Fig. 7.1
Cerebral vasculitis in a 50-year-old female with a history of TIA. MRI FLAIR sequence (a arrows): focal white matter hyperintensities. Left thalamic hypointensity on T2* sequence (b hollow arrow) related to old haematoma. Intracranial TOF MR angiography (c, d and e): multiple irregularities and arterial stenoses mainly involving terminal internal carotid arteries (c, d and e arrows)
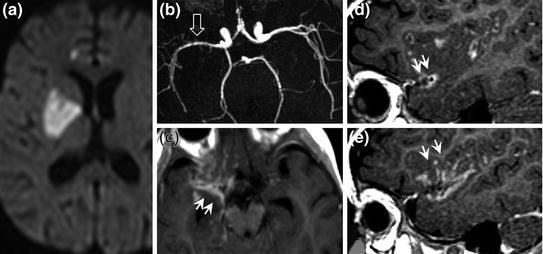
Fig. 7.2
Tuberculous cerebral vasculitis in a child with right deep middle cerebral artery infarction (a diffusion sequence). Stenoses and irregularities of right middle cerebral artery on the TOF sequence (b hollow arrow) with perivascular and meningeal contrast enhancement (c, d and e double arrows) related to infection
Systemic: Takayasu arteritis, polyarteritis nodosa (PAN), giant cell arteritis, Wegener’s granulomatosis, connective tissue diseases (systemic lupus erythematosus (Fig. 7.3), scleroderma), Behçet’s disease, Sjögren’s syndrome, rheumatoid arthritis.
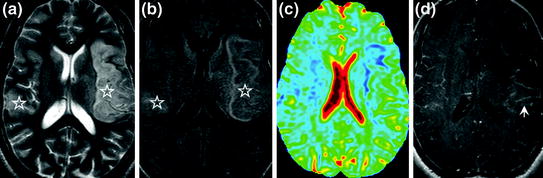
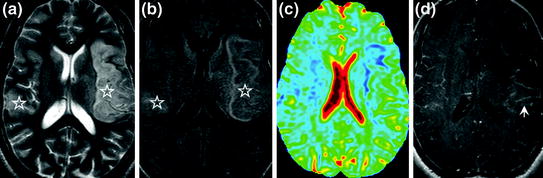
Fig. 7.3
Systemic lupus erythematosus in a 26-year-old patient. Recent bilateral middle cerebral artery cerebral infarction (a [T2] and b [FLAIR]: stars). Decreased ADC in ischaemic territories (c decreased ADC is shown in blue). Diffuse pial contrast enhancement after gadolinium injection (d arrow)
Toxins: opioids, heroin, cocaine, crack.
Isolated primary vasculitis of CNS (Fig. 7.4): isolated CNS vasculitis is rare, characterized by a nonspecific lymphocytic or necrotic granulomatous inflammatory infiltrate (also called cerebral granulomatous angiitis). It is diagnosed after exclusion of other causes of cerebral vasculitis.
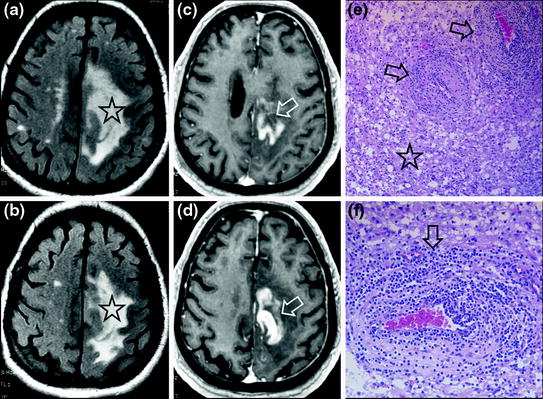
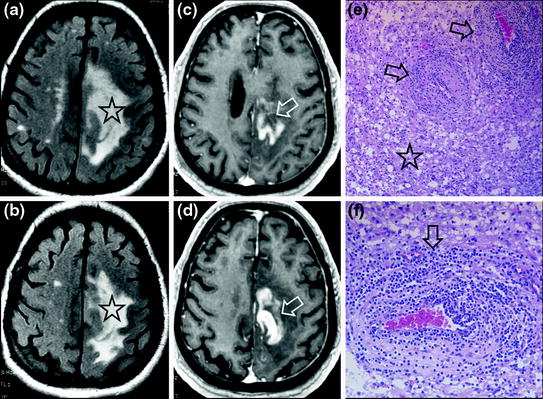
Fig. 7.4
Recent progressive right hemiplegia in a 74-year-old female patient. MRI shows oedematous lesions on FLAIR sequence (a and b stars) with cortical contrast enhancement (c and d hollow arrows). Histological diagnosis of primary central nervous system vasculitis: thickening of arterial walls (e and f arrows) and intravascular and perivascular T lymphocyte infiltrate with necrosis of adjacent cerebral parenchyma (e star). By courtesy of Dr. M. Levasseur, hôpital d’Orsay
Note: In SLE, the cerebral ischaemic lesion is more often caused by emboligenic lupus cardiomyopathy than by cerebral vasculitis.
Aetiological Work-Up
Laboratory tests:
routine: CBC, platelets, serum protein electrophoresis, CRP;
immunological: ANA, anti-DNA, ANCA, circulating anticoagulant, antiphospholipid antibodies, rheumatoid factor, cryoglobulin, complement, angiotensin-converting enzyme;
serology: herpes virus, varicella-zoster, hepatitis viruses, HIV, Lyme disease;
lumbar puncture.
Funduscopy or even fluorescein angiography.
ENT examination: look for evidence of Wegener’s granulomatosis.
Brain biopsy: only biopsy can provide the definitive diagnosis in primary CNS vasculitis and should be performed whenever aggressive treatment is considered.
Imaging
CT
Multiple intraparenchymal hypodensities corresponding to ischaemic sequelae. Intraparenchymal or cortical sulcus hyperdensity in the presence of cerebral or meningeal haemorrhage.
MRI
Multiple stenoses of intracranial and extracranial arteries on TOF sequences and cerebral MR angiography. Multiple focal, mostly subcortical hyperintensities on T2 and FLAIR images corresponding to ischaemic sequelae. Isolated or multiple focal hyperintensities on diffusion-weighted images with decreased ADC related to recent ischaemia. Possible contrast enhancement and thickening of vessel walls related to mural inflammation, especially visible on thin sections (2 or 3 mm) and with fat saturation (Fig. 7.5). Leptomeningeal contrast enhancement (more clearly visible on T1 SE sequences and less clearly visible on gradient-echo sequences such as 3D MPR sequences) and hyperintensity of cortical sulci on FLAIR sequences related to inflammation of leptomeningeal vessels. Signs of focal pachymeningitis may sometimes be observed.
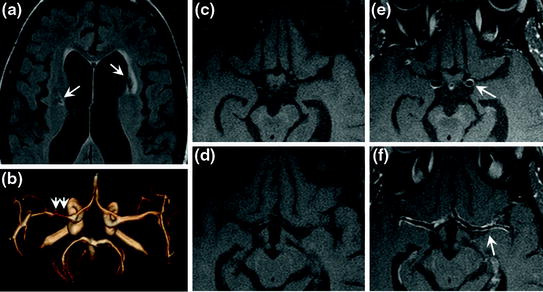
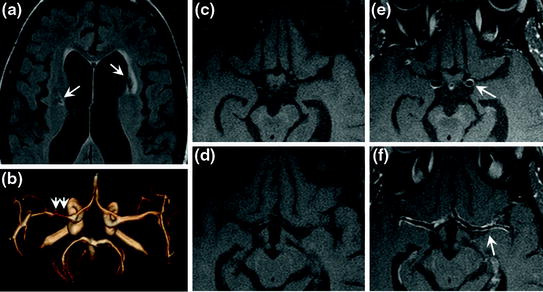
Fig. 7.5
Cerebral vasculitis in a 56-year-old female patient. MRI FLAIR sequence (a arrow) visualizes focal hyperintensities corresponding to old deep infarcts. On TOF sequence (b posterosuperior view, double arrows), severe stenosis of M1 segment of right middle cerebral artery. Diffuse contrast enhancement of arterial wall, clearly visible on T1 sequences on thin sections with fat saturation, before (c and d) and after gadolinium injection (e and f arrow)
Arteriography
Succession of segmental stenoses and/or arterial irregularities ± associated with interposed fusiform dilatations. Vascular occlusions.
Parenchymographic defect in hypoperfused or ischaemic zones. May be associated with distal aneurysms.
Imaging
Consensus for at least long-term steroid therapy (oral and possibly with initial boluses), usually in combination with immunosuppressive therapy (monthly bolus or daily oral cyclophosphamide, azathioprine, methotrexate).
Duration of treatment according to therapeutic response (the main outcome measure must be defined at the start of treatment: clinical, imaging, CSF ?).
Generally associated with a poor prognosis.
Non-Inflammatory CNS Small-Vessel Disease
CADASIL (Fig. 7.6)
Definition and Clinical Features
CADASIL means “Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy”. Autosomal dominant disorder of small perforating arteries associated with migraine with aura (one-third of cases), recurrent subcortical infarcts, mood disorders (apathy, severe depression, episodes of melancholia and mania), pseudobulbar syndrome and dementia. Mutation in the Notch 3 gene. The vascular disease is responsible for white matter ischaemia. Death around the age of 60 years, about twenty years after the first ischaemic sign.
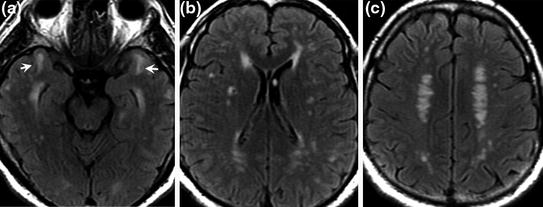
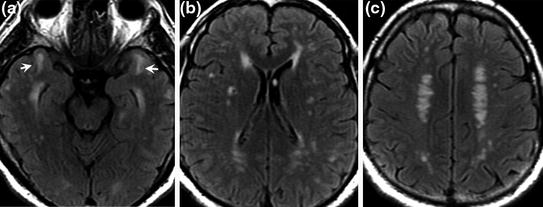
Fig. 7.6
CADASIL (Notch 3 mutation) in a 47-year-old patient. FLAIR sequence: diffuse hyperintensities of the periventricular and subcortical white matter. Constant involvement of anterior poles of the temporal lobes with white matter hyperintensities (a arrow) on FLAIR sequence
Investigations
In patients with a family history or personal history of migraine with aura, recurrent lacunar infarcts, severe leukoaraiosis on imaging: screening for Notch 3 gene mutations (more than 100 mutations have been identified).
Imaging
MRI
Diffuse nonspecific leukoencephalopathy with constant involvement of anterior poles of temporal lobes and subcortical ischaemia, visualized as hyperintensities on FLAIR and T2 images. Dilated Virchow-Robin spaces. Multiple lacunar infarcts. Diffuse microbleeds, seen as focal T2* hypointensities.
Treatment
No known treatment.
Usual stroke management.
Sneddon’s Syndrome (Fig. 7.7)
Multifocal infarcts and livedo racemosa in young subjects.
Most frequent symptom: headache. May mimic migraine with aura.
Investigations: screening for circulating anticoagulant, antiphospholipid, anticardiolipin, and anti-beta2GP1 antibodies.
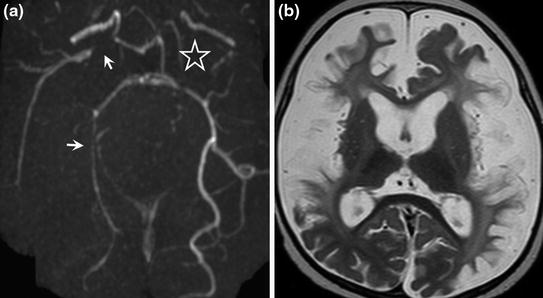
Fig. 7.7
Sneddon’s syndrome with antiphospholipid antibodies in a young patient associated with cerebral vasculitis responsible for infarction and livedo racemosa. MRI shows extensive involvement with multiple proximal vascular stenoses of the carotid and vertebrobasilar systems (a TOF sequence, inferior view, arrows) with left middle cerebral artery occlusion (a star). On T2-weighted SE sequences, multiple sequelae of extensive infarcts with diffuse parenchymal atrophy
Imaging
MRI: multiple focal white matter hyperintensities on T2-weighted sequences. Pseudo-multiple sclerosis appearance on MRI.
SUSAC’S Syndrome (Fig. 7.8)
Also called SICRET syndrome (Small Infarction of Cochlear, Retinal and Encephalic Tissue). It is a microangiopathy responsible for the occlusion of small retinal, cerebral and cochlear vessels. More common in young women. Symptoms comprise small cerebral infarcts, impaired hearing and vision.
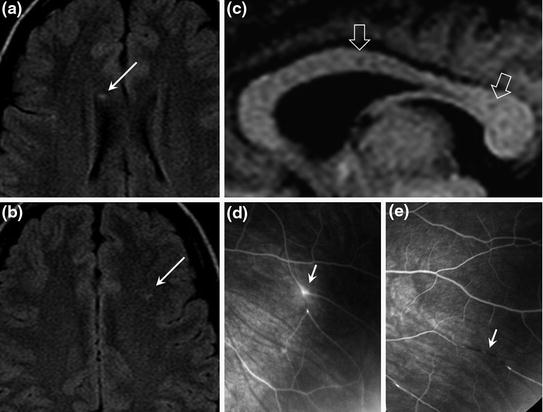
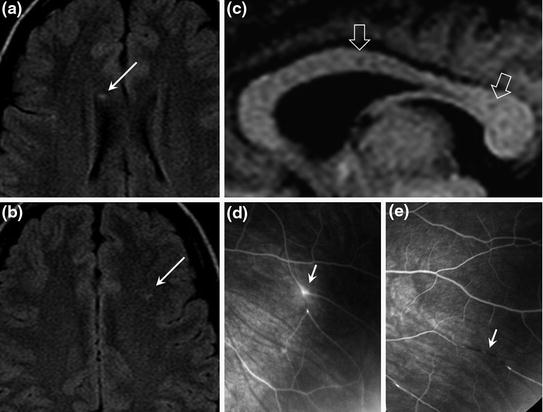
Fig. 7.8
34-year-old female with Susac’s syndrome. MRI FLAIR sequence shows focal periventricular white matter hyperintensities (a and b arrows) with suggestive central callosal lesions (c hollow arrows, central callosal holes on T1). Fluorescein angiography demonstrates fluorescein leakage (d arrow) and lesions suggestive of peripheral vasculitis (e arrow, vascular occlusion). Funduscopic views by courtesy of Dr. Yvan de Monchy, hôpital Bicêtre
Investigations
Funduscopy and fluorescein angiography (small retinal infarcts), audiometry to detect cochlear lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








