Recovery and social inclusion
The recovery model
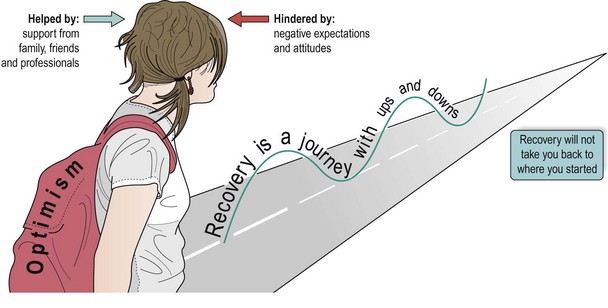
The key elements of recovery are shown in Figure 1. An important component of recovery is that patients feel they gain control over the symptoms of mental illness. However, gaining control over wider aspects of life, such as relationships, home life, employment and money is often even more important to a sense of wellbeing and quality of life. It is essential, therefore, that in treating mental illness these broader issues are taken into account, and given the same consideration as the medical treatments.
Social inclusion
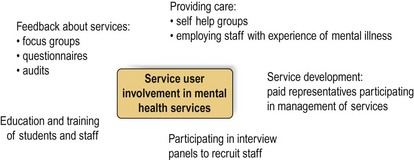
1. Stigma and discrimination. There is ample evidence of stigma and discrimination against people with mental illness. The consequences of this are that people with mental illness are more likely to have a low income, insecure housing, be unemployed and denied access to education, and have limited social networks. Negative attitudes and fear of mental illness are reinforced by media portrayals of people with schizophrenia being violent or having a split personality. Sadly, discrimination also occurs within health services. Diagnoses of mental illness are commonly cited on sick certificates, but in many cases no active treatment is delivered. The physical healthcare of people with serious mental illness is often inadequate. People with schizophrenia have a life expectancy that is 10 years shorter than average, mainly as a consequence of physical health problems. Patients report that their physical health concerns are not taken seriously by doctors, or are assumed to be manifestations of their mental illness, and this leads to reluctance to disclose symptoms. One way of addressing these issues is to involve patients (in this context the term ‘service user’ is usually used) in the running and development of services. Examples of service user involvements are shown in Figure 2.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree