
Radiosurgical Treatment of Arteriovenous Malformations
Objectives: Upon completion of this chapter, the reader should recognize the indications for selecting radiosurgery over other treatment options and the results expected from this therapy.
Accreditation: The AANS* is accredited by the Accreditation Council for Continuing Medical Education (ACCME) to sponsor continuing medical education for physicians.
Credit: The AANS designates this educational activity for a maximum of 15 credits in Category 1 credit toward the AMA Physician’s Recognition Award. Each physician should claim only those hours of credit that he/she spent in the educational activity.
The Home Study Examination is online on the AANS Web site at: http://www.aans.org/education/books/controversy.asp
* The acronym AANS refers to both the American Association of Neurological Surgeons and the American Association of Neurosurgeons.
Patients and doctors have to choose between different management options for arteriovenous malformations (AVM); hence, controversy is common. Interpretation of the available literature (the science), together with physician judgment (the art), allows doctors to make clinical decisions with patients. The choices may be controversial in some instances and agreed upon by all in others. In this chapter, we discuss controversies associated with AVM radiosurgery, particularly in relation to patient selection and technique.
Successful AVM radiosurgery is dependent upon achievement of the outcome of complete AVM nidus obliteration that leads to elimination of the future hemorrhage risk.1–3 In achieving this goal, there should be no morbidity or mortality from hemorrhage or radiation-induced brain injury. When these outcomes can be achieved with a high likelihood, a strong case can be made for radiosurgery. If clinical or angiographic factors argue against the achievement of these goals, then other strategies should be considered. Physicians who make an argument for radiosurgery cite one or more of the following: (1) that radiosurgery is an effective therapy required for the management of deep-brain AVMs; (2) that radiosurgery is an effective therapy for residual AVMs after subtotal resection; (3) that radiosurgery is worthwhile in an attempt to lower management risks for AVMs in functional brain locations; (4) because embolization does not cure most AVMs, additional therapy such as radiosurgery may be required; (5) microsurgical resection may not be the best choice for some patients depending on their general health; and (6) reduced cost. Radiosurgery is the first and only biologic AVM therapy; it represents the beginning of future cellular approaches to vascular malformation diseases. For this reason, the future of radiosurgery may be impacted positively by the development of other biologic strategies such as brain protection or endothelial sensitization.
 Decision Making
Decision Making
Those who make an argument against the use of radiosurgery argue the following points: (1) that radiosurgery does not always work especially when only partial AVM obliteration is achieved4; (2) that brain hemorrhage may occur during the time it takes for radiosurgery to work; (3) that radiation-related morbidity may cause functional neurological deficits; (4) that there may exist “longterm” problems after brain irradiation5; and (5) that resection may be a more cost-effective treatment over the long term.6 Though all these points can be argued, most neurosurgeons agree that the role of radiosurgery is greatest for patients with small-volume, deep-brain AVMs.2,7–9 It has a lesser role for patients with larger and surgically accessible AVMs. In between these two extremes, there exists much debate. The role of radiosurgery for patients with small yet accessible AVMs is growing steadily.10 For patients with large-volume yet deeply located AVMs, multimodality management often is required. Thus, whether radiosurgery should be considered in the management of an individual patient depends upon the factors of AVM volume, brain location, prior hemorrhage history, patient age, and surgical resectability. These factors have been studied in detail by different groups toward predicting successful AVM outcomes or reasons for radiosurgery failure.3,11–14 The factors of AVM obliteration and radiosurgical morbidity on decision making are addressed in further detail later in this chapter.
 Case Illustrations
Case Illustrations
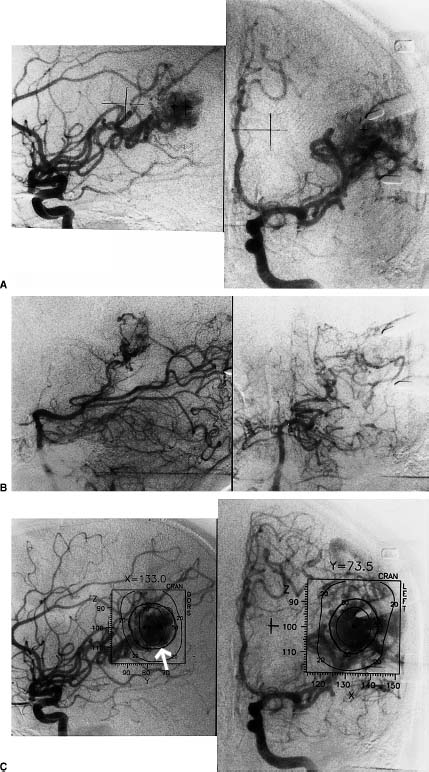
Case 1
A 20-year-old woman sustained a brain hemorrhage caused by an arteriovenous malformation in the region of the angular gyrus (Fig. 14-1A–D, 1F, 1G). The arguments for the use of radiosurgery are the location of the AVM within a critical brain area and that its overall size made it suitable for radiosurgery. However, because she had sustained a hemorrhage that caused neurological deficits, resection was considered because any potential deficits were already present. An argument against radiosurgery is the chance for hemorrhage during the latency to obliteration. The expected obliteration rate for an AVM of this size would be ~80% after a single procedure. Four years after radiosurgery, a small persistent nidus was identified on the vertebral angiogram (Fig. 14-1E). A second radiosurgery was performed that was followed by complete AVM obliteration.
Case 2
A 45-year-old man presented with headaches. They were caused by a temporal lobe arteriovenous malformation supplied by the middle cerebral artery. An aneurysm just proximal to the arteriovenous malformation was also identified (Fig. 14-2A,B). An argument for the use of radiosurgery is the small AVM volume, thus allowing radiosurgery as an alternative to resection or embolization. Arguments against the role of radiosurgery include the resectability of the AVM in this location (with relatively low risk) and the sustained hemorrhage risk during the radiosurgery latency interval. Management of the proximal aneurysm via intraoperative clipping is a strong argument for resection. This patient underwent radiosurgery; his 2-year angiogram showed complete AVM obliteration and elimination of the aneurysm.
Case 3
A 22-year-old woman suffered an intracerebral hemorrhage from an AVM located in the posterior limb of the left internal capsule. The hemorrhage caused hemiparesis, which had improved to a level of only mild arm weakness (Fig. 14-3A,B). She underwent radiosurgery because of the critical brain location of the malformation, its small and suitable size for radiosurgery, and the belief that this approach represented the lowest overall management risk. An argument could be made against radiosurgery because the patient had already sustained one hemorrhage and remained at a higher risk for a second bleed. However, the potential morbidity of resection appeared to outweigh this risk. Two years after radiosurgery, complete obliteration of the malformation was documented.
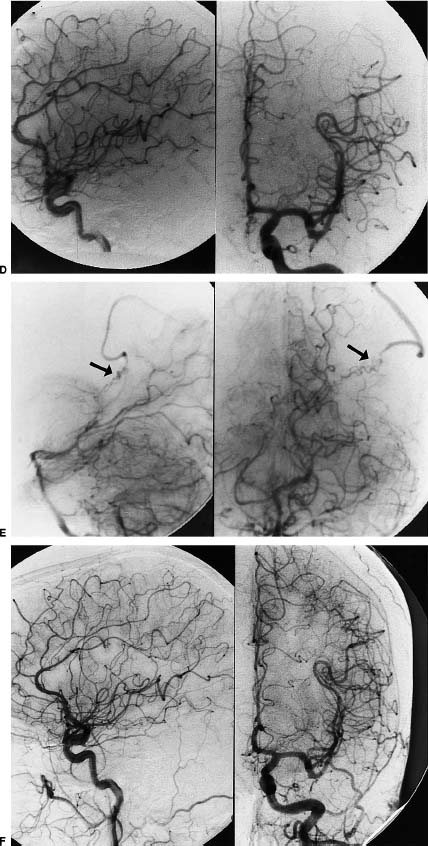
Case 4
A 40-year-old woman sustained an intraventricular and subarachnoid hemorrhage from a left parietal arteriovenous malformation. Symptoms from her intraventricular hemorrhage resolved. The case for radiosurgery included the critical brain location of the malformation and its suitable size. The argument against radiosurgery was that there remained a continued risk of rebleeding prior to nidus obliteration, and that the nidus was superficial in location and suitable for resection. However, the good functional status of the patient and the critical brain location were stronger arguments for radiosurgery (Fig. 14-4A–E). Three years following radiosurgery complete obliteration of the malformation was confirmed. She remains active with no new neurological deficits.
 Why Does Radiosurgery Work?
Why Does Radiosurgery Work?
Radiosurgery is effective because single-fraction irradiation causes significant injury to the endothelial cells of blood vessels that compose the AVM.8,15–17 Stereotactic definition of the AVM target ensures that these radiobiological effects are limited to the malformation. Conformal radiosurgery allows irradiation of only a small volume of surrounding normal tissue in the region of radiation dose fall-off.2,18 Dose-prescription formulae are used to help select an appropriate radiation dose depending on imaging and clinical factors.19,20
The immediate effect of radiosurgery is to damage the endothelial cells of the AVM vessels. The release of tissue-specific cytokines common to other forms of radiation-induced injury is likely to mediate such acute effects. Inflammatory cells mediate tissue repair in response to irradiation. Later, chronic inflammation consists of the ingrowth of granulation tissue that contains fibroblasts and new capillaries. These events may explain the delayed imaging changes sometimes observed after radiosurgery (as in Case 4 above). Szeifert et al identified the presence of actin-producing fibroblasts, so-called myofibroblasts, that are hypothesized to exert contractile properties and facilitate AVM obliteration.21 It is common that contrast-enhanced magnetic resonance imaging (MRI) studies at this late stage after obliteration show enhancement of the obliterated AVM. This finding does not indicate a “patent” AVM, but, we believe, a marker for the newly formed capillary network within the scarred AVM tissue remnant. Several reports have noted the rare, late finding of cyst formation at the AVM site, which probably represents expansion of the extracellular fluid space within the fibrosis.5,22 Radiosurgery may affect seizure control through irradiation of epileptogenic tissue or through correction of abnormal hemodynamic conditions.23–25
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


