Fig. 3.1
A 50-year-old man. (a) Sagittal T2-weighted image of lumbar spine, (b) MR myelography, (c) axial T1-weighted image and (d) axial T2-weighted image of intervertebral disk and facet joints
For practical purposes, a short standard protocol, including sagittal T1- and T2-weighted sequences and axial GRE or T2, is desirable for screening of a large number of patients with referred low-back pain. Improving the speed of these acquisitions with parallel imaging is helpful not only to improve patient throughput but also to minimize discomfort for patients who suffer back pain and may have difficulty lying in a fixed position for long periods of time. Axial GRE is used typically to assess degenerative disease in the cervical spine. Unlike with SE and FSE sequences, disk material (hyperintense on GRE) and osteophytes (hypointense) usually can be differentiated with GRE, regardless of flip angle.
Balanced steady state free procession (bSSFP) sequences also have an inherently high contrast between tissue and fluid. Moreover, compared with unbalanced steady state free procession (SSFP) sequences, bSSFP provides high baseline SNR. Thus, it provides an efficient alternative sequence for better detection of herniations, sequestrations, or nerve root compression. Conversely, the gray matter/white matter contrast of conventional bSSFP is relatively poor [11].
SE and FSE sequences provide good anatomic detail in spine imaging and are favored for the evaluation of spinal canal diameter and for the detection of spinal cord abnormalities, with less susceptibility artifact from the bone and improved contrast between gray and white matter structures within the cord, compared with GRE. Given the abundance of epidural fat within the lumbar spine and the relatively large disk spaces, FSE sequences are favored over GRE in the lumbar spine to assess for focal disk protrusion and nerve root compression. However, the CSF adjacent to the cord, together with cord motion, often causes ghosting artifacts in conventional Cartesian imaging and is particularly problematic in FSE T2-weighted images [26–30].
Additional sequences may be helpful in the case of persistent unexplained symptoms or for more complex or specific questions about anatomy or the influence of patient position on alignment and stenoses. Contrast-enhanced T1-weighted images with fat saturation can reveal facet joint pathology, spondylolysis, spinal degenerative/inflammatory changes, and changes within the paraspinal muscles, which are not always evident on conventional imaging.
Degenerative diskogenic vertebral changes can be noted on endplates bordering the intervertebral disks (Modic types 1–3). There are degenerative changes such as intervertebral osteochondrosis that are considered pathologic and not due to normal aging, including desiccation and narrowing of the disk, extensive gas in the disk, disk bulging, radial annular tears, posterior osteophytes, endplate sclerosis and erosions, and chronic bone marrow changes adjacent to the disk interspaces. Radial annular tears are failures of multiple annular layers. They are bright on T2-weighted images and may enhance. Modic type 1 corresponds to increased vascularity in the juxta-endplate vertebra. Its MRI appearance reflects increased water content: dark on T1-weighted images and bright on T2-weighted images. Modic type 2 represents increased fatty marrow: bright on T1-weighted and dark on fat-suppressed T2-weighted FSE images. Modic type 3 denotes sclerotic changes: dark on both T1- and T2-weighted images. Posterior osteophytes are also dark on both T1- and T2-weighted images and can narrow the spinal canal and neural foramina. Extensive gas in the disk (vacuum disk) can be seen on plain films and CT and sometimes seen on MRI [17].
The association of vertebral instability with changes in the bone marrow adjacent to the endplates has been discussed, but without consistent results. Modic et al. stated that the clinical importance of these changes in the bone marrow is unknown. Lang et al. observed bone marrow changes adjacent to the endplates in postoperative instability, but no statistically significant correlation exists between segmental instability and abnormalities of the bone marrow adjacent to the endplates in patients without spinal fusion, as resulted from a study of Bram et al [14]. Conversely, Bram et al. found a significant association between radiographic instability and traction spurs and between radiographic instability and annular tears. In their study of patients with chronic low-back pain, Aprill and Bogduk first described annular tears as a high-signal intensity dot on sagittal T2-weighted images [1, 2, 17].
Therefore, flexion-extension radiographs should be considered in patients with annular tears or traction spurs. Unfortunately, additional studies supporting this conclusion are necessary before it can be generally accepted. A high-signal-intensity zone in the posterior annulus fibrosus on sagittal T2-weighted images has been found much too frequently in asymptomatic subjects to be considered a reliable independent diagnostic indicator.
A common source of chronic back pain is spondylolysis; it is defined as a fracture through the pars interarticularis. Diagnosis on MRI is difficult: sagittal T1-weighted images can be seen as a break in the bony cortex or the marrow signal of the pars interarticularis; however, 25 % of spondylolysis are missed on MRI [35].
Spondylolisthesis is anterior or posterior displacement (translation) of a vertebra relative to an adjacent vertebra. Anterolisthesis refers to anterior displacement of a vertebra relative to the adjacent caudal (inferior) vertebra, while retrolisthesis refers to posterior displacement. Severity is graded by the percentage of the vertebral body that is displaced (grades I–IV). Spondylolisthesis frequently causes neural foraminal narrowing best evaluated on sagittal T1-weighted MR images [34]. The normal shape of the neural foramen is altered; the longest axis of the foramen changes from vertical to horizontal. The sagittal MRI can demonstrate foraminal stenosis, obliteration of foraminal fat, and nerve root compression and/or kinking. A fibrocartilaginous mass may be seen around the nonhealed pars fracture. A disk herniation is more common at the level above the spondylolisthesis than at the same level. The anterior displacement of the upper vertebra relative to the disk confers the artifactual appearance of a disk bulge or herniation (pseudo-bulge or herniation) [35, 36].
Degenerative spondylolisthesis appears to be associated with instability or hypermobility when studied with kinematic MRI (Figs. 3.2 and 3.3).
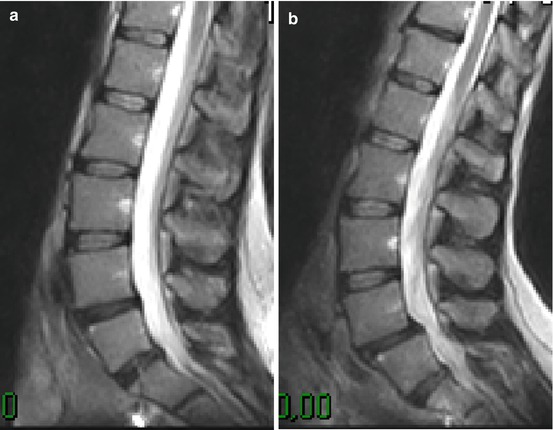

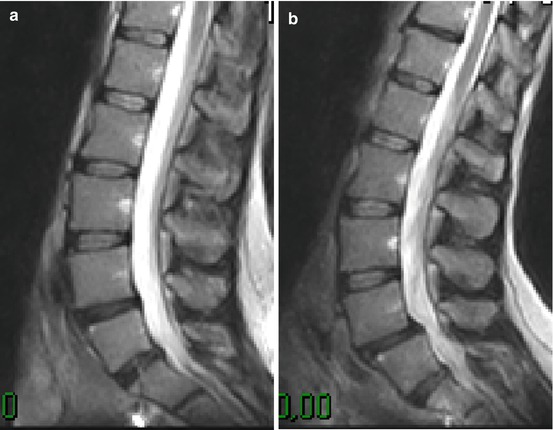
Fig. 3.2
A 55-year-old man with low-back pain. (a) Sagittal T2-weighted image of lumbar spine shows dehydration of the nucleus pulposus of L5/S1. (b) In upright position there is a spondylolisthesis in the L5/S1 (microinstability)

Fig. 3.3
A 75-year-old woman with neurogenic claudication. (a) MR examination in recumbent position shows mild listhesis of L5 and diffuse degenerative phenomena. (b) In upright examination the shifting of the vertebral body and stenosis of neural foramina that determine compression of nerve roots bilaterally are evident (c, d)
Degenerative disk disease and facet joint osteoarthritis affect the stability of the motion segment. However, the exact relationship between degenerative disk disease, facet joint osteoarthritis, and vertebral instability at MR imaging has not been defined. Murata et al. compared disk degeneration at MR imaging with that of flexion-extension radiography and found no statistically significant relation between segmental instability and disk degeneration. Fujiwara et al. also compared MR imaging and functional radiography of the lumbar spine to examine the relations among segmental instability, disk degeneration, and facet joint osteoarthritis in patients with low-back pain; they reported that an anterior translation of 3 mm or greater was positively associated with disk degeneration and facet joint osteoarthritis [6, 7, 9].
Recently, Splendiani et al. reported a study that suggests that the pathogenesis of radicular pain in some patients is the result of a dynamic stenosis of the foramen caused by the physiological load. In fact they demonstrate that the association between disk pathology and facet osteoarthrosis can determine foramina occult stenosis. Imaging with the patient in a supine position may not correctly represent the degree and the clinical relevance of a foraminal stenosis (Fig. 3.3) [29].
Although the lumbar spine undergoes large compression loads in normal activities, MR imaging is routinely performed with the patients supine and, therefore, with the spine unloaded. Advances in MR techniques have made possible the development of open MRI systems, which provide the opportunity to investigate spinal kinematics and vertebral instability. Early studies were limited to assessing spinal kinematics by imaging the patient in the supine position in combination with several different axial-loading MRI-compatible devices and not truly reflect postural spinal changes related to muscle tone, loads on the lumbar spine that increase in a caudal direction rather than being uniform at each spinal level, and the effects of core muscle activation on the spine [10].
Improvements in available open MRI systems from increased field strength, field homogeneity, gradient generation, coil technology (quadrature coils), and faster image acquisition (dynamic equilibrium and magnetization transfer) have resulted in better signal-to-noise ratios, contrast and spatial resolution, and therefore, image quality. Open MRI systems with a vertical gap allow imaging under the influence of gravity in the upright position (seated or standing), with varying kinetic maneuvers (flexion, extension, lateral bending, rotation, etc.), as well as with the patient supine. Imaging in the physiologically representative upright position and with kinetic maneuvers allows accurate assessment and measurement of changes in the relationship between the components of the functional spinal unit and the potential to correlate radiological signs with positional symptoms [31].
Weishaupt et al. evaluated whether positional (seated) MR imaging can demonstrate nerve root compromise not visible at conventional (supine) MR imaging in 30 patients with chronic low-back pain unresponsive to nonsurgical treatment but without compression of neural structures. Positional pain differences were related to position-dependent changes in foraminal size. Positional MR imaging more frequently demonstrated minor neural compromise than did conventional MR imaging, but no convincing signs of canal or foraminal encroachments were found [32].
Wildermuth et al. investigated the influence of various body positions on the dural sac and the intervertebral foramina in 30 consecutive patients with combined low-back pain and sciatica, who were examined in the supine, upright flexion, and upright extension positions with an open MR imager. The authors found only small position-dependent differences in the sagittal diameter of the dural sac and foraminal size, and the information gained in addition to that from standard MR imaging was limited. Moreover, the overall examination time created severe pain problems. Motion artifacts and difficulties in reproducing the positioning between the sequences occurred regularly. This impaired the possibilities for analyzing the content of the spinal canal [33].
On supine imaging, spinal alignment does not reflect the true postural effect of body weight, which can increase by 80 %, and the action of paraspinal and abdominal musculature. Normally the upper lumbar spine undergoes increased extension in the upright sitting and kneeling positions, the degree of extension decreasing in a caudal direction. The lumbosacral junction, representing the angle between the posterior margins of the L5 and S1 vertebral bodies, becomes less flexed and also more vertical to support the increased load in the upright position. This flexed position becomes more prominent in the seated compared with the standing position. On movement from flexion to extension, there is normally an increase in lumbar lordosis of 1.1–2.9° per vertebral level. From a neutral upright seated to flexed position, paradoxical extension at L5/S1 or L4/L5 and L5/S1 can be observed in normal subjects, whereas a change in anterior-posterior translation of between 1 and 1.5 mm may also be evident [14].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








