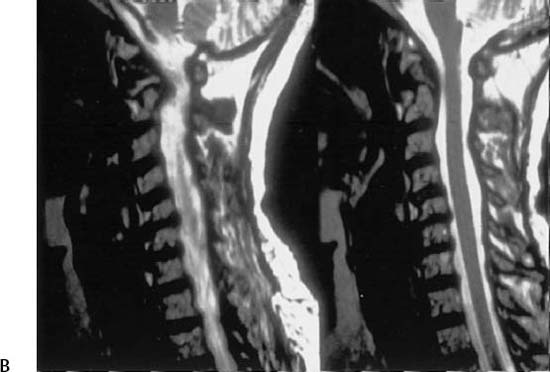
21 I. Rheumatoid arthritis A. Clinical findings 1. Most commonly affects the cervical spine 2. Within 5 years of serological diagnosis, 30 to 50% develop subluxation. 3. Most common during the third decade 4. Three-to-one female-to-male ratio 5. Insidious onset, symmetrical polyarthritis, constitutional symptoms, and variable clinical course a. Patients are at risk for sudden death. B. Pathogenesis 1. Unknown antigens a. Epstein-Barr virus b. Bacteria cell wall products c. Collagen II d. Mycoplasma 2. Genetically susceptible individuals a. HLA-DR4 type 3. Antibody formation and cellular interaction a. Monocyte b. B and T lymphocytes c. Immune complex formation (1) Rheumatoid factor—immunoglobulin M 4. Phagocytosis of immune complexes a. Synovial cells type A and polymorphonuclear neutrophilic leukocytes (PMNs) (1) Complement activation 5. Chemotaxis of inflammatory cells a. Production of proteolytic enzymes and prostaglandins 6. Cartilage destruction a. Collagenase b. Proteolytic enzymes from PMNs c. Synovial cells and chondrocytes 7. Periarticular osteoporosis due to disuse and prostaglandins 8. Subluxation, dislocation, deformity, and ankylosis C. Pathology 1. Synovium a. Synovitis with villi infiltrated with lymphocytes and plasmacytes b. Surrounding edema and fibrin 2. Pannus a. Proliferation of mesenchymal cells and vascular granulation invading the cartilage from the periphery 3. Rheumatoid nodules a. Fibrinous necrosis in the center with surrounding layer of palisading epithelial cells D. Cervical spine deformity 1. Instability depends on the severity of the disease process 2. Subluxation appears one decade after the disease onset 3. Radiographic progression of subluxation has been observed in 35 to 80% of patients. a. Five-year mortality rate of 17% 4. Atlantoaxial subluxation (Fig. 21–1) a. The normal anterior atlantodens interval (AADI) is 3 mm in adults and 4 mm in children. (1) AADI greater than 5 mm represents instability. Figure 21–1 (A) Lateral radiograph of a rheumatoid arthritis patient with C1–C2 instability. The atlantodens interval is measured to be 17 mm, and the PADI/SAC is only 8 mm on flexion. A SAC of 13 mm or less represents a significant risk for the development of neurological compromise. (B) Sagittal T2-weighted MRI taken of the same patient demonstrating that the spinal cord is decompressed in extension. (3) AADI is an unreliable predictor of paralysis because of poor correlation between the AADI and the degree of cord compression as shown by magnetic resonance imaging (MRI). (4) Posterior atlantodens interval (PADI) has been found to be a better predictor of paralysis. (a) Critical lower limit is 14 mm. (b) Important to note that PADI is not the same as space available for the cord. (i) In rheumatoid arthritis patients, retro-odontoid synovial pannus may occupy as much as 3 mm of space. b. Weak transverse ligament and synovitis of atlantoaxial and atlanto-odontoid joints c. Symptoms (1) Neck pain (2) Headache (3) Myelopathy (a) Paresthesias (b) Abnormal gait (c) Bowel/bladder difficulties (d) Difficulty with fine motor control 5. Atlantoaxial impaction or basilar invagination a. Characteristics (1) Superior migration of the odontoid (SMO) (2) Vertical subluxation of the axis (3) Pseudobasilar invagination b. Synovitis and cartilage destruction of the occipitoatlantal and atlantoaxial joints c. Symptoms include occipital headache, myelopathy, or brain stem compression signs d. Radiographic landmarks (1) McGregor’s line (a) Connects the posterior margin of the hard palate to the most caudal point of the occiput (b) Positive if >4.5-mm odontoid projection above the foramen magnum (2) Ranawat’s C1–C2 index (a) Distance between the center of the pedicle of the axis and the transverse axis of the atlas (b) Less than 13 mm in women and <15 mm in men are abnormal. (3) McRae’s line (a) Connects the anterior and the posterior margins of the foramen magnum (i) Tip of the odontoid should lie 1 cm below this line. (4) Redlund-Johnell occiput-C2 index (a) Perpendicular distance from the middle of the lower end plate of the axis to McGregor’s line (b) Less than 34 mm in men and <29 mm in women are abnormal. 6. Subaxial subluxation a. Synovitis of facet joints, intervertebral disks (spondylodiscitis), and ligament involvement b. Multiple-level involvement (1) Particularly common at C2–C3 and C3–C4 region (2) Degenerative involvement typically occurs at C5–C6 c. End plate erosions are present in 12 to 15% of patients. d. MRI is indicated whenever there is suspicion of instability on plain radiographs. II. Predictors of neurological recovery A. Ranawat classification 1. More severe preoperative neurological deficits tends to have a poorer neurological recovery. B. Location of disease 1. The more proximal the pathology, the worse the prognosis. C. Preoperative PADI of 14 mm or greater predicts a potentially significant motor recovery after appropriate surgery. 1. In contrast, PADI <10 mm has a poor prognosis. D. Postoperative subaxial canal diameter <14 mm indicates a poor prognosis. III. Indications for surgical stabilization (Fig. 21-2) A. Definite indications 1. Intractable pain 2. Neurological defect B. Atlantoaxial subluxation 1. PADI ≤ 14 mm warrants an MRI scan.
Rheumatoid Arthritis

Neupsy Key
Fastest Neupsy Insight Engine









