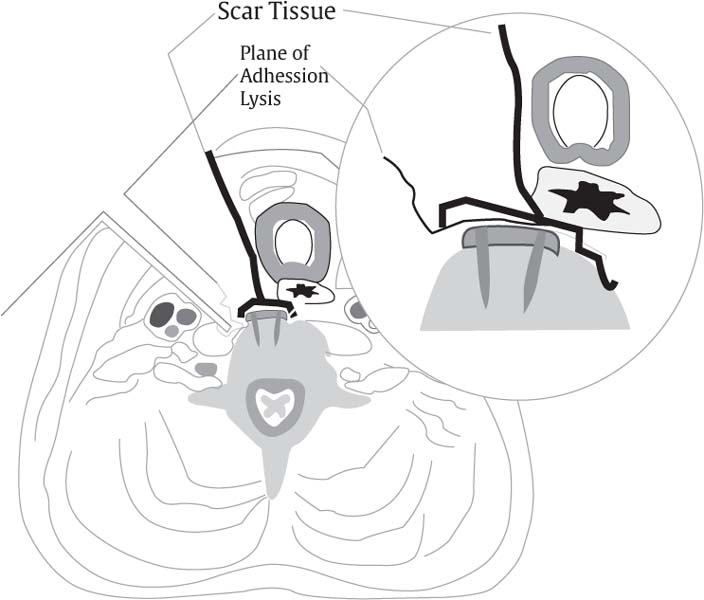
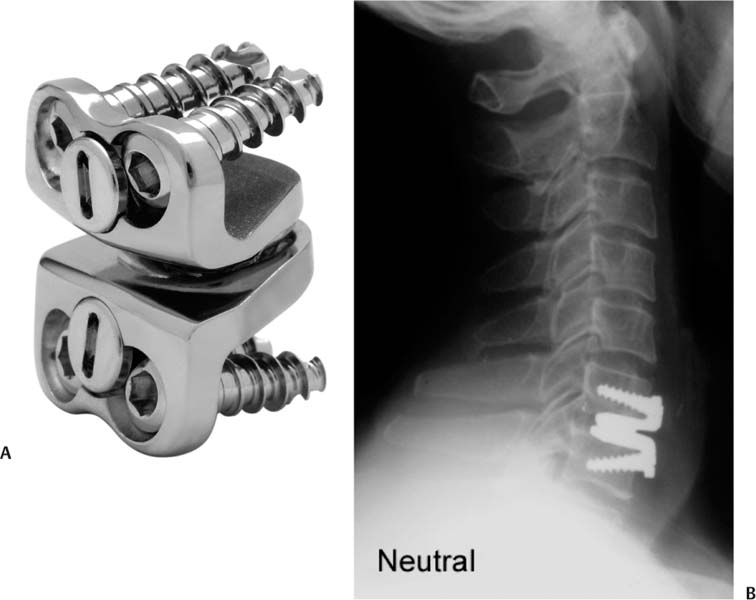
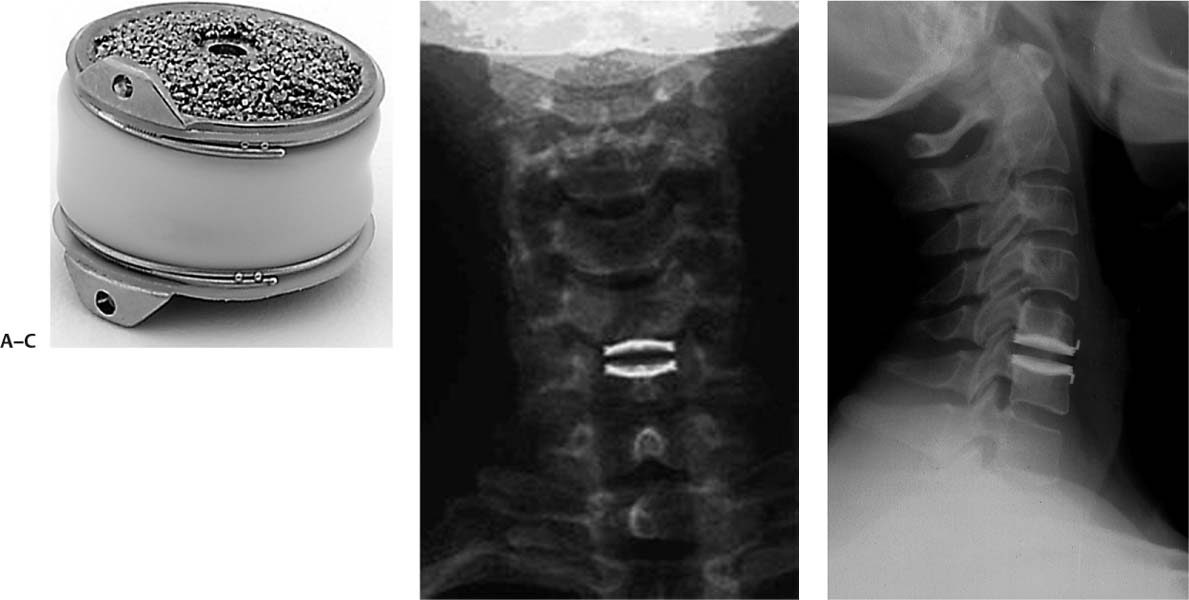
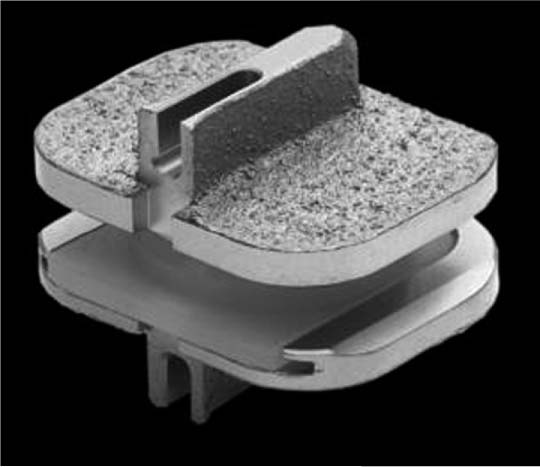
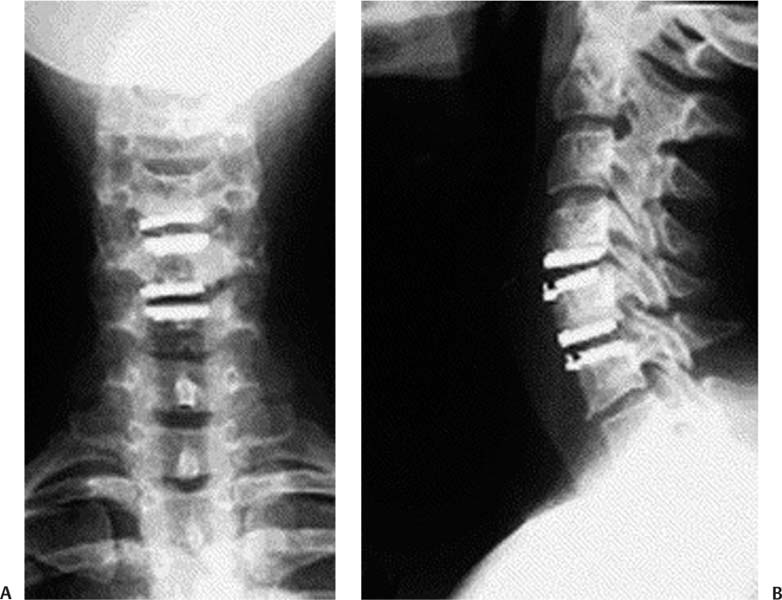
24 Since its development in the 1950s, anterior cervical diskectomy and fusion (ACDF) has proven to be a successful and versatile surgical procedure. Large clinical series have produced excellent results. Gore and Sepic1 reported on 146 patients with a 5-year follow-up. Ninety-seven percent achieved a solid arthrodesis radiographically; 78% experienced complete pain relief, whereas 18% had partial relief. Only 4% showed no improvement in their pain. The authors had no serious complications in their series. Bohlman et al2, in another large series with long-term follow-up, had 108 of 122 patients with no impairment of function, and who were able to resume normal activities. Numerous studies have produced similar results. The use of plating and allograft have, diminished pseudarthrosis and graft site complications.3 However, several studies have revealed the limitations of ACDF. While ACDF provides an excellent solution for anterior pathology, the arthrodesis alters the biomechanics of the cervical spine. Pospiech et al,4 in a cadaveric biomechanical study, found increased intradiskal pressures adjacent to simulated fusion, especially at the levels inferior to the fusion. Eck et al5 also studied adjacent-level intradiskal pressure and segmental motion in a cadaveric model. They found significantly increased intradiskal pressures and motion at the segments adjacent to the simulated fusion. The altered biomechanics decrease the diffusion characteristics of the affected disk, leading to accumulation of waste products, increased lactate levels, decreased pH levels, and subsequent cell death.6,7 Increased compression forces may lead to increased type 1 collagen, decreased proteoglycans, chondroitin sulfate, and type 2 collagen, thus disk degeneration.8 Large clinical series of patients undergoing ACDF bear out the potential problems of adjacent segment degeneration (ASD). Gore and Sepic,9 in a series of 50 ACDF patients followed an average of 21 years, had 48 patients with initial pain relief. Long term, 32 of the patients remained pain free; 16 developed recurrent pain an average of 7.2 years postoperatively, eight of whom required further surgery. Radiographically, 48 of the 50 patients developed adjacent segment disease, 19 both above and below the index level, 21 above only and eight below only. Only two patients had no degenerative changes long-term. The oft-quoted paper by Hilibrand et al10 follows 374 patients long term after ACDF. The authors showed a relatively constant rate of symptomatic adjacent segment disease of 2.9% per annum. By survivorship analysis, 25.6% of their ACDF patients at 10 years postoperatively will have new disease at an adjacent level. Other findings included highly significant (p < 0.0001) differences in adjacent segment disease by level, with these changes occurring most commonly at C5–C6 and C6–C7, and adjacent segment disease significantly lower in a multilevel as opposed to a single-level fusion. Lastly, two thirds of the patients with new onset ASD failed conservative care and required additional surgery. Goffin et al11 evaluated a smaller series of patients undergoing ACDF for traumatic as well as degenerative conditions. Follow-up was from 5 to 9 years. Sixty percent of patients developed ASD, with the rate no different in the younger traumatic patients compared with the relatively older degenerative patients. They saw more ASD in patients undergoing lower cervical fusion, but in contradistinction to Hilibrand et al,10 they saw higher ASD rates in multilevel fusion. Goffin et al concluded that the biomechanical alteration of the disk adjacent to a fusion was the most significant factor contributing to ASD. Goffin et al12 reported on another series of ACDF patients consisting of 180 patients followed for an average of 8.3 years. There were equal numbers of patients with traumatic versus degenerative diagnoses. Ninety-two percent of the patients developed ASD, with similar rates again seen between the younger trauma patients and the older degenerative patients. These findings led the authors to again conclude that the biomechanical effect of fusion contributed to the progression of disk degeneration. Their reoperation rate for symptomatic ASD was 6.1%, distinctly lower than that for Hilibrand et al10 (Fig. 24.1). A heightened awareness of the risk of dysphagia after ACDF arose during the current decade. Edwards et al13 evaluated the incidence of dysphagia after ACDF in surgeons’ clinical records compared with the patients’ reporting via a mailed survey. They found dysphagia to be underreported in the surgeons’ records by 76%. Bazaz et al14 followed 224 patients who underwent an ACDF using the Smith-Robinson technique via a left-sided approach. Because no validated dysphagia scale was available, Bazaz and Yoo created an instrument to follow these patients, based on the severity of the dysphagia with both solids and liquids. At 1 month, 50.3% of patients had some swallowing difficulty, dropping to 12.5% at 1 year. No specific risk factors were identified in surgeons’ records. Fig. 24.1 Disk degeneration arising above solid anterior cervical diskectomy and fusion. Fogel and McDonnell15 retrospectively reviewed 31 patients who had dysphagia status post-ACDF, and who underwent plate removal and lysis of adhesions. The patients averaged three levels fused and were followed using the Bazaz-Yoo dysphagia scale. Preoperatively, 15 patients had moderate and 16 patients had severe dysphagia. At the time of the revision surgery, most patients exhibited extensive adhesions between the trachea and esophagus and the prevertebral fascia and the plate. Postoperatively, 55% of patients had no dysphagia, 32% mild, 10% moderate, and only 3% severe (Fig. 24.2). Riley et al16 reviewed data on 454 patients involved in the CSRS plating study. They found 30% of patients had dysphagia at 3 months, persisting at 24 months in 21% of patients. The number of levels fused increased the risk of dysphagia, with 20% of single-level fusion patients reporting dysphagia versus 39% having three or more levels fused. Smith-Hammond et al17 analyzed prospectively the incidence of and risk factors for developing dysphagia; 83 patients, 38 of whom underwent ACDF were followed for 3 years, by the dysphagia disability index and by video-fluoroscopic swallowing evaluation. Forty-seven percent of ACDF patients developed dysphagia. Of the risk factors assessed, surgical level, instrumentation, operative time, and myelopathy were not found to be significant. Only an age greater than 60 years was clinically significant. Although there is some evidence that use of instrumentation with ACDF may increase the risk of dysphagia, the problem will require more research. This decade has seen the development of the cervical disk replacement in an attempt to overcome some of the shortcomings of ACDF. Cummins, in the late 1980s, developed a metal-on-metal ball and socket device, fixed to the adjacent vertebrae by screws placed through an anterior flange.18,19 The device has undergone many design changes, including conversion to a ball and trough articulation, addition of another screw through each flange, and development of a locking device for the screws. This prosthesis has undergone a U.S. Food and Drug Administration (FDA) Investigational Device Exemption (IDE) study and is now marketed as Prestige ST Cervical Disc System (Medtronic Sofamor Danek, Memphis, TN) (Fig. 24.3). The BRYAN® Cervical Disc System (Medtronic Sofamor Danek, Memphis, TN) consists of a polyurethane nucleus attached to two convex titanium alloy shells that have a titanium porous coating, allowing bony ingrowth. A polyurethane sheath surrounds the nucleus, attaching to the titanium shells. The BRYAN Cervical Disc System has also completed its U.S. IDE evaluation20(Fig. 24.4). Thierry Marnay, MD, of France adapted his lumbar prosthesis into a cervical design, ProDisc-C (Synthes, Paoli, PA). Pro-Disc-C is a ball-and-socket design with a convex ultra-high-molecular-weight-polyethylene inlay attached to an inferior cobalt chrome alloy end plate, articulating with a polished socket integral to the superior cobalt chrome end plate. The end plates have keels for immediate fixation and a titanium plasma spray backing for bony ingrowth.21,22 ProDisc-C has also completed its IDE study (Fig. 24.5). Fig. 24.2 Example of adhesions between trachea, esophagus, and plate, status post–anterior cervical diskectomy and fusion. (From Fogel GR, McDonnell MF. Surgical treatment of dysphagia after anterior cervical interbody fusion. Spine J 2005;5:140–144.) Fig. 24.3 (A) Prestige ST Cervical Disc replacement. (B) Lateral radiograph of implanted Prestige ST Cervical Disc pros-thesis. (Courtesy of Medtronic Sofamor Danek, Memphis, TN) The Porous Coated Motion (PCM) Artificial Cervical Disc (Cervitech, Rockaway, NJ) originally developed by Paul C. McAfee, MD, features cobalt-chrome alloy end plates with a large radius ultra-high-molecular-weight polyethylene bearing surface attached to the caudal end plate, allowing translational motion. The end plates have a titanium porous coating with an additional calcium phosphate layer. The PCM replacement has a press-fit insertion. The PCM IDE study is nearing completion; the implant has significant international experience23 (Fig. 24.6). A plethora of other cervical disk prostheses are in design and evaluation phases, but the foregoing replacements have undergone the majority of clinical and biomechanical testing. Fig. 24.4 (A) BRyAN Cervical Disc replacement. (B) Anteroposterior view of implanted BRyAN Cervical Disc Prosthesis. (C) Lateral flexion view of implanted BRyAN Cervical Disc replacement. ([A] Courtesy of Medtronic Sofamor Danek, Memphis, TN) Several studies have shown the safety and efficacy of cervical disk replacement.20–27 However, the advantages of cervical disk replacement over ACDF are unproven in these studies. Questions to be answered in the paper concerning cervical disk replacement include the following: (1) Is cervical disk replacement clinically superior to ACDF, including diminishing adjacent segment disease? (2) Does cervical disk replacement decrease the risk of dysphagia? Fig. 24.5 ProDisc-C Cervical Disc replacement. (Courtesy of Synthes– North America, West Chester, PA) Fig. 24.6 PCM Artificial Cervical Disc replacement (Cervitech, Rockaway, NJ). (Courtesy of Paul C. McAfee, MD) To address these issues, a systematic review of the literature was undertaken to assess the evidence. The search included Medline, Embase, and the Cochrane Controlled Trials Registry. A total of 173 articles was found on the subject. Several of the studies are level III case control studies, which demonstrate the safety of cervical disk replacement but were not used to argue for the efficacy of cervical disk replacement. Due to the recent FDA IDE studies, several articles reported these randomized clinical trials. Twelve articles compared cervical disk replacement with ACDF. Of these, there were seven level I studies, two of which use randomized, controlled trial data to assess specific clinical issues, two level II studies, and two level III studies. One level IV study, a biomechanical study, was included. The resulting level of evidence is summarized in Table 24.1. Table 24.1 Evidence Levels of Published Studies
Role of Cervical Disk Replacement: Does It Avoid the Shortcomings of a Fusion?
 Limitation of Anterior Cervical Diskectomy and Fusion
Limitation of Anterior Cervical Diskectomy and Fusion
Biomechanics
Clinical Disk Degeneration
Dysphagia
 Cervical Disk Replacement
Cervical Disk Replacement
Clinical Studies
Level | Number of studies | Study Type |
|---|---|---|
I | 7 | |
II | 3 | |
III | 2 | |
IV | 1 | Biomechanics study (1 study)40 |
Clinical Studies: Is Cervical Disk Replacement Superior to Anterior Cervical Diskectomy and Fusion?
Level I Data
The data of these studies originate from the FDA IDE studies. Although these studies were designed as noninferiority studies, the results are beginning to reveal the advantages of cervical disk replacement. Mummaneni et al28 reported on the Prestige ST prospective, randomized, multicenter IDE trial. Five hundred forty-one patients with single-level disease were enrolled, with 276 patients receiving the Prestige ST disk replacement and 265 patients treated with ACDF. Eighty percent of the investigational patients and 75% of the fusion patients were available for follow-up at 24 months. In the disk replacement patients, there were no revision surgical procedures compared with five (1.9%) in the fusion patients. Five disk replacement patients (1.8%) had to have their implants removed, compared with nine (3.4%) of the ACDF patients; this number was not statistically significant. There was a statistically significant (p = 0.0492) lower rate of surgery for adjacent segment disease, with three (1.1%) of disk replacement patients requiring surgery versus nine (3.4%) of the ACDF patients.
Clinically, the neck disability index (NDI), Short Form-36 (SF-36), and visual analogue scale (VAS) results were better in the disk replacement patients, but not to the level of significance. Neurological success, which required maintenance or improvement of the neurological condition postoperatively, was seen in 92.8% of disk replacement patients versus 84.3% of controls, which was statistically significant. The authors also investigated return-to-work and found that the arthroplasty patients were able to resume work in 45 days compared with 61 days for the ACDF patients. Lastly, overall success of the procedure, defined as NDI improvement ≥ 15 points, maintenance, or improvement of the neurological status and lack of implant-associated adverse events, was seen in 79.3% of disk replacement patients versus 67.8% of ACDF patients, a statistically superior result.
Heller et al29 published the results of the BRYAN Cervical Disc replacement (Medtronic, Memphis, TN) IDE study and found similar results to the Prestige ST IDE study. Four hundred sixty-three subjects were enrolled and randomized, with 242 receiving a one-level BRYAN Cervical Disc replacement and 221 receiving ACDF. The disk replacement patients had statistically greater NDI score improvements at all time intervals compared with the ACDF control patients (p = 0.025 at 24 months). VAS pain scores also improved in both groups, with the investigational group showing statistically significant (p = 0.009) improvement in the neck pain scores at 24 months. SF-36 and neurological success improved equally in both groups. As with the Prestige ST study, the disk replacement patients were able to return to work sooner (48 days vs 61 days, p = 0.015). Adverse events were more common in the ACDF group, but not statistically significant. Overall success was defined as an NDI improvement ≥ 15 points, maintenance or improvement of neurological status, no adverse events related to the index surgery, and no subsequent surgery. At 24 months, a higher number of disk replacement patients (82.6% vs 72.7%, p = 0.010) met the criteria for overall success.
Nabhan et al30 evaluated 49 patients who either underwent ProDisc-C Cervical Disc replacement or ACDF in a randomized, controlled series. The patients were followed for 1 year, clinically and by roentgen stereometric analysis (RSA). Both groups improved clinically with no statistical significance. By RSA, both groups lost some cervical segmental range of motion, with ACDF patients losing significantly more segmental motion.
Murrey et al31 reported the results from the ProDisc-C IDE study. Two hundred nine total patients were enrolled, 103 who received the disk replacement and 106 who underwent ACDF. Both groups clinically showed similarly improved NDI scores, SF-36 scores, VAS arm and neck pain scores, as well as neurological success. A significant difference existed in reoperation rates: 8.5% in the ACDF patients versus 1.8% in the disk replacement group (p = 0.033). The study also evaluated health-related quality of life scores, based on minimum clinically important differences, including NDI scores improved ≥ 20%, VAS arm/neck frequency scores improved ≥ 20%, absence of device failure, and absence of strong narcotic/muscle relaxant use. Seventy-three percent of the disk replacement patients met all health-related quality of life parameters, while only 60.5% of ACDF patients did (p = 0.0472).
Delamarter et al32 evaluated the ProDisc-C IDE patients and an additional 136 patients treated with ProDisc-C in the continued access phase of the study, with a minimum 4 years follow-up. Several parameters showed significant improvement in the investigation group, including NDI scores (17.10 in ProDisc-C vs 28.00 in ACDF) and VAS satisfaction (91.10 ProDisc-C vs 79.99 ACDF). Device success was seen in 98.8% of ProDisc-C patients compared with 88.7% of ACDF patients (Fig. 24.7).
Other studies have concentrated on specific clinical entities where cervical disk replacement may offer advantages over ACDF.
Anderson et al33 used the BRYAN Cervical Disc replacement IDE study data to compare the rate of adverse events between the ACDF and disk replacement groups. The severity of the adverse events was graded using the World Health Organization (WHO) scale. The WHO scale is a four-point scale, ranging from grade 1 events, which require no treatment and do not affect outcome, to grade 4, which require an operation, are life threatening, or cause death or permanent disability. Grade 3 or grade 4 adverse events are classified as “serious,” whereas grade 1 or grade 2 is classified as “nonserious.” Adverse neurological events, grade 3 or 4, occurred with the same frequency in the Bryan (1.6%) versus ACDF (1.8%) group. However, other serious adverse events were more frequent in the ACDF group (36.2%) versus the Bryan group (30.2%), (p = 0.012), primarily due to the ACDF group having more reoperations for persistent symptoms and pseudarthrosis.
Riew et al34 has challenged traditional thought that patients with myelopathy secondary to cervical disease have to be treated with ACDF. The study evaluated a subset of patients with myelopathy, defined as being hyperflexic, having clonus, or having a Nurick grade ≥ 1, that were enrolled in the BRYAN or Prestige IDE studies. Because the IDE study required that pathology should be confined to one level, patients with multilevel disease and retrovertebral pathology such as ossification of the posterior longitudinal ligament were excluded. Of the 465 patients enrolled in the BRYAN Cervical Disc replacement trial, 93 were myelopathic; of these, 49 had disk replacement surgery. Five hundred forty-two patients were in the Prestige ST IDE trial, 106 myelopathic patients; 58 were randomized to disk replacement. In both studies, all patients who underwent cervical disk replacement demonstrated improvement or maintenance of their neurological status; one ACDF patient had neurological deterioration. There were no statistical differences in the clinical outcome in either the disk replacement or ACDF group. The results suggest that for myelopathy secondary to disk herniation, without retrovertebral or multilevel pathology, cervical disk replacement may be a suitable alternative to ACDF.
Fig. 24.7 (A) Anteroposterior view of implanted ProDisc-C (Synthes West Chester, PA) at C6–C7, 6 years postoperatively, demonstrating no adjacent segment disease. (B) Lateral view of implanted ProDisc-C at C6–C7, 6 years postoperatively, demonstrating no adjacent segment disease.
Level II Data
Goffin et al35 evaluated 74 patients who underwent a BRYAN Cervical Disc replacement, with 4- to 6-year follow-up. These patients are part of a multicenter, prospective, nonrandomized European study. Seventy-eight patients (69 single-level and nine two-level) had at least 4-year follow-up, whereas 10 single-level patients had 6-year follow-up. Of the patients with 4-year follow-up, 29 had no disk degeneration at baseline. At the 4-year radiographic evaluation, only three of the 29 patients (10.3%) had developed adjacent-level degeneration; at 6-year follow-up, four patients had no index adjacent-level disease, and none developed de novo degeneration. Of the two-level implants, seven of the eight with no index adjacent-level degeneration remained without degeneration at 4-year follow-up. Of the 41 single-level patients with baseline adjacent segment degeneration, 19 had no further disk degeneration, whereas 21 progressed radiographically at 4 years. Of the six single-level patients with 6-year follow-up and prior adjacent segment disease, all progressed radiographically. The disk replacement patients may have a lower radiographic rate of adjacent segment degeneration progression compared with prior ACDF studies. These patients also maintain their clinical improvement. Fifty-nine percent of the patients had excellent, 29% good, 8% fair, and 4% poor clinical results by Odom’s criteria at 4 years.
Phillips et al36 studied the efficacy of disk replacement implanted adjacent to prior cervical fusion. As part of the PCM cervical disk replacement IDE study, 126 patients received a primary PCM disk replacement, and 26 patients had the disk replacement adjacent to a prior fusion. Clinical results were similar in both groups. Two patients in each group had to undergo revision surgery. Although the numbers are small, disk replacement appears feasible adjacent to fusion.
Kim et al37 compared radiographic changes in a cohort of patients undergoing single-level and two-level Bryan disk replacement with patients undergoing single-level and two-level ACDF. Fifty-one patients underwent Bryan disk replacement (39 single-level and 12 two-level), and 54 patients underwent ACDF (26 single-level, 28 two-level). The average follow-up was 20 months. Clinically, by NDI and VAS scores, all groups improved without statistical significance. Radio-graphically, 40.74% of single-level ACDF patients developed adjacent segment disease, whereas only 17.6% of the single-level Bryan disk patients did. At two-levels, the ACDF patients again had higher rates of adjacent segment disease (57% vs 33%). Disk replacement appears to affect adjacent segment disease, although the numbers are too small and the length of follow-up too short to declare this result definitively.
Level III Data
Pimenta et al38 compared 71 single-level PCM cervical disk replacement patients with 69 patients who had multilevel (two to four levels) PCM disk replacements. By self-assessment measures, the multilevel disk replacement patients showed better improvement compared with the single-level patients. The mean NDI improvement was 52.6% for multilevel patients versus 37.6% for single-level patients (p = 0.021). VAS scores showed a similar trend, with mean improvement of 65.9% for the multilevel patients versus 58.4% for the single-level patients. Baseline scores for the NDI and VAS in both groups were almost identical. Reoperation rates were also similar, with three single-level and two multilevel patients requiring either revision of the prosthesis or removal and arthrodesis. Multilevel disk replacement is a viable option for multilevel disease confined to the disk space (Fig. 24.8).
Summary of Data
Several level 1 clinical studies demonstrate the safety and efficacy of cervical disk replacement. Mummaneni et al28 in the Prestige ST IDE study showed better clinical results in the disk replacement group, though they did not reach clinical significance. There was a statistically significant lower rate of surgery for adjacent segment disease, as well as a better rate of neurological success and overall success in the disk replacement patients. These patients were able to return to work sooner compared with the ACDF patients.
Heller et al29 in the BRYAN Cervical Disc replacement IDE study had improved clinical results, with NDI scores and VAS neck scores at 24 months statistically significantly improved. There were similar improvements in return to work and overall success in the disk replacement patients.
Murrey et al31 reported on the ProDisc-C IDE study showed excellent clinical results in both the disk replacement patients and the fusion controls. There was a much lower reoperation rate in the disk replacement patients and statistically significant improvement in the health-related quality of life scores.
Delamarter et al32 evaluated the ProDisc-C IDE patients as well as the continued access patients with 4-year follow-up. The ProDisc-C patients had significant improvement in NDI scores, VAS satisfaction, and device success.
There are two other level 1 studies, both of which used the IDE data to examine specific questions. Anderson et al33 used BRYAN study data to evaluate WHO adverse events. There were no differences in the “serious” or grade 3 or 4 neurological events, but other grade 3 or 4 events were higher in the ACDF group, primarily for reoperations for persistent symptoms or pseudarthrosis. Riew et al34 evaluated patients with myelopathy using data from Prestige ST and BRYAN Cervical Disc replacement IDE studies, and found that in myelopathic patients with pathology confined to the disk space, disk replacement yields equal outcomes to ACDF.
Goffin et al35 in the prospective, multicenter European BRYAN Cervical Disc replacement trial reported the longest follow-up published on cervical disk replacement. At both the 4- and 6-year follow-up points, the clinical results of both single- and two-level implants were maintained. Phillips et al,36 as part of the PCM Cervical Disc replacement cohort, found that the patients who had a disk replacement adjacent to a prior fusion had similar results compared with patients who had a primary disk replacement. Pimenta et al38 found that multilevel PCM disk replacements performed as well or better than single-level disk replacements. The data are summarized in Table 24.2.
Fig. 24.8 (A) Anteroposterior view of two-level PCM disk replacement (Cervitech, Rockaway, NJ). (B) Lateral view of two-level PCM disk replacement.
Pearls
• Level I and II evidence suggests equivalent or superior clinical results with cervical disk replacement compared with ACDF.
• Level I evidence suggests lower reoperation rates and quicker return to work with cervical disk replacement versus ACDF patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree