosis, and represents alternating layers of necrosis, edema, and hemorrhage. (B) The eccentric “target” sign is seen on contrast-enhanced T1-weighted images, and is highly suggestive of toxoplasmosis (seen in about one third of patients with the diagnosis). (D) Low T2 signal intensity can be seen in enhancing gran-ulomas, including cryptococcomas and tuberculo-mas but is not specific.
B Hand and arm dysesthesia
The coronal CT image shows large cervical ribs arising from the C7 vertebrae bilaterally. They may constitute a cause of thoracic outlet syndrome. By far, the most common clinical manifestations of thoracic outlet syndrome are neurogenic (about 95%), and include pain, dysesthesias, weakness, and cold intolerance in the hands, arms, or shoulders. Most commonly, neurogenic thoracic outlet syndrome involves the C8 and T1 cervical roots, which may result in symptoms along the ulnar nerve distribution. Less commonly, the upper cervical brachial plexus roots may be affected and lead to symptoms in the neck, upper chest, and back. (A) Signs and symptoms of arterial compression with or without thromboembolism, including hand ischemia, are the least common presentations of thoracic outlet syndrome, constituting approximately 1% of cases. (C) Muscle atrophy can be seen in cases of severe and prolonged compression of the brachial plexus, but this is extremely uncommon. (D) Upper extremity swelling may be a manifestation of venous compression and/or thrombosis; however, neurogenic symptoms are more common manifestations of thoracic outlet syndrome. (E) Chronic venous compression can lead to the development of collateral veins, but neurogenic symptoms are more common in thoracic outlet syndrome.
B TSC1/TSC2
The constellation of findings presented is compatible with tuberous sclerosis complex (TSC). In particular, the combination of glioneuronal hamartomas (also known as cortical tubers) and subependymal nodules is sufficient to make the diagnosis as per the 2012 TSC Consensus Guidelines. White matter radial migration lines and parenchymal cysts also are characteristic. TSC can develop due to mutations in either the TSC1 or TSC2 genes, which code for hamartin and tuberin. (A) Neurofibromatosis type 1 can lead to various lesions in the central nervous system, including gliomas, sphenoid wing dysplasias, and focal areas of high signal intensity (FASI), also known as unidentified bright objects (UBOs). (C) Neurofibromatosis type 2 is characterized by the presence of multiple inherited schwannomas, meningiomas, and ependymomas (MISME). (D) The hallmark central nervous system lesions in von Hippel-Lindau disease are hemangioblastomas, which are very vascular and invariably enhance; two thirds present as typical, cystic masses with mural nodules, and the rest are entirely solid. Patients also can develop endolymphatic sac tumors as well as various extra-cranial lesions. (E) Mutations in the SMARCB1 and LZTR1 genes have been associated with schwanno-matosis (neurofibromatosis type 3).
B Dural venous thrombosis
Dural venous thrombosis can lead to the so-called empty delta sign, due to the presence of a nonenhancing thrombus in the dural venous sinus against a background of enhancing blood in the surrounding sinus/dura. (A) Cortical vein thrombosis does not result in an empty delta sign. Depending on bolus timing, it can be seen as a filling defect on a contrast-enhanced study, hyper-intensity within the vessel on FLAIR sequences, or associated blooming artifact on gradient echo-based sequences (particularly susceptibility weighted imaging). (C, E) Dense subdural or subarachnoid blood along the posterior falx and dural reflections can cause a “pseudo-delta” sign on a noncontrast CT study. (D) Deep venous thrombosis does not cause an empty delta sign.
D Dorsal arachnoid web
The “scalpel” sign has been described in dorsal thoracic arachnoid webs and refers to the shape of the dorsal subarachnoid space at the level of the lesion. MRI and CT myelography show ventral displacement of the spinal cord due to the presence of an abnormal arachnoid membrane. Dorsal thoracic arachnoid webs can be associated with symptoms of long-standing cord compression. (A) Epidural hematomas can exert mass effect on the intra-spinal structures. They are not associated with the “scalpel” sign. (B) Spinal cord herniation is thought to be caused by a dural defect, with resultant communication between the subarachnoid and epidural spaces. The spinal cord progressively her-niates through the defect, with subsequent distortion and potential development of myelopathy. (C) An arachnoid cyst can result in variable degrees of mass effect on the spinal cord.
C Antiepileptic drug usage
Antiepileptic drug usage and sudden withdrawal of antiepileptic drugs have been linked to transient splenic lesions. Various infectious, inflammatory, and autoimmune processes have been associated with a transient splenic lesion. The etiopathogen-esis is uncertain. (A) A demyelinating plaque can occur in the corpus callosum but more commonly is asymmetric, and follow-up imaging may show the sequela of demyelination. (B) The corpus callosum is relatively resistant to embolic infarcts, due to the perpendicular orientation of its penetrating arteries and a rich blood supply. It would be unusual for an embolic infarct to occur at the midline. (D) Acute disseminated encephalomyeli-tis can affect the corpus callosum but usually is asymmetric.
C FGFR
There is trigonocephaly resulting from premature fusion of the metopic suture, which usually closes at 6 to 12 months of age. This deformity can result in ridging along the forehead, bifrontal and bitemporal narrowing, and hypotelorism. Most cases of trigonocephaly are sporadic, and the majority of nonsyndromic cases may be related to a variety of genetic and environmental factors. Trigonocephaly may be associated with many syndromes such as Jacobsen, Saethre-Chotzen, Opitz C, and Say-Meyer, among others. Most syndromic cases are related to mutations in the FGFR genes, but alterations also may be seen in chromosomes 9, 11, and 22. (A) TSC1 and TSC2 mutations are the hallmark of tuberous sclerosis complex. (B) NOTCH3 mutations can result in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. (D) Mutations in the SMARCB1 gene can lead to Coffin-Siris syndrome and an increased risk of developing rhabdoid tumors such as ATRT.
B Arachnoiditis
An “empty sac” sign has been described in arachnoiditis due to peripheral displacement of nerve roots that are adherent to the sac. Nerve roots also can be clumped, and there rarely may be soft tissue masses in patients with fibrosing or ossifying arachnoiditis. Although most cases are postsurgi-cal, arachnoiditis also may be seen after infection, trauma, subarachnoid hemorrhage, and intrathe-cal steroids. (A) An arachnoid cyst appears as a well-circumscribed filling defect within the thecal sac and can result in displacement of the spinal contents. If there is communication with the sub-arachnoid space, an arachnoid cyst eventually will fill with contrast and may become invisible on delayed imaging; 80% of spinal arachnoid cysts are thoracic, and only 5% are lumbar. (C) An intradural tumor can displace the spinal nerve roots but does not produce an “empty sac” sign. (D, E) Epidural and subdural collections can result in variable degrees of mass effect on the thecal sac and its contents.
D Auriculotemporal nerve
The auriculotemporal nerve arises from the posterior division of the mandibular branch of the trigeminal nerve. It anastomoses with the tempo-rofacial division of the facial nerve and is a common route of perineural spread, particularly from tumors in the temporal scalp, parotid gland, and external auditory canal. (A) The maxillary nerve is the second division of the trigeminal nerve. Perineural spread along this nerve can occur from malignancies arising in the facial region. (B, C) The greater superficial petrosal nerve is a branch of the facial nerve that arises from the geniculate ganglion. The Vidian nerve is formed by the confluence of the greater superficial petrosal nerve, deep petrosal nerve, and ascending sphenoidal branch from the otic ganglion. These are potential routes of spread in various tumors from the nasopharynx, paranasal sinuses, and orbits.
A Metastasis
The images accompanying the question demonstrate an intra-axial mass in the left cerebellum with peripheral enhancement (left) and restricted diffusion of the enhancing component as evidenced by high signal on the diffusion-weighted image (center) and dark signal on the apparent diffusion coefficient map (ADC, right), which also demonstrates increased surrounding signal due to edema. Metastases constitute the most common cerebellar tumors in adults. (B) Primary cerebellar glioblastomas are rare and constitute less than 1% of all such tumors. Solid components may show restricted diffusion. (C) Tumefactive demyelination may present as an enhancing mass, typically with an incomplete ring of enhancement that may show variable degrees of restricted diffusion. (D) Abscesses show restricted diffusion in the central necrotic component, not in the enhancing peripheral rim. (E) Cerebral toxoplasmosis is an AIDS-defining condition, and most cases are seen in this context. Toxoplasma lesions tend to be small (2 to 3 cm) and commonly occur in the gray matter-white matter junction of the supratentorial brain and deep gray nuclei. They may show enhancement with an eccentric nodule (the “eccentric target” sign) or alternating rings of T2/FLAIR hypo- and hyperintensity related to areas of necrosis, edema, and hemorrhage.
A Originates from arachnoid meningothelial cells
1p36 deletions have been found in a variety of human cancers. In the central nervous system, these cancers include meningiomas, oligodendro-gliomas, and neuroblastomas. Of these, an avidly enhancing intraventricular mass would be most consistent with a meningioma, which originates from arachnoid meningothelial cells. In meningiomas, 1p deletions are the second most common genetic abnormality after deletions on chromosome 22, and they have been associated with an increased risk of tumor recurrence and progression. (B) The incidence of meningiomas increases with age. They are very rare in the pediatric population except when they are associated with neurofibromatosis type 2, in which case they more frequently develop at an earlier age or in patients with a history of radiation therapy, although the latency in such cases may be long. (C) Hamartin is a ubiquitous protein encoded by the TSC1 gene in the tuberous sclerosis complex, where it is associated with the development of hamartomas in various tissues. It is not related to the formation of meningiomas. (D) Ependymomas, not meningiomas, arise from the ependymal lining of the ventricular system. (E) Except for a few isolated reports of papillary and rhabdoid meningiomas, these tumors do not show glial fibrillary acidic protein staining.
D Endocarditis
Mycotic pseudoaneurysms form after infectious disruption of all three layers of the arterial wall and formation of a vascular outpouching. These lesions characteristically arise from distal branches of the middle cerebral artery along the surface of the brain and can develop as a complication of endocarditis and septic emboli, as was the case in this patient. (A) The pathogenesis of intracranial aneurysms is complex and multifactorial. Atherosclerosis may play a role in the formation of at least some fusiform aneurysms. The lesion in this case is very peripheral, almost along the inner table of the skull (note the faint subtraction artifact related to the calvaria), a location that is more often seen in mycotic pseudoaneurysms. (B) The imaging presentation of vasculitis is variable, and in many cases the angiogram may be normal and, therefore, does not rule out the diagnosis. The classic finding in vasculitis is regions of segmental stenosis and dilatation resulting in a “string of beads” appearance. (C) Mycotic pseudoaneurysms are infectious in nature.
B Methanol intoxication
The most characteristic imaging finding of methanol intoxication is bilateral putaminal necrosis with variable degrees of hemorrhage, and this may be accompanied by white matter edema or necrosis in severe cases. Findings are thought to be caused by the direct toxic effects of methanol metabolites and metabolic acidosis. Necrosis of the retinae and optic disks/nerves may lead to blindness. (A) The most common findings in sporadic Creutzfeldt-Jakob disease are cortical and basal ganglia signal abnormalities involving the corpus striatum. The variant form more commonly shows involvement of the pulvinar or dorsomedial thalami (“hockey-stick” sign). (C) Carbon monoxide intoxication typically affects the globus pallidus and also may involve the white matter. (D) Wernicke encephalopathy preferentially affects the mammillary bodies, medial thalami, tectal plate, and periaqueductal gray. Contrast enhancement of the thalamus and mammillary bodies has been associated with alcohol abuse.
A Often respects cranial sutures
The CT image shows a hyperdense, acute epidural hematoma with mass effect on the frontal lobe and mild midline shift. Classically, epidural hematomas are limited by tight dural attachments at the cranial sutures, which results in a lentiform or biconcave shape. They usually do not cross sutures unless there is a fracture or sutural dias-tasis. (B) Supratentorial subdural (not epidural) hematomas do not cross the midline because they are limited by the reflection of the inner layers of the dura as they form the falx cerebri. Epidural hematomas may cross the midline if there are no intervening sutures or if there is a sutural fracture or diastasis. This is seen, for instance, with vertex epidural hematomas, which usually are venous and associated with a fracture crossing the superior sagittal sinus and, therefore, can be seen across the sagittal suture. (C) Mixed density contents with areas of low attenuation within the dense hematoma (i.e., the “swirl sign”) indicate active extravasation and are an indication for emergent surgical evacuation. (D) 90 to 95% of epidural hematomas are due to an arterial injury. Epidural hematomas due to a venous injury are less common and usually are associated with fractures crossing the dural venous sinuses. (E) Epidural hematomas develop between the outer (periosteal) layer of the dura and the inner table of the skull.
B The majority are low-grade lesions.
The majority of tectal gliomas are low-grade lesions, but high-grade histologies also may be seen. (A) The vast majority of tectal gliomas are low-grade, insidious lesions that can be observed for relatively long periods of time without intervention. Shunting with an endoscopic third ventriculostomy or ventriculoperitoneal drainage generally is an accepted initial treatment. Tumors that persistently are symptomatic may require further treatment, such as radiotherapy and/or chemotherapy. (C) Aqueductal stenosis is the most common cause of congenital hydrocephalus and may be secondary to congenital stenosis of the cerebral aqueduct or a sequela of intrauterine infection. (D) Five to seven percent of patients with aqueductal stenosis have a congenital form (X-linked hydrocephalus) seen in males and determined by mutations in the L1CAM gene.
D Cerebrospinal fluid IgG and IgM oligoclonal bands
The axial FLAIR images accompanying the question show periventricular white matter lesions in a radial orientation, and two juxtacortical (abutting the cortex) lesions on the left side, characteristic of multiple sclerosis. The presence of both periventricular and juxtacortical lesions satisfies the 2010 modified MacDonald criteria for dissemination in space. The concurrent presence of an enhancing lesion (right image) and multiple nonenhancing lesions satisfies the criteria for dissemination in time. Oligoclonal bands are found in the cerebrospinal fluid in 95% of patients with clinically definite multiple sclerosis. (A) Serum aquaporin-4 antibodies are highly specific (between 92% and 99%) for the diagnosis of neuromyelitis optica and are seen in about 60% of patients. Lesions in the brain are not entirely specific, but tend to favor areas of high aquaporin-4 expression. White matter lesions with cloud-like enhancement and ependymal enhancement may be seen. (B) Cryptococcal antigen can be detected in the serum and cerebrospinal fluid of patients with cryptococcal meningoencephalitis. Cryptococcomas and gelatinous pseudocysts preferentially develop in the basal ganglia and medial cerebellum, and patients can have dilated perivascular spaces. (C) Lyme disease is caused by the spirochete Borrelia burgdorferi. MRI findings in the brain include nonspecific white matter lesions, which sometimes may enhance, and leptomeningeal and cranial nerve enhancement.
C Fibrous dysplasia
The CT image demonstrates osseous expansion and remodeling of the right maxilla, adjacent zygoma, and pterygoid process with a ground-glass appearance that is most consistent with fibrous dysplasia. This is a benign condition that develops as a result of abnormal osteoblastic differentiation and leads to replacement of normal marrow with immature osseous and fibrous elements. Fibrous dysplasia is a disease of children, adolescents, and young adults. It can be monostotic (80%) or polyostotic. In the head, the most common sites of involvement are the frontal, sphenoid, and ethmoid bones along with the maxilla. Although the majority of cases are sporadic, fibrous dysplasia can be seen as part of McCune-Albright and Mazabraud syndromes. On CT, the appearance is often characteristic with areas of ground-glass texture admixed with sclerotic and sometimes cystic changes. Diagnosis on MRI may be challenging, as the appearance is more variable. (A) Blastic (sclerotic) osseous metastases are seen with many primary malignancies including breast and prostate cancer and neuroendocrine tumors. They do not result in the expansile or ground-glass appearance seen in this case. (B) Paget disease essentially can occur in any bone and also can result in osseous expansion; however, it is a disease of middle-aged and elderly individuals. The ground-glass appearance of this case and the location are typical for fibrous dysplasia. (D) A plasmacytoma would have a destructive, lytic appearance on CT with or without a soft tissue component. It also is a condition seen in older individuals.
B Thin middle cerebellar peduncles
The “hot cross bun” sign is produced by degeneration of transverse pontine fibers and is highly specific for multiple system atrophy (MSA), although it only is seen in about half of the patients with this condition. The middle cerebellar peduncles are significantly thinned in MSA patients with predominant cerebellar ataxia, compared with patients with Parkinson disease and control individuals. (A) A molar tooth configuration is characteristic of Joubert syndrome, in which there is a lack of decussation of the superior cerebellar peduncles, which have a more horizontal trajectory. (C) The “hummingbird” sign is produced by midbrain atrophy with preserved volume of the pons in patients with supranuclear palsy. (D) Nonvisualization of the normal signal hyperintensity of nigrosome-1 has been described in patients with Parkinson disease using high field MR magnets.
D A dysplastic cerebellar gangliocytoma
A “corduroy” appearance is often used in MRI reports to describe the striated pattern that is highly characteristic of dysplastic cerebellar gangliocytoma (Lhermitte-Duclos disease). This is a hamartomatous formation occurring in the cerebellum that is seen in association with Cowden syndrome and loss of PTEN gene function. Patients are at an increased risk of developing various malignancies, including thyroid, breast, and endometrial cancer. The lesion may show increased signal on T2/FLAIR sequences and hyperperfusion. It also can be associated with increased mass effect and elevated intracranial pressure, which may necessitate ventricular decompression and/or surgical resection. (A) Cerebellitis typically does not result in a “corduroy” imaging pattern. It has various etiologies, and its presentation is varied. Cerebellitis can be unilateral, bilateral, symmetric, asymmetric, or diffuse. (B) A “corduroy” pattern is not typical of medulloblastoma; however, the desmoplastic variant of medulloblastoma features a multinodular architecture that may be confused with Lhermitte-Duclos disease. (C) Posterior inferior cerebellar infarcts are a known cause of mass effect in the posterior fossa and can be mistaken for tumor. They may enhance in the subacute phase, where striations may be seen related to the cerebellar folia; however, these striations tend to be thinner and more uniform than those of Lhermitte-Duclos disease.
C Increased perfusion on an MR relative cerebral blood flow map
Studies have shown increased relative cerebral blood flow (rCBV) perfusion in lymphoma compared with toxoplasmosis, although lymphomas commonly are hypovascular on perfusion imaging sequences. (A) The concentric T2 FLAIR “target” sign is characteristic of toxoplasmosis, and is produced by alternating rings of hemorrhage, edema, and necrosis within the lesion. It is present in approximately one third of cases. (B) The eccentric “target” sign is seen on contrast-enhanced T1 images and is highly suggestive of toxoplasmosis, although it is present only in about one third of cases. It is produced by a leash of inflamed leaky vessels coursing along a sulcus into the lesion. (D) Lymphomas show increased uptake of thal-lium-201, but the sensitivity decreases with small lesions, particularly those less than 2 cm. (E) Lipid/lactate peaks on MR spectroscopy previously have been suggested to imply toxoplasmosis; however, further studies have shown various spectral patterns in both lymphoma and toxoplasmosis without significant differences.
B Reversible cerebral vasoconstriction syndrome
The patient’s clinical presentation and imaging findings essentially are pathognomonic for reversible cerebral vasoconstriction syndrome. The angiogram was performed following an internal carotid injection and shows segmental multifocal narrowing involving both the anterior and posterior (through a fetal posterior cerebral artery) circulations. Initial CT and cerebrospinal fluid studies commonly are normal, although small-volume sub-arachnoid hemorrhage is present in 20% of patients with reversible cerebral vasoconstriction syndrome. Ischemic stroke, parenchymal hemorrhage, and areas of edema may be seen. (A) Venous infarction may present with headaches, nausea and vomiting, and altered mental status. It is not associated with recurrent “thunderclap” headaches. Additionally, only the arterial phase is shown on the angiogram. (C) There is no evidence of an aneurysm on the angiogram. (D) Acute vascular occlusion is not seen on this exam.
C Neuroblastoma
Neuroblastomas are tumors derived from primitive sympathetic ganglion cells. They most commonly occur in young children with a mean age of presentation of 22 months; 40% arise from the adrenal glands, and 15% are thoracic. When paravertebral, their growth results in remodeling of the adjacent vertebrae and ribs, and they can extend into the spinal canal through the neural foramina. They show heterogeneous enhancement and may be accompanied by cystic change and necrosis. Due to their adrenergic origin, they show avid uptake of 123I-metaiodobenzylguanidine (123I-MIBG), which has shown high sensitivity and specificity. (A) Giant cell tumors rarely occur in the vertebrae. They do not accumulate 123I-MIBG. (B) Eosinophilic granuloma is the localized and most common form of Langerhans cell histiocytosis. It can occur in the spine, where it usually affects the vertebral body and may result in a vertebra plana. (D) Aneurysmal bone cysts are histologically benign but may be locally aggressive. The presence of an expansile vertebral mass with thin bone rims and fluid–blood levels is nearly pathognomonic. They do not demonstrate 123I-MIBG uptake.
B Intravenous drug use
The sagittal T2 (left) and contrast-enhanced T1(right) MR images show the typical findings of diskitis/osteomyelitis with fluid/edema in an intervertebral thoracic disk and formation of an epidural abscess that extends dorsally into the spinal canal and compresses the cord. Note the extensive end-plate destruction and bone marrow edema in the adjacent vertebrae. Diskitis/osteomyelitis is more common in males, and its incidence increases with age. Risk factors include bacteremia (nosocomial or secondary to intravenous drug use), spinal procedures, direct inoculation from trauma, and various causes of immunosuppression including diabetes. (A) Metastatic disease usually spares the intervertebral disks and would not result in a fluid collection. Additionally, the bone marrow abnormality in this case is isolated to the vertebrae contiguous with the infected disk. (C) Fall from a height may result in a fracture, which would not explain the disk-centered inflammatory findings of this case. (D) Anemia, hypercalcemia, and renal failure are findings that would be expected with multiple myeloma, which is characterized by multiple lytic lesions that may have a permeative pattern on CT or radiography. Multiple myeloma can be seen as normal on MRI or may present as multiple hyperintense foci or with a variegated, micronodular pattern. (E) A seronegative (rheumatoid factor negative) spondyloarthropathy may present as inflammatory arthritis involving the spine and sacroiliac joints, with corner erosions in the vertebrae and ankylosis.
C Associated with hemorrhagic necrosis
Hemorrhagic necrosis is the pathological hallmark of HSV-1 encephalitis affecting primarily the limbic system and temporal lobes. The classic lesion distribution includes the mesial temporal lobes, insular cortices, and inferior frontal lobes. The abnormalities usually are bilateral but asymmetric, and MRI diffusion-weighted imaging and FLAIR sequences are the most sensitive to define their extension. Contrast enhancement is rare in the early stages of disease but may be present later along the gyri or leptomeninges. Prognosis is poor, with a high incidence of neurologic sequelae. Mortality is related directly to the time of initiation of acyclovir after disease onset. (A) Herpes simplex virus (HSV) encephalitis beyond the neonatal period is caused by HSV-1 in the majority of cases. Neonates can be infected with either HSV-1 or HSV-2 and usually present with a more diffuse type of encephalitis. (B) HSV-1 encephalitis typically spares the basal ganglia, but may cause middle cerebral artery strokes that could otherwise have a similar appearance to the image shown. (D) The majority of patients with paraneoplastic encephalomyelitis have antineuronal (anti-Hu) nuclear antibodies. The distribution of imaging abnormalities in limbic encephalitis may mimic that of HSV-1 encephalitis, but the clinical picture differs, with a more subacute progression of cognitive and behavioral changes and sometimes seizures in the former. (E) Diffuse infiltration of two or more lobes with neoplastic glial cells is the definition of gliomatosis cerebri. This potentially could mimic some of the signal abnormalities seen in HSV encephalitis but would not explain the acute presentation of symptoms in this patient.
A Fluid-attenuated inversion recovery
The two most relevant differential considerations for a nonenhancing, extra-axial, cystic mass are an arachnoid cyst and an epidermoid cyst. Arachnoid cysts follow cerebrospinal fluid signal intensity on all sequences and fully suppress on fluid-attenuated inversion recovery (FLAIR) sequences. Epidermoid cysts show a “dirty” appearance on FLAIR and very high signal intensity on diffusion-weighted sequences. (B) Susceptibility-weighted imaging (SWI) is a gradient echo MRI sequence that maximizes tissue differences by virtue of their local magnetic fields. SWI is highly sensitive to the presence of ferritin, calcium, deoxyhemoglobin, and hemosiderin, but does not play a role in characterizing arachnoid cysts. (C) Gradient recalled echo sequences generate images that are particularly susceptible to magnetic field inhomogeneities. Dynamic susceptibility contrast MRI and functional MRI are different techniques based on GRE sequences. (D) T2-weighted images would not be helpful, as both epidermoid tumors and arachnoid cysts will show high signal. (E) Dynamic susceptibility contrast perfusion would show only a nonperfusing, space-occupying lesion and would not aid in differentiation.
C Occipital lobe, thalamus, and part of the midbrain
This is a digital subtraction angiogram following an internal carotid injection. It shows a fetal origin of the posterior cerebral artery that supplies the occipital lobe, thalamus, and part of the midbrain. (A) The superior cerebellar artery supplies the superior cerebellum, superior vermis, dentate nuclei, and part of the midbrain. (B) The posterior inferior cerebellar artery supplies the posteroinferior cerebellum, inferior cerebellar vermis, and lateral medulla. (D) The anterior inferior cerebellar artery supplies the anterior aspect of the right cerebellar hemisphere, middle cerebellar peduncle, inferolateral aspect of the pons, and flocculus.
A Aneurysm
This is a well-circumscribed extra-axial lesion with mixed signal intensities and profound peripheral T2 hypointensity along the expected course of the posterior inferior cerebellar artery (PICA). Findings are most concerning for an aneurysm, which probably is partially thrombosed (note the enhancement of a nonthrombosed lumen on the third image). There is a small, old infarct in the left cerebellum seen on the FLAIR image likely related to thromboembolism. PICA aneurysms are rare, and the great majority arises proximally. (B) Although most meningiomas enhance homogeneously, they can calcify and sometimes present with cystic change or, very rarely, hemorrhage, and therefore they also may show variable signal intensities on MRI. Eighty percent of intraventricular meningiomas arise from the atrium of the lateral ventricle, and only 5% are seen in the fourth ventricle. (C) Eighty percent of choroid plexus tumors are benign papillomas. They are rare in adults, where they most commonly occur in the fourth ventricle. Papillomas tend to enhance avidly and diffusely and characteristically show frond-like margins with a texture that is similar to that of the normal choroid plexus. (D) Subependymomas are slow-growing tumors that commonly are seen in adults. They most commonly occur in the fourth ventricle, particularly at the obex followed by the frontal horns of the lateral ventricles. They typically do not enhance, but enhancement may be seen in a minority of them.
A Giant perivascular space
This lesion is formed by a cluster of cystic spaces that follow cerebrospinal fluid signal and fully suppress on FLAIR sequences. There is a small FLAIR hyperintense focus in the intervening parenchyma, consistent with gliosis, but no evidence of mass effect or any contrast enhancement. A somewhat branching pattern is present, which may be easier to appreciate on consecutive slices. Findings are most consistent with a giant or tumefactive perivascular space. Although headache is the most common complaint, its association with the presence of a giant perivascular space is uncertain. (B) Dysembryoplastic neuroepithelial tumors can have a bubbly appearance, and most do not enhance. These lesions are centered in the cortex, and there usually is some identifiable mass effect. Note that the cortex is thinned but not primarily involved in this case. (C) Metastases almost always have some degree of contrast enhancement. A lesion of this size also should have considerable surrounding edema. (D) A cystic glioma would be associated with enhancing components or with nonenhancing infiltrative tumor, none of which are evident in this case.
A Precocious puberty
A nonenhancing mass that is isointense to gray matter in this location in a patient of this age is suggestive of a hypothalamic (tuber cinereum) hamartoma. These hamartomas are composed of disorganized neural elements, can be sessile or pedunculated, and may be iso- to hyperintense on T2 images (as in this case), depending on the proportion of glial cells within them. These are benign lesions that do not grow and classically are associated with central precocious puberty and uncontrollable laughing spells (gelastic seizures). The main diagnostic consideration is a low-grade glioma. (B–D) Hypothalamic hamartomas do not enhance or grow, and calcifications are rare.
B CCM1
Approximately 20% of cavernomas are familial, and these are more commonly multiple. They can be associated with mutations in the CCM1 (usually in Hispanics), CCM2, or CCM3 genes. (A) Mutations in the ENG gene are associated with hereditary hemorrhagic telangiectasia type 1. (C) Mutations in the ACVRL1 gene are associated with hereditary hemorrhagic telangiectasia type 2. (D) Phenotypic manifestations of RASA1 gene mutations include capillary and arteriovenous malformations and arteriovenous fistulas.
B Rathke cleft cyst
Rathke cleft cysts are true cysts lined by epithelium that develop from remnants of Rathke’s pouch between the pars intermedia and pars distalis of the pituitary gland. Because the pars intermedia is difficult to visualize on imaging, it typically appears as a homogeneous mass separating the adenohypophysis from the neurohypophysis. It almost always is homogeneous, and its signal intensity varies depending on the presence of triglycerides, cholesterol, and protein (note intrinsic T1 hyperintensity on this noncontrast scan). It sometimes can occur in the suprasellar compartment and almost never is symptomatic. (A) Craniopharyngiomas are heterogeneous masses that usually arise at the level of the infundibulum. They show areas of enhancement, and the great majority of the adamantinomatous type (seen predominantly in children) have associated calcifications. (C) Lymphocytic hypophysitis is a nonneoplastic inflammatory condition that may affect any part of the pituitary gland and infundibulum. It does not present as a discrete mass, as seen in this case. (D) Granular cell tumors arise from granular cell nests in the neurohypophysis or infundibulum. They most commonly are suprasellar and almost never are purely intrasellar. Note the normal-appearing posterior pituitary bright spot along the posterior aspect of the cyst. (E) Neurosarcoidosis can involve the pituitary gland and infundibulum but would not result in a discrete, well-defined mass with intrinsic T1 hyperintensity, as in this case.
B Solid appearance
Craniopharyngiomas have a bimodal distribution with peaks at 5 to 14 years of age and 50 to 75 years of age. Adamantinomatous craniopharyngiomas tend to occur in children and more commonly are associated with cystic changes (filled with what is described as “motor oil” on gross exam) and calcifications. Adult craniopharyngiomas more commonly are of the papillary subtype and are more solid and devoid of cystic changes. (A) Cystic changes are more common in adamantinomatous craniopharyngiomas, which usually occur in children. (C) Calcifications are more common in adamantinomatous craniopharyngiomas. (D) Heterogeneous contrast enhancement can be present in both types of craniopharyngiomas but may be more commonly homogeneous in the papillary type due to their usually solid appearance. (E) Apparent diffusion coefficient (ADC) values do not discriminate between papillary and adamantinomatous craniopharyngiomas. They may, however, help distinguish solid papillary craniopharyngiomas from germinomas, which show restricted diffusion and therefore lower ADC values by virtue of their high cellularity.
D Semicircular canal
The arrow points to the posterior limb of the posterior semicircular canal. (A) The singular canal transmits nerve fibers from the vestibule to the posterior semicircular canal. It is very small and not shown on this image. (B) The tympanic segment of the facial nerve canal can be seen more anteriorly along the medial aspect of the epitym-panum. (C) The normal vestibular aqueduct is seen as a flat line posterior and medial to the posterior semicircular canal.
C Leading edge of high diffusion-weighted imaging signal
A leading edge of high diffusion-weighted imaging signal has been described in larger and new progressive multifocal leukoencephalopathy (PML) lesions and is thought to be related to cytotoxic edema. (A) Signal abnormalities in PML are usually bilateral but asymmetric. (B) There generally is no significant edema in PML, and when it is present, it should raise concern about immune reconstitution inflammatory syndrome (IRIS), particularly when accompanied by contrast enhancement. (D) There usually is no contrast enhancement in PML. (E) Involvement of the U fibers is a characteristic of subcortical PML, which results in a scalloped appearance.
A Low apparent diffusion coefficient values
The lesion’s location, imaging characteristics, and pathological description are most consistent with a pineoblastoma. These lesions are primitive neuroectodermal tumors that most commonly occur in children younger than 10 years of age. Like other highly cellular tumors with a similar histology, pineoblastomas commonly have profound restricted diffusion due to very low apparent diffusion coefficient values. (B) “Engulfed” calcifications characteristically are described in germinomas. Calcifications in pineoblastomas tend to be more peripheral (“exploded”). (C) Because of their high cellularity, pineoblastomas usually show high density on CT. They may be heterogeneous due to cystic changes and necrosis. (D) A dural tail is characteristically seen in meningiomas. It should enhance more avidly than the tumor and taper away from it.
A Pituitary apoplexy
Pre- and postcontrast MR images of the pituitary fossa accompany the question. The noncontrast image (left; note the lack of enhancement of the nasal mucosa) shows bright foci expanding the pituitary gland consistent with blood products. Pituitary apoplexy is an acute syndrome that can present with severe headaches, diplopia (due to mass effect on the oculomotor nerves), visual deficits (if the optic chiasm or optic nerves are compressed), and hypopituitarism. Sudden deficiency of adrenocorticotropin/cortisol may result in life-threatening hypotension. Hemorrhage usually occurs into a preexisting pituitary adenoma (such as in this case; note how the sella is mildly expanded) and rarely into a healthy gland. (B) Craniopharyngiomas typically are seen in children but have a bimodal age peak and also can present in young and middle-aged adults. They tend to develop around the infundibulum (rather than within the pituitary gland) and have a more insidious course compared with pituitary apoplexy. (C) Epidermoid tumors in this region usually are suprasellar. On T1-weighted sequences, they tend to have signal intensities close to that of cerebrospinal fluid and do not enhance. They may result in mass effect on adjacent structures, but their presentation would be more insidious than pituitary apoplexy. (D) Aneurysms can have unusual signal intensities due to thrombosis and also can present with acute headache if they rupture. The lesion in this case arises within the pituitary gland as can be seen by small claws of enhancing tissue around the hemorrhage.
D The lesion is entirely radiation sensitive and should be treated primarily by radiation.
The imaging and pathological characteristics of this mass in a young adult are most consistent with a germinoma. A normal pituitary gland is present on the sagittal images; therefore, this is not a pituitary adenoma. Germinomas usually demonstrate avid homogeneous enhancement as well as restricted diffusion on MRI apparent diffusion coefficient maps and hyperdensity on CT due to their high cellularity. Although pineal region germinomas are significantly more frequent in males (male-to-female ratio of 10:1), the gender distribution of suprasellar lesions is relatively even. Pure germinomas are exquisitely sensitive to radiation, with long-term progression-free survival rates greater than 90% for localized lesions; therefore, this constitutes the mainstay of therapy, and gross total resection is not usually recommended for pure germinomas. The role of surgery in such cases generally is limited to tissue biopsy and decompression in cases of acute visual symptoms (in suprasellar lesions) or obstructive hydrocephalus (in pineal lesions). Although most germinomas do respond to chemotherapy, chemotherapy alone is associated with high rates of relapse.
B Hemiparesis
The axial FLAIR image shows increased signal in the visualized portions of the right internal carotid artery within the carotid canal due to thrombosis, which may result in left hemiparesis if there is resultant anterior circulation ischemia. (A) Vision loss may be seen as a consequence of posterior circulation infarcts involving the visual cortex. (C) Gait ataxia may result from occlusion of the cerebellar arteries. (D) Lateral medullary syndrome (also known as Wallenberg syndrome) usually results from posterior inferior cerebellar artery territory infarcts. (E) Locked-in syndrome may be secondary to infarcts of the lower pons in the proximal basilar artery territory.
D High FiO2 concentration
High FiO2 concentrations have been shown to result in sulcal FLAIR nonsuppression and is a commonly encountered phenomenon in patients undergoing general anesthesia. Keeping FiO2 concentrations below 50% decreases the incidence of this finding. Causes of FLAIR nonsuppression include leptomeningeal disease (infectious or carcinomatous meningitis), subarachnoid hemorrhage, prior gadolinium administration in patients with renal insufficiency, and susceptibility artifacts commonly from metallic dental orthodontia and ventriculoperitoneal shunt reservoirs. (A) Leptomeningeal tumor spread would be highly unlikely in an asymptomatic and otherwise healthy child. (B, C) Meningitis and subarachnoid hemorrhage are unlikely, given the patient’s clinical background.
B Well-circumscribed margins
Hydatid cysts usually have well-circumscribed margins with a thin wall that is hypointense on T1 and T2 images. They are spherical and typically occur in the middle cerebral artery distribution. Their signal tends to follow that of cerebrospinal fluid. (A) Perilesional edema is absent in hydatid cysts unless there is superimposed infection or rupture. (C, D) Hydatid cysts do not show restricted diffusion or enhancement unless there is superimposed infection. (E) There is usually no calcification in hydatid cysts.
B Eosinophilic granuloma
Eosinophilic granuloma is the localized form of Langerhans cell histiocytosis characterized by infiltration with myeloid dendritic cells. In the spine, it most commonly affects the vertebral body and can result in a vertebra plana with variable degrees of epidural or paravertebral tissue. T2 signal tends to be normal or near normal. (A) Metastases from neuroblastoma usually are more heterogeneous and ill defined. They also may present with a soft tissue component projecting outside of the vertebra. (C) Telangiectatic osteosarcomas of the spine are rare. They are heterogeneous and frequently hemorrhagic with fluid-fluid levels. (D) Diskitis-osteomyelitis is an infectious process that, in children, probably begins in the disk (which still is vascularized). It would result in increased T2 signal within the disk and variable degrees of end-plate destruction (not present in this case). (E) A fracture would not have such a homogeneous appearance with smooth margins unless it is chronic. It also would not explain the solid-appearing tissue bulging into the prevertebral region.
C Inferior petrosal sinus
Shown in the image accompanying the question is the inferior petrosal sinus, which generally transmits blood from the cavernous sinus to the jugular vein or, less commonly, to the suboccipital venous plexus via the hypoglossal canal; however, there is marked anatomic variation. (A) The sphenoparietal sinus receives tributaries from the middle cerebral, middle meningeal, and anterior diploic veins, and drains into the cavernous sinus. It courses along the ridge of the lesser wing of the sphenoid bone. (B) The superior petrosal sinus runs along the superior aspect of the petrous bone and drains blood from the cavernous sinus into the transverse sinus. (D) The inferior anastomotic vein (of Labbé) drains the temporal convexity and opercular region transmitting blood from the middle cerebral vein to the transverse or sigmoid sinus. (E) The marginal sinus extends along the rim of the foramen magnum.
B They arise from anomalous differentiation of the meninx primitiva.
Intracranial lipomas are congenital lesions and not true neoplasms. They arise from anomalous differentiation of the meninx primitiva. (A) The tubulonodular variant and not the curvilinear type of intracranial lipoma is associated with callosal dysgenesis. (C) Short-tau inversion recovery (STIR) sequences nonselectively suppress fat and other tissues that have a short T1 values; therefore, a lipoma would demonstrate suppressed signal. (D) Calcification is common in pericallosal and interhemispheric lipomas, particularly in association with callosal dysgenesis. (E) Approximately 85% of intracranial lipomas arise at the midline. They are less commonly seen in the quadrigeminal plate, cerebellopontine angle, suprasellar, and sylvian cisterns.
D Grade 4
The coronal ultrasound image accompanying the question shows intraventricular hemorrhage involving the entire right lateral ventricle and left temporal horn. There is extensive parenchymal abnormality surrounding the right lateral ventricle due to venous ischemia. Findings are consistent with grade 4 intraventricular hemorrhage. Note ventricular dilatation. (A) Grade 1 intraventricular hemorrhage is confined to the germinal matrices, which are located in the caudothalamic grooves. (B) Grade 2 intraventricular hemorrhage is defined by intraventricular hemorrhage extension with normal-sized ventricles. (C) Grade 3 intraventricular hemorrhage is defined by intraventricular hemorrhage extension accompanied by ventricular distention. (E) There is no grade 5 intraventricular hemorrhage.
C Neuroglial cyst
The axial T2 image accompanying the question shows a well-circumscribed, cystic-appearing parenchymal lesion in the right cerebellum with an imperceptible wall. There is no contrast enhancement. Findings are most consistent with a neuroglial cyst. These are benign, epithelial-lined lesions of different sizes that can be found virtually anywhere in the neuraxis. There typically is no surrounding edema. (A) Arachnoid cysts are extra-axial. This is an intra-axial lesion, as it is nearly completely surrounded by parenchyma. (B) Even though they can occur in isolation, giant perivascular spaces usually have some structure to them and often show a clustered or branching pattern. It would be very unusual for one to present as a single, well-circumscribed cyst. Giant perivascular spaces can have areas of FLAIR hyperintensity due to gliosis around them. (D) Cysticercal cysts usually are smaller than the pictured cyst. A scolex, wall enhancement, calcification, or surrounding edema may be seen depending on the Escobar stage of the parasite. The racemose form can develop within the subarachnoid space or ventricles and appears like a cluster of cysts.
D Atrophy of the ipsilateral mammillary body
The image accompanying the question shows atrophy and loss of the internal architecture of the right hippocampus with increased signal. Additionally, there is atrophy of the ipsilateral mammillary body compared with the left, as can be seen in severe and long-standing cases of mesial temporal sclerosis. (A) MR spectroscopy may show decreased N-acetylaspartate and mildly increased myoinositol in mesial temporal sclerosis. (B) FDG-PET may by useful by showing decreased metabolism/uptake in the hippocampus in patients with mesial temporal sclerosis even in the absence of structural abnormalities on MRI. (C) Atrophy of the ipsilateral fornix can be seen in severe and longstanding cases of mesial temporal sclerosis.
A Requires a pial-arachnoid defect
The images accompanying the question show an intracerebral pneumatocele. The coronal CT reformat (left) shows a fracture through the right frontal sinus and air tracking intracranially with the formation of a parenchymal air cyst, which can be characterized best on the axial T2 image (right). There also is a cerebrospinal fluid level present within the cyst. An intracerebral pneumatocele requires a defect in the pia-arachnoid membrane in close proximity to a craniodural defect. Air may accumulate due a ball valve effect or possibly due to increased cerebrospinal fluid leakage, leading to slightly negative intracranial pressures. (B) About 75 to 90% of intracerebral pneumatoceles are secondary to trauma as in this case. Pneumatoceles are present in up to 25% of all cases of pneumocephalus. (C) Pneumatoceles are not true cysts, and therefore are not lined by epithelium. (D) Arachnoid cysts are lined by arachnoid cells formed by the splitting of arachnoid membranes.
C Enhancement of the paraspinal musculature
Enhancement of the paraspinal musculature is an indirect sign of avulsion injury due to denervation. Enhancement of intradural nerve roots indicates functional avulsion even in the presence of a normal-appearing nerve. (A) These lesions are fluid-filled pseudomeningoceles and would not show contrast enhancement unless they were infected. (B) Fatty lesions would show suppression of signal on STIR images. (D) Restricted diffusion may be seen in many disease processes. In the spinal cord, it can be secondary to infection or cord ischemia. The pseudomeningoceles in this case would not show restricted diffusion.
C Trigeminal nerve
Shown in the image accompanying the question is the trigeminal nerve, which arises from the lateral aspects of the pons. It has a characteristic shape, with fibers that appear to spread out before piercing the dura and entering the Meckel cave. (A) The oculomotor nerves are relatively thick and can be identified exiting the brainstem at the level of the pontomesencephalic junction. They course between the posterior cerebral and superior cere-bellar arteries on coronal images. (B) The trochlear nerve generally is not seen on CISS or FIESTA images due to its small caliber, unless thinner slices are acquired (0.4 mm). (D) The abducens nerves are thin and can be seen exiting the brainstem at the level of the pontomedullary junction. (E) The glossopharyngeal nerve is part of the cranial nerve IX–X–XI complex. It exits the upper medulla and leaves the skull through the pars nervosa of the jugular foramen.
C Carotid artery dissection
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree