Fig. 2.1
The White and Punjabi three-dimensional space coordinates system
When this happens, in a biomechanical approach [2, 3] the spine can be defined as “unstable” since there is a loss of motion segment stiffness with an abnormal response to the applied loads characterized kinematically by abnormal movement in the motion segment beyond normal constraints [3].
Obvious modifications happen in the unstable spine, from discopathy to facets degeneration and often, finally, degenerative spondylolisthesis, but the main difficulty in studying the unstable spine (often an aging spine) is the extreme variability of symptoms even in presence of the same modifications.
This consideration is important since spine instability is considered the principal cause of low back pain and the most important indication to spine surgery [4].
As the “degenerative cascade” [5] starts, for example, from an early disc degeneration, this motion conduction disorder promotes further degeneration of the whole structures involved (bones, ligaments, articular processes) that increase the initial anomaly. As the cascade proceeds, the system decreases its potential energy to a lower value, producing pain until it reaches a new equilibrium at a lower energy level.
This new relatively stable energetic level can be the starting point of a new “instability cycle” in a sort of cyclic self-perpetuating disorder that finally leads to hypomobility, stenosis, and functional damage [6] at the lowest energetic level; in other words, the theory of the “degenerative cascade” identifies three phases (dysfunction, instability, restabilization at a lower potential energy level) by which degenerative disease of the spine proceeds and with regard to the “catastrophe fold theory” [5], according to which further minimal changes in a “quite-stable/quite-unstable” system may be accompanied by major changes in function.
2.2 Diagnostic Workup
The X-ray–based imaging techniques used in the diagnosis of spine instability can be divided in two great groups: the static and the functional. In the first group are conventional plain films and computed tomography (CT).
In the second group are the dynamic plain films and axial loaded (AL)-CT systems.
Magnetic resonance imaging (MRI) and upright MRI will be discussed in a different chapter
Get Clinical Tree app for offline access

1.
Plain Film – The two-projection conventional plain film of the lumbar spine remains the basis in the study of the lumbar tract. Much information can be obtained from a simple couple of images. In a nonpathological spine (Fig. 2.2), usually in younger people, it is possible to assess if the vertebrae are well aligned, if the lumbar lordosis is correct, if the discs have sufficient thickness and shape, if the spinous processes are well distanced and aligned, and if the articular processes are in the correct position; in fact when the FSU is intact, the disc has normal height and the articular facets have a correct position: the inferior edge of the inferior facet of the superior element of the FSU must be higher than the inferior edge of the superior facet of the inferior element of the FSU (Fig. 2.2b, c).
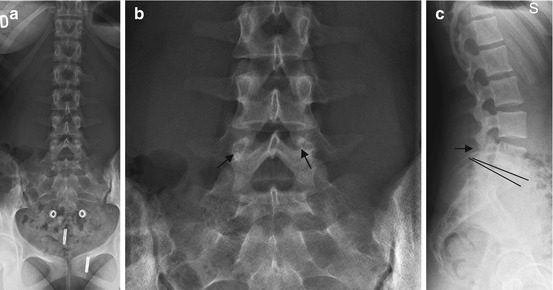
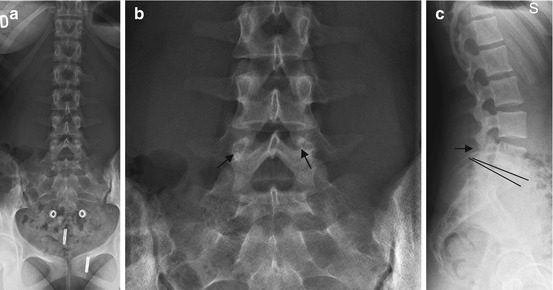
Fig. 2.2
Female, 20 years old. Nonpathological lumbar spine: conserved lordosis, regular disc-space height and regular disc shape (c). The interspinous processes are well aligned (a, b) and the interspinous space is conserved. The articular processes are in regular position (arrows – see text)
This sign can be easily seen on the AP projection of a common plain film. If it is true, the corresponding interspinous space is conserved, and this can be seen both on AP and lateral view of a conventional plain film. Obviously discs and roots cannot be directly seen on plain film, and this is the main limit of this diagnostic method.
On the lateral view not only the distance between discs but even the shape of the discal space can be observed: usually discs have a quite rectangular shape from L1 to L3; in L4–L5 and, above all, in L5–S1, the disc has a triangular shape, with the apex directed backward. A change in this shape, even with a conserved disc thickness, can be one of the first signs of some disc degeneration (Fig. 2.3) (see later).
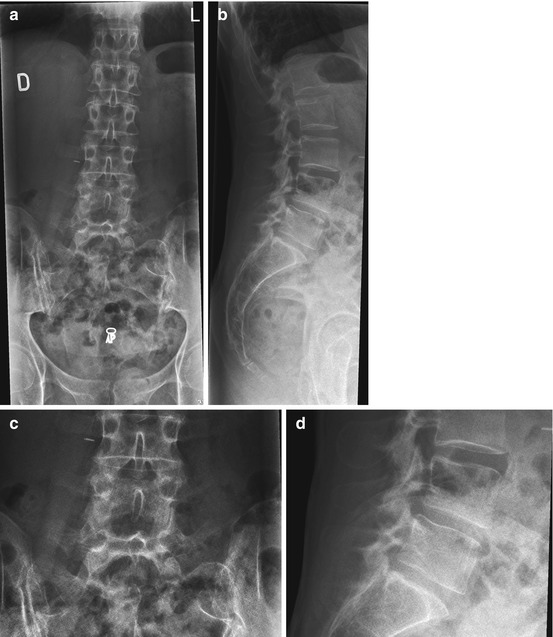
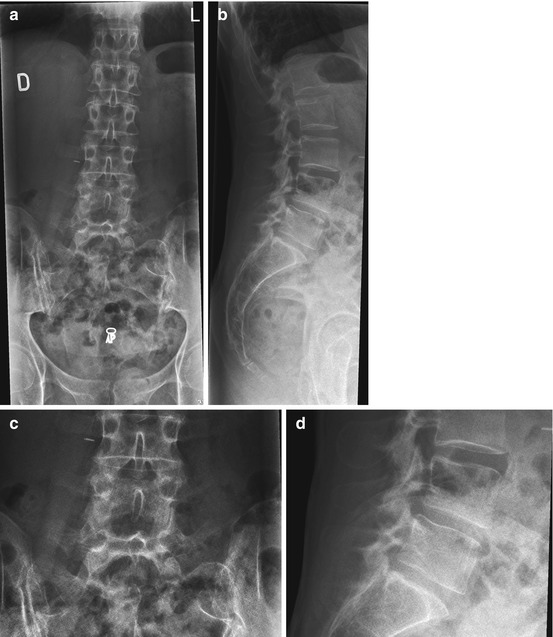
Fig. 2.3
Female, 51 years old, LBP. Reduction of lordosis but conserved disc height. Slight reduction in interspinous space L4–L5 (b, d). In L4–L5 and L5–S1 the disc shape is quite rectangular (a, c). Minimal anterior listhesis of L4 on L5 (b, d). Schmorl nodes are present on the end plates of many vertebrae (b)
When disc degeneration proceeds, early signs can be the presence of Schmorl nodes on the vertebral end plates and, later, the comparison of traction spurs, located 2–3 mm from the vertebral end plate.
Another early sign is the underslipping of the inferior facets, with narrowing of the interspinous space (Fig. 2.4).
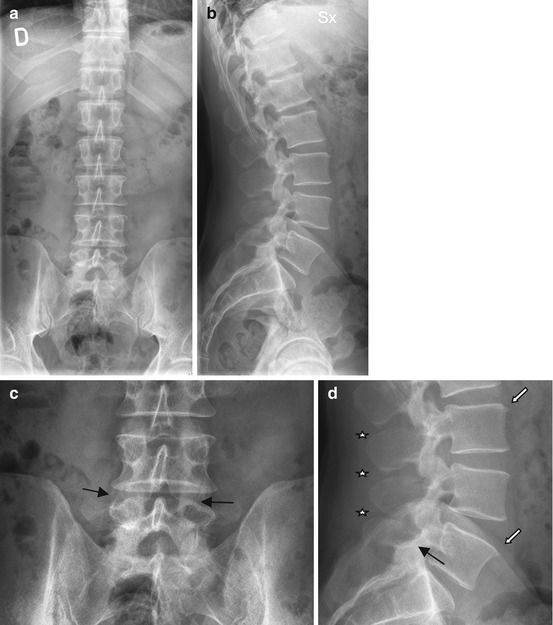
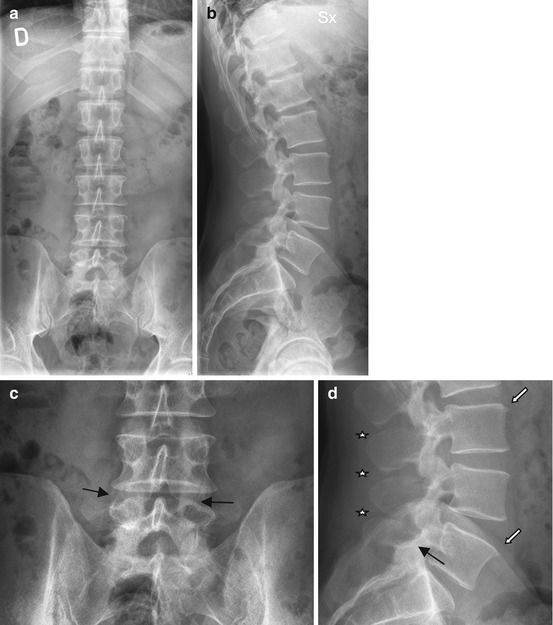
Fig. 2.4
Male, 35 years old, LBP. AnteroPosterior (a) and Lateral (b) X-ray view, and L4-S1 unit magnification (c, d). Reduction of the interspinous spaces between L3 and S1 (stars in d), low position of inferior articular processes of L4 (black arrows in c and d), traction spurs on many vertebrae (white arrows in d)
This sign means that the disc begins to transfer part of the axial load to the posterior arch [7].
They can be seen on AP and lateral view. As the degeneration proceeds, the discs loose thickness, and often, in decubitus views, a vacuum phenomenon can be seen [4].
On AP view deformation of the spine (scoliosis, rotation on “Z” axis, osteophytes) can be appreciated, especially in follow-up radiograms (Fig. 2.5). The articular facets are further underslipped, and the spinous processes are in contact and misaligned and deformed and often show sclerosis in the contact points (the so-called Baastrup’s disease), which often appears degenerative listhesis of L4 on L5.


Fig. 2.5
Female, 30 years old at a–a′; LBP. Good conservation of lordosis. Reduction of L5–S1 disc height, with rectangular shape of disc space. Underslipping of L4 inferior facets and reduction of interspinous space. Three years later (b–b′) comparison of left scoliosis, further facets underslipping and reduction of interspinous spaces; loss of disc height in L4–L5 and L5–S1. Two years later comparison of L4–L5 degenerative listhesis. Further left scoliosis. Deformation of vertebrae and misalignment of the spinous processes (c–c′)
At the late stage of the disease the most frequent abnormalities detected are stenosis due to extensive spondylosis, loss of disc height, facets joints degeneration, and degenerative listhesis (usually of L4 on L5). The stenosis can be central and/or lateral but usually is mixed (Fig. 2.6).


Fig. 2.6
Female, 72 years old. LBP and neurogenic claudication – end-stage spine instability
2.
Functional Plain Film – Functional radiography in the sagittal plane can be achieved either in flexion and extension or in the AP projection in left and right lateral bending. Because of its simplicity, low expense, and wide availability, functional flexion-extension radiography is the most studied and the most widely used method in the imaging diagnosis of lumbar intervertebral instability and this despite the approximation of the method, due to the geometrical distortion of the radiological projection and to the fact that any patient has its own capacity to perform such maneuvers. It is still debated what patient position (lateral decubitus versus standing) is the best way to execute the examination, the difference probably being the muscular compensation and resistance to the pain and to the spine insufficiency. On the other hand with this examination, the edge between normal and abnormal movement is also difficult to determine. In any case in functional plain films, many signs can be detected: the loss of disc height, the loss/reduction/comparison of disc vacuum phenomenon, the misalignment of vertebrae, their rotation on any of the three space planes, increasing lateral bending, and/or listhesis (Fig. 2.7)
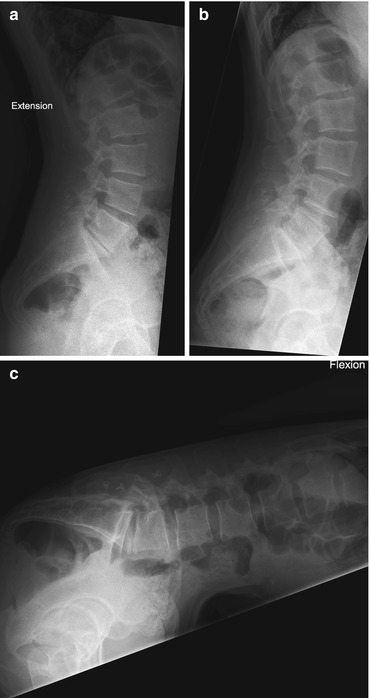
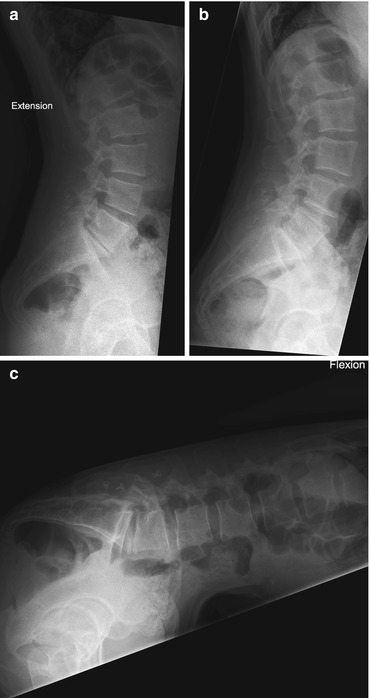
Fig. 2.7
Female, 33 years old. LBP after L4–L5, L5–S1 DIAM positioning. Functional X-ray. On neutral upright position (b) L5–S1 discopathy. In extension (a) poor mobility due to pain; comparison of little vacuum phenomenon in L5–S1. In flexion (c) note the change of shape of L4–L5 disc due to sagittal rotation of the vertebrae
3.
Myelography – In this examination an opaque iodinated contrast media is injected in the dural sac with a lumbar puncture. In this way the content of the dural sac and the compression that can be determined by discs, ligaments, or tumors can be easily evaluated. This examination is usually completed by functional plain films. Until the emergence of CT and MRI, it was the only way to study the spine contents. Actually the use of this method is limited because of its invasivity; nevertheless, in some situations, it can be used when MRI cannot be performed (i.e., claustrophoby, pacemaker, or other electronic devices) or in instrumented spines, where artifacts hinder a correct diagnosis (Fig. 2.8). Myelography is always completed with functional X-ray (Fig. 2.9) and with myelo-CT; if possible, it can be completed with AL/myelo-CT.
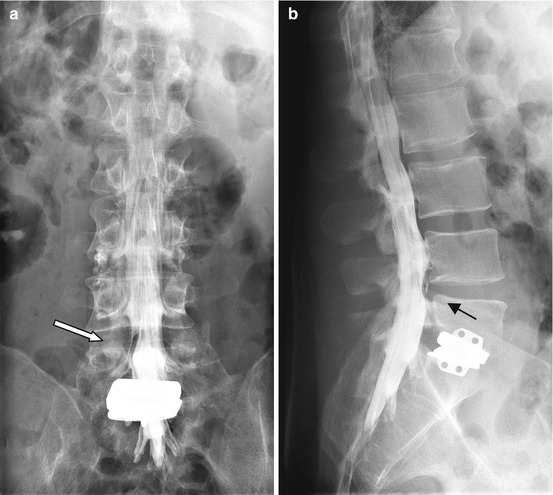
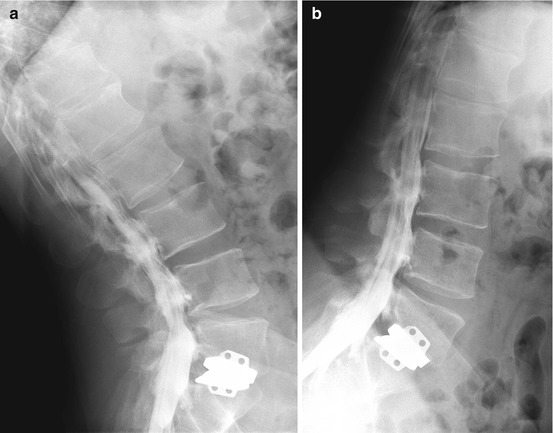
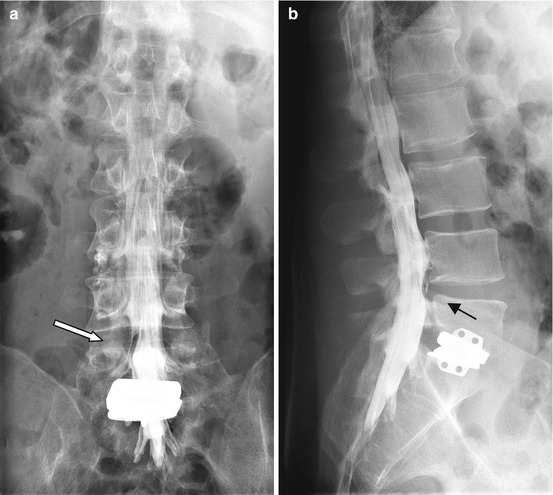
Fig. 2.8
Male, 34 years old. LBP after L5–S1 disc prosthesis. Myelography – mild disc compression on sac in L4–L5 (black arrow in b) with compression on right L5 root (white arrow in a)
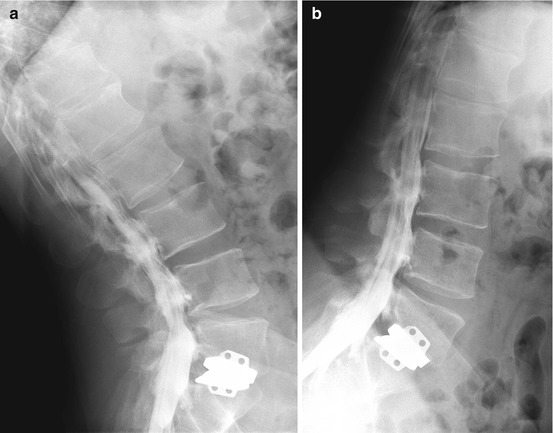
Fig. 2.9
Same patient in Fig. 2.8. Functional projections: extension (a), flexion (b). Mild dural sac compression in L2–L3, L3–L4, and L4–L5 during the functional maneuvers
4.
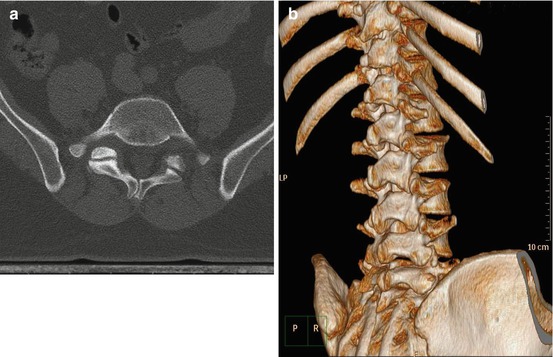
CT – Since this diagnostic tool appeared in late 1970s and early 1980s, it had a deep impact on the spine diagnostic workup: for the first time, all the structures of the lumbar spine could be directly seen; the disc, the ligaments, the nerve roots, and the dural sac could be seen without the use of contrast media. The view on the axial plane gave another perspective to the understanding of the modifications that happen in the unstable spine. Lately the spiral technology added the multiplanar view and the three-dimensional (3D) perspective to the study of the spine. For example, CT can demonstrate underlying predisposing anatomic factors, such as facet joint asymmetry, or asymmetry of the posterior arch (Fig. 2.10), that may lead to an abnormal distribution of the vectorial forces, leading to axial rotation of a vertebra on the subjacent one. This can lead to the comparison of abnormal centers of rotation that accelerate the degenerative cascade on the lumbar spine. CT is the procedure of choice to detect a vacuum phenomenon within the degenerating discs or facet joints, findings that express a deep degenerative process on these structures and suggest their hypermobility (Fig. 2.11). A further advantage of CT is the actual possibility to produce high-definition 3D images; especially in late instabilities, 3D images clearly demonstrate the stenosis and the degenerative changes. CT finally is always the completion of myelography (see later).