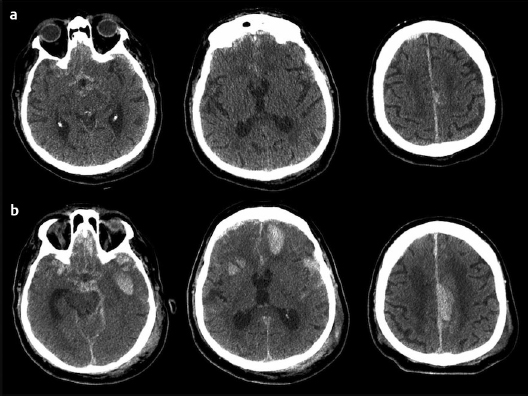
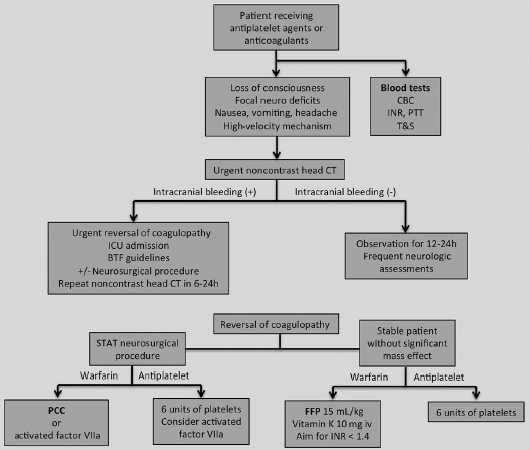
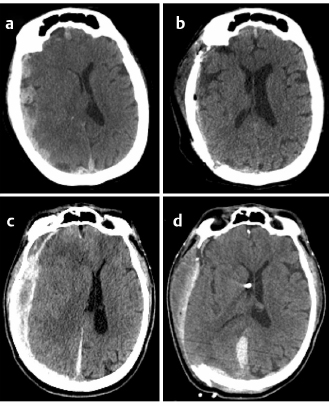
23 Trauma is the leading cause of death and disability in children, adolescents, and young adults. Injuries to the central and peripheral nervous systems can lead to disastrous consequences if not treated in a timely manner. Numerous innovations have advanced the field of neurotraumatology in the past few decades, with the goals of diminishing secondary injuries and restoring normal physiology. However, there remains great variability in the management of neurotrauma due to the complexity of neurophysiology, the heterogeneity of lesions, and the lack of randomized controlled studies and comparative effective research. Patient characteristics and comorbidities are crucial considerations in the initial evaluation of the neurotrauma patient. The assessment of the coagulation parameters in this population is important not only at the time of presentation but also during the entire hospitalization. Coagulopathies can result from deficiencies or disorders of the coagulation pathways, such as hemophilia, thrombocytopenia, or liver disease. Medical therapy with oral anticoagulants, antiplatelet, anti-inflammatory, or chemotherapy agents also contribute to bleeding diatheses. Finally, trauma itself can lead to coagulation abnormalities. Currently, more than 1% of the population receives oral anticoagulation therapy for various cardiovascular conditions. Although several recent studies have focused on traumatic brain injury (TBI) in patients receiving anticoagulation and antiplatelet therapies, there are no strict guidelines regarding the management of these complex patients. The literature, composed mostly of retrospective studies, has shown conflicting results regarding TBI in the setting of preinjury anticoagulation and antiplatelet usage, with a trend toward worse outcome. The management of these patients raises multiple questions regarding initial blood testing and imaging, reversal of anticoagulant agents, timing of follow-up imaging, and resumption of the oral anticoagulants or antiplatelet therapies. Anticoagulation therapies are commonly indicated for the prevention of thromboembolic complications of atrial fibrillation, deep venous thrombosis, pulmonary emboli, extracranial vascular disease, prosthetic heart valves, ischemic stroke, and ischemic heart disease. The most frequently used medication is warfarin, an oral anticoagulant that inhibits vitamin K–dependent clotting factors. Therapeutic monitoring is crucial with warfarin administration, as it has numerous interactions with food and medications. Advanced age and concomitant diseases can also affect its metabolism. Low molecular weight heparin (LMWH) is occasionally used instead of warfarin, especially as a bridging therapy in certain clinical conditions. Direct thrombin inhibitors (DTIs) are a new class of oral anticoagulation medication that was recently approved by the Food and Drug Administration (FDA) for the prevention of thromboembolism in atrial fibrillation. Dabigatran etexilate has a predictable pharmacokinetic profile allowing a fixed dose to be given without the need to monitor the anticoagulation status.1 Spontaneous intracranial hemorrhage is a well-known complication of long-term anticoagulation therapy, with an annual risk of 0.3 to 0.6%.2 In a meta-analysis by Linkins et al,3 21% of the major bleeds associated with anticoagulation were ICHs. Intensity of anticoagulation (international normalized ratio [INR] > 4), increased variations in INR, and advanced age have been associated with increased risk for ICH.2 There is conflicting data regarding outcomes following TBI in the setting of prehospital antiplatelet and anticoagulant therapies. The results are confounded by the retrospective nature of the study series, the heterogeneity of patient populations, and the inconsistencies in the categorization of injury patterns and clinical classifications. There appears to be a trend toward higher morbidity and mortality associated with TBI in patients taking anticoagulation or antiplatelet agents. These results, however, need to be confirmed with prospective studies. Spontaneous ICHs associated with warfarin therapy with an INR greater than 3.0 are associated with a larger hematoma size, higher probability of hematoma progression in the first 24 to 48 hours, and delayed hematoma expansion up to 7 days when compared with spontaneous ICH in the absence of anticoagulation.4–6 Several retrospective studies have shown an up to five times increased risk of mortality in warfarin-treated patients after TBI when compared with non-anticoagulated patients.7–10 However, similar results were not seen in other larger observational studies.11–13 Age and initial Glasgow Coma Scale (GCS) score continue to be the most important predictors of mortality and outcome in the trauma population. There is a trend toward clinical and radiological deterioration in patients receiving preinjury warfarin therapy who present with an abnormal head computed tomography (CT) but good neurologic status. Although these patients may appear to have only mild head injury, they are at high risk of delayed neurologic deterioration, and rapid correction of INR may lead to a lower mortality in these patients.9,10,12,14 A retrospective study by Howard et al15 found that preinjury warfarin therapy had the greatest negative impact on mortality in elderly patients who presented with an initial GCS of 14 to 15 after a fall. These patients had a 25% chance of positive findings on head CT and a 2.3 increase in mortality compared with those without preinjury anticoagulation. Several retrospective studies have analyzed the effects of preinjury antiplatelet therapy in TBI patients. These studies have demonstrated conflicting results due to their retrospective nature, variability in the antiplatelet agents, and the inability to objectively quantify the effects of antiplatelet agents.16 Several studies have shown increased mortality risk with antiplatelet agents,7,17–19 whereas others have shown no higher risk when adjusted for age and severity of injury.13 A recent retrospective study by Siracuse et al19 found that traumatic ICH in patients taking antiplatelet agents has increased 5-fold in 2007–2008 compared with 1999–2000. The mortality rate in the antiplatelet group was 17%, which is similar to the mortality rate associated with warfarin therapy.19 Similar results were obtained in a retrospective study examining 109 trauma patients taking antiplatelet therapy with evidence of ICH on the initial head CT. These patients were more likely to present with a higher grade of hemorrhagic injury and have a higher mortality rate (18%) than did similarly injured patients not receiving antiplatelet therapy (Fig. 23.1). Interestingly, the high mortality was not caused by hemorrhage progression (as in warfarin patients) but by either the severity of the hemorrhage at the time of injury or the exacerbation of other medical conditions.17 Fig. 23.1a,b Progression of intracranial hemorrhage with preinjury antiplatelet therapy. An 81-year-old man with syncope and a fall from the standing position. (a) Initial noncontrast head computed tomography (CT) showed bifrontal contusions and subarachnoid hemorrhage. (b) Follow-up noncontrast head CT 3 hours later after neurologic deterioration showed enlargement of contusions. The patient was later found to be taking prasugrel (a third-generation oral thienopyridine). The management of patient with suspected TBI receiving antiplatelet or anticoagulation therapy must take into account the mechanism of injury, and the complete history and physical examination, including any loss of consciousness (LOC), seizure, headache, nausea or vomiting, or focal neurologic deficits (Fig. 23.2). A high index of suspicion is warranted, and there should be a low threshold for obtaining cerebral CT imaging even in the absence of LOC or focal neurologic findings.15,20,21 In fact, the American College of Emergency Physicians specifically recommends a head CT in the presence of coagulopathy.22 Some studies have found that anticoagulated patients with an initial GCS of 15 and a normal head CT were still at risk of delayed neurologic deterioration and should be observed for 12 to 24 hours with frequent neurologic assessments.12 Patients with TBI, especially those with preinjury anticoagulation or antiplatelet therapy, should be admitted to the intensive care unit (ICU) and managed as per the Brain Trauma Foundation guidelines.23 Fig. 23.2 Management of patients with preinjury antiplatelet or anticoagulation therapies. BTF, Brain Trauma Foundation; CBC, complete blood count; CT, computed tomography; FFP, fresh frozen plasma; ICU, intensive care unit; INR, international normalized ratio; PCC, prothrombin complex concentrate; PTT, partial thromboplastin time; STAT, at once; T&S, type and screen. Any positive finding on the head CT should prompt the reversal of anticoagulation or antiplatelet therapy. Infusion of fresh frozen plasma (FFP) at 15 mL/kg and vitamin K injections can be used for correction of coagulopathy secondary to warfarin therapy. Platelets should be transfused for those receiving antiplatelet therapy. In patients requiring emergency neurosurgical procedures, including invasive neuromonitoring, the administration of prothrombin complex concentrate (PCC) or activated factor VIIa should be considered (Fig. 23.3). These agents have been shown to be safe and can normalize the INR quicker than the administration of FFP. Patients with preinjury antiplatelet therapy should receive at least six units of platelets at the time of the procedure, and activated factor VIIa may also be considered if profuse bleeding is seen during the operative procedure.16,24,25 Currently, there is no antidote to reverse the effects of DTIs, though hemodialysis, activated factor VIIa, and PCC may be considered during emergencies.1 Although there are no established guidelines regarding follow-up imaging, it is common practice to repeat cerebral imaging 6 to 24 hours after the first positive radiographic findings. Changes in neurologic examination or neuromonitoring should prompt reevaluation with appropriate radiographic testing. There is currently no guideline for determining the optimum timing for the reintroduction of anticoagulation or antiplatelets therapy after traumatic ICH. The indications for anticoagulation and the risks of withholding treatment must be weighed against the risks of rebleeding on an individual basis. Although most authors feel that it is generally safe to resume anticoagulation after of 1 to 2 weeks, some advocate waiting 10 to 30 weeks.26–28 A common practice is to repeat cerebral imaging before and after the reintroduction of anticoagulation and to use preferentially anticoagulant medications that can be reversed. The patient should be observed closely following the resumption of anticoagulation. Chronic subdural hematoma (CSDH) is frequently seen in elderly patients and is thought to be the result of a traumatic tear in a parasagittal vein. Surgical treatments include bedside drainage, bur hole evacuation, and craniotomy. CSDHs have high rates of recurrence, ranging from 9.2 to 26.5%, often necessitating repeat evacuations. The incidence of CSDH and the risk of reaccumulation following evacuation in patients receiving antiplatelet or anticoagulation therapy are unclear. Anticoagulation usage seems to be more frequent in patients presenting with CSDH without any obvious history of head trauma.29 However, the overall mortality and morbidity did not appear to be affected.30 The recurrent rate of CSDH following evacuation appears to be higher in patients maintained on antiplatelet therapy before surgery. Patients receiving warfarin therapy, whose coagulopathies were normalized prior to surgery do not appear to be at elevated risk for reaccumulation of their CSDH.31–34 Some attribute this difference to the difficulty of reversing antiplatelet agents versus warfarin therapy. However, given the heterogeneity the study populations, definitive recurrence rates cannot be determined. Follow-up imaging should be strongly considered, especially in those receiving antiplatelet treatment. The timing of reintroduction of antiplatelet or anticoagulation therapy after successful surgical treatment of CSDH is also unclear. In the majority of patients, the associated risk of withholding the medication seems to be low. A period of 3 to 8 weeks before the reintroduction of anticoagulation is often cited in the literature, but this delay should be personalized according to the indication for anticoagulation in each patient.31,32 Even in a high-risk patient (cardiac valve replacement), stopping anticoagulation for 1 to 2 weeks appears to be safe.35,36 A follow-up imaging before the reintroduction of anticoagulation is a common practice. Although spine fractures are common findings following trauma, the exact incidence of posttraumatic spinal hematoma is difficult to assess. Posttraumatic epidural hematoma is reported in 52% of patient with spine fracture when a magnetic resonance imaging (MRI) scan is ordered within the first 48 hours. The 6-month prognosis is the same in patient with spinal fractures, with or without epidural hematoma.37 According to a meta-analysis of 613 patients with spinal hematomas, the localization of spinal hematomas is mostly epidural (75%), follow by subdural/subarachnoid (20%), and intraparenchymal in less than 1%.38 Anticoagulation was the etiology in 17% of the patients, representing the second most common cause of spinal hematoma. Anticoagulation with warfarin was the most common culprit, rather than antiplatelet agents. Clinically significant posttraumatic spinal hematoma was found in 10% of patients.38 Of these, 55% were associated with spinal fractures. The majority of cases were cervicothoracic or thoracolumbar epidural hematoma. Most patients with spinal hematoma present with acute back pain, with or without radiculopathy, that progresses rapidly to a sensorimotor deficit. An MRI scan is the gold standard exam to delineate the location and anatomy of the hematoma. Emergency reversal of anticoagulation with timely surgical management including laminectomy with evacuation of the hematoma and spinal cord decompression offer the best chance of neurologic recovery.39,40 A complete recovery is expected in 40% of patient, and 34% will have a mild to severe neurologic deficit. The two most important prognostic factors are the preoperative neurologic status of the patient and the timing of the surgery. Early surgery within 24 hours offers the best chance of recovery, with the greatest recovery if decompression is performed within 8 hours. Although recovery after 24 hours is unlikely, some studies have demonstrated neurologic improvements even following decompression after 48 hours.38 The timing of the resumption of anticoagulation in this population has not been systematically studied, but most authors recommend waiting for 7 to 14 days after surgery, with special attention to the neurologic exam when anticoagulation is reinitiated.41 There is a paucity of studies regarding the risk of peripheral nerve injury associated with treatment with antiplatelet or anticoagulation therapy. Most of the literature is composed of case reports and small series of patients presenting with spontaneous hematoma causing direct compression of peripheral nerves or plexus. Retroperitoneal hematoma, whether spontaneous or posttraumatic, has been known to occur in patients receiving anticoagulation or antiplatelet therapy.42,43 The hematoma is usually located in the iliacus muscle or in the retroperitoneal space and causes direct compression on the lumbosacral plexus. Patients present with acute onset of severe groin/abdominal pain followed by a variable picture of femoral neuropathy including numbness in the anteromedial thigh and weakness in the iliopsoas and quadriceps muscle. The diagnosis is made by abdominal ultrasound, abdominal pelvic CT, or MRI. Although the treatment is controversial, most authors agree that surgical drainage of the hematoma (ultrasound guided or through a limited retroperitoneal incision) offers the best chance of recovery in the presence of progressive neurologic deficit. The coagulopathy should also be reversed using the appropriate treatment. Other forms of compressive neuropathy such as acute carpal tunnel syndrome has also been described in anticoagulated patients.44 Although infrequent, significant bleeding and neurologic injury have been reported following regional anesthesia involving peripheral nerve, brachial, and lumbosacral plexus, and paravertebral blocks. Strict recommendations for regional anesthesia in patients under antiplatelet or anticoagulation therapy have been published and are beyond the scope of this chapter.45 Increasing numbers of patients treated with antiplatelet or anticoagulation therapies are being evaluated after sustaining neurotrauma. These patients must be considered at high risk for neurologic deterioration, and any suspicion of injuries to the central nervous system must be dealt with promptly. Currently, no guideline exists for the management of these complex patients due to the lack of level 1 evidence. For patients receiving anticoagulation with warfarin who have suffered a traumatic lesion to the nervous system, the coagulopathy should be reversed using FFP and vitamin K. If an emergency neurosurgical procedure is indicated, rapid normalization of the INR may be achieved with the administration of PCC or activated factor VIIa. However, their use in trauma has never been compared with FFP and vitamin K in a randomized controlled study. The management of patients receiving antiplatelet therapy is less clear. Transfusion of platelets will reduce bleeding in unstable patients or if an emergency neurosurgical procedure is necessary. After the acute event, the decision to resume anticoagulation therapy should be considered on individual basis, and the indications, risks, and benefits of those treatments must be taken into account. Repeat imaging before and after resumption of the anticoagulation and antiplatelet therapies should be considered. Overall, more prospective research and comparative effectiveness research are needed to address these important questions. KEY POINTS • The literature concerning the use of preinjury antiplatelet and anticoagulation therapy in nervous system trauma is mostly retrospective and confounded by the heterogeneity of the studied populations and the study methods. • An extremely high index of suspicion is imperative in patients receiving antiplatelet or anticoagulant therapy who have sustained traumatic injuries, as they are at high risk of neurologic deterioration. • The rapidity of the reversal of the coagulopathy must take into account the neurologic state of the patient, the radiological findings, and the need for emergency neurosurgical procedure. • Resuming anticoagulation following neurotrauma should take into account indications, risks, and benefits of the therapy and imaging before and after the initiation of the treatment is strongly recommended.
Risk of Anticoagulants and Antiplatelet Agents in Trauma Patients
Anticoagulant and Antiplatelet Agents
Specific Risks Associated with Preinjury Anticoagulation or Antiplatelet Therapies
Traumatic Brain Injury and Warfarin
Traumatic Brain Injury and Antiplatelet Agents
Management of a Traumatic Brain Injury Patient Receiving Antiplatelet or Anticoagulation Therapy
Timing for Resuming Anticoagulation After Traumatic Brain Injury
Chronic Subdural Hematoma
Traumatic Spinal Hemorrhage
Traumatic Nerve Injury Associated with Antiplatelet or Anticoagulation Therapy
Conclusion
Risk of Anticoagulants and Antiplatelet Agents in Trauma Patients
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree