Chapter 15 Respiratory management in neurological rehabilitation
Introducton
Respiratory problems are not confined to respiratory patients. Every patient has the potential to develop respiratory dysfunction. This is particularly true for patients with neurological disorders. As well as problems with reduced central drive or neuromuscular weakness associated with pathology and trauma, many neurological patients are susceptible to respiratory infections through immobility or aspiration (see Table 15.1). As respiratory dysfunction can be life-threatening, it makes sense for every physiotherapist to be competent to conduct an assessment of the respiratory system, to be aware of the common problems with which patients present, and to have a basic toolkit of interventions designed to manage such problems. This chapter will cover the areas of respiratory assessment, problem recognition and respiratory physiotherapy management in neurological patients.
Table 15.1 Clinical course for some neurological conditions commonly associated with respiratory problems
| Disorder | Clinical Course | Prevalence of Respiratory Involvement |
|---|---|---|
| CNS | ||
| Multiple sclerosis | Relapsing | Pulmonary function impaired in 63%; respiratory failure or infection causes death in 5% |
| Parkinson’s disease | Slowly progressive | Pneumonia accounts for 20% of deaths, possibly from bulbar or upper airway muscle involvement and impaired cough |
| Spinal cord | ||
| Trauma | Permanent | High lesions (C1–3) usually require long-term ventilation |
| Motor neurone | ||
| Postpolio syndrome | Very slowly progressive | Respiratory impairment usually only in those with initial respiratory muscle involvement |
| Motor neurone disease | Progressive | Death almost uniformly due to respiratory complications |
| Motor nerves | ||
| Guillain-Barré syndrome | Slowly reversible | Respiratory failure in 28% |
| Charcot–Marie–Tooth | Very slowly progressive | 96–100% have prolonged phrenic nerve conduction; 30% have vital capacity <80% predicted |
| Neuromuscular junction | ||
| Myasthenia gravis | Reversible | Aspiration pneumonia gives rise to crises with 6% mortality |
| Botulism | Slowly reversible | 8% mortality due to respiratory failure |
| Muscle | ||
| Duchenne muscular dystrophy | Progressive | Respiratory failure is major cause of death |
(Adapted from Aboussouan 2005, with permission.)
Respiratory assessment
A comprehensive respiratory assessment as outlined in Box 15.1 is only possible in a patient in a stable situation. If any ‘red flags’ are noticed (see Box 15.2), the assessment may need to be adapted and shortened. Although it is generally recognized that neurological disease may result in respiratory dysfunction, its presentation in such patients may be atypical, because of wider effects of the underlying condition (Polkey et al., 1999). The tests starred (*) in Box 15.1 will now be described further in relation to neurological patients.
Box 15.1 Elements of a respiratory assessment
General end-of-bed observations:
History (from patient/relatives/friends):
Respiratory bedside/laboratory testing:
Box 15.2 Respiratory ‘red flags’
Arterial blood gases
Arterial blood gas (ABG) sampling is performed to obtain accurate measures of arterial oxygen (PaO2), arterial carbon dioxide (PaCO2), and blood acidity/alkalinity (pH); these variables combined with body temperature allow for calculation of bicarbonate (HCO3) and arterial oxygen saturation (SaO2). Both PaO2 and PaCO2 can be affected by respiratory muscle weakness. Mild weakness leads to slight hypoxaemia (low oxygen, i.e. PaO2 <8 kPa/<60 mmHg) and hypocapnia (low carbon dioxide, i.e. PaCO2<4.7 kPa/<35 mmHg); severe weakness causes hypercapnia (high carbon dioxide, i.e. PaCO2 >6kPa/>45 mmHg), but only when muscle strength is <40% predicted (ATS 2002). However, ABG derangement is a late feature in neuromuscular disease, so normal results are compatible with significant weakness of the respiratory muscles (Hutchinson & Whyte, 2008). Patients with established respiratory failure from neuromuscular weakness will show hypoxaemia and a compensated respiratory acidosis (raised PaCO2 and HCO3 with a normal or mildly reduced pH).
Vital capacity
Vital capacity (VC) is the volume change at the mouth between full inspiration and complete expiration (see Figure 15.1). VC can be measured using conventional spirometers or recorded from equipment used to measure static lung volumes and their subdivisions. Guidelines for measurement have been published by the American Thoracic Society/European Respiratory Society task force (Wanger et al., 2005).
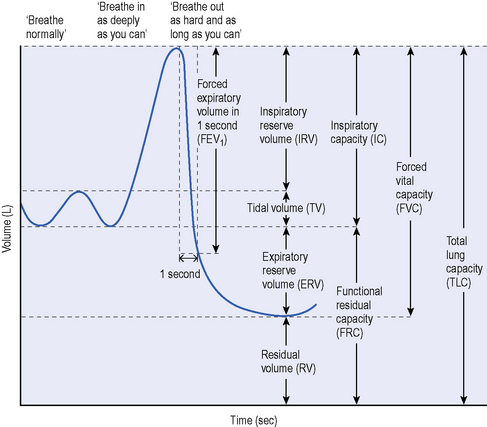
Figure 15.1 Lung volumes and capacities in neurological disease.
(From Aboussouan LF. Respiratory disorders in neurologic diseases. Cleve Clin J Med 2005; 72:511–520. Reprinted with permission. Copyright © 2005 Cleveland Clinic. All rights reserved.)
In acute neuromuscular disorders the VC and oxygen saturation should be rechecked at frequent intervals. A VC <1 L in an adult (<15 mL/kg), a fall in VC by more than 50% on serial testing, or onset of bulbar palsy are all indications to involve the intensive care unit (Hutchinson & White, 2008). In chronic neuromuscular disorders, monitoring can be less frequent, but a serial fall in VC (particularly a fall below 1.2–1.5 L or <40–50% of predicted) indicates a need for further respiratory assessment (Hutchinson & Whyte, 2008).
Peak cough flow
A normal cough requires the ability to generate sufficient inspiratory and expiratory power and a functional glottis.Ability to cough effectively is therefore compromised by either inspiratory or expiratory muscle weakness. However, expiratory muscle weakness has greater impact as mild to moderate expiratory muscle weakness can result in a weak cough, even if inspiration is normal (Boitano, 2006). In some neurological disorders, such as bulbar type motor neurone disease (MND; see Ch. 8), a functional glottis may be absent. Formal cough assessment requires the insertion of gastric balloons and is conducted in specialized laboratories, but cough strength can be assessed at the bedside using peak cough flow (PCF). PCF is a measure of maximal airflow generated during a cough manoeuvre. It provides a global indicator of cough strength that correlates well with the ability to clear secretions.
The recent joint guidelines from the British Thoracic Society (BTS) and Association of Chartered Physiotherapists in Respiratory Care for respiratory physiotherapy (Bott et al., 2009), include a guide for recording PCF in patients with neuromuscular weakness. It can be measured through either a mouthpiece or face mask attached to a peak flow meter and expressed in litres/minute or litres/second. The patient should be instructed to breathe in as deeply as possible and cough hard into the device. PCF is expected to be higher than peak expiratory flow, but in patients with bulbar dysfunction, this difference is not seen – potentially offering a way to monitor the onset of bulbar involvement (Boitano, 2006).
PCF is dependent on effort and lung volume, with cooperation being essential. The largest value from at least three acceptable attempts is usually recorded. Normal PCF is around 360 to 840 L/minute (Hutchinson & Whyte, 2008). Airway clearance becomes impaired and the risk of serious infection increases when PCF<160 L/minute, so in chronic progressive conditions, airway clearance techniques should be taught before these levels are approached (Tzeng & Bach, 2000). It has been suggested that any neuromuscular patients with a PCF<270 L/minute should be considered at risk of respiratory complications.
Inspiratory/expiratory pressures
Guidelines for testing the respiratory muscles have been published by the American Thoracic Society (2002). Inspiratory and expiratory pressures are recorded to assess respiratory muscle strength, but should be viewed as indices of global respiratory muscle output rather than as direct measures of their contractile properties (ATS, 2002). Mouth and nasal pressures can be recorded at the bedside using hand-held pressure meters. These volitional bedside tests are simple, portable and inexpensive; but their accuracy and reliability has been questioned because of their dependence on maximal effort and their significant learning effect. Non-volitional tests such as phrenic nerve stimulation are more reliable, but are expensive and confined to specialist centres.
Patients are normally seated and noseclips are not required. Careful instruction and encouraged motivation are essential. Measurements require maximal inspiratory or expiratory efforts against a quasi occlusion. The pressure must be maintained for at least 1.5 seconds, so that the maximum pressure sustained for 1 second can be recorded. The maximum value of three manoeuvres that vary by less than 20% is usually recorded, but some authors have recommended that more measures are needed to reach a true maximum, and even low variability between measures may not guarantee that maximal efforts have been made (Aldrich & Spiro, 1995). Although simple in principle, the manoeuvres are difficult for many patients and require a good seal around the mouthpiece. Low values may therefore be due to true muscle weakness, or a submaximal effort, or air leaks, e.g. in the case of facial muscle weakness. The sniff is an alternative manoeuvre that is more natural and easier for most patients (see section on Sniff test).
The normal ranges for PImax and PEmax are wide, so that values in the lower quarter of the normal range are compatible both with normal strength and with mild or moderate weakness. In adults a PImax of more than 80 cmH2O in males, or 70 cmH2O in females, excludes clinically significant respiratory muscle weakness (Hutchinson & Whyte, 2008).
Sniff test
A sniff is a short, sharp voluntary inspiratory manoeuvre involving contraction of the diaphragm and other inspiratory muscles. Sniff nasal inspiratory pressure (SNIP) has been proposed as a volitional, non-invasive measure of inspiratory muscle strength. Peak nasal pressure is measured in one occluded nostril during a maximal sniff, performed from relaxed end-expiration through the other open nostril. Portable commercial systems are available for measuring SNIP at the bedside. Patients should be encouraged to make maximal efforts, with a rest between sniffs. Most patients achieve a plateau within 5–10 attempts. A sniff test is not suitable in patients with nasal congestion, which leads to falsely low values (Fitting, 2006). The sniff is easily performed by most patients, requires little practice and is relatively reproducible. It is therefore a useful voluntary test for evaluating diaphragm strength in the clinical setting, giving equal or greater pressures than PImax. However, SNIP and PImax are not interchangeable and should be considered as complementing one another for the assessment of inspiratory muscle strength.
There are reference values for SNIP in adults (Uldry & Fitting, 1995) and children (Rafferty et al., 2000). Surprisingly, SNIP is similar in children and adults, despite a large difference in respiratory muscle mass. Values of maximal SNIP greater than 70 cmH2O (males) or 60 cmH2O (females) are unlikely to be associated with significant inspiratory muscle weakness (Hutchinson & Whyte, 2008). The SNIP test appears particularly suited to neuromuscular weakness because it obviates the use of a mouthpiece and because it is easily mastered by most patients. However, assessment of severe muscle weakness should not rely on SNIP alone, but should include other tests such as PImax, vital capacity, nocturnal oximetry or ABGs (Fitting, 2006).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







