Schizophrenia
HISTORIC PERSPECTIVE
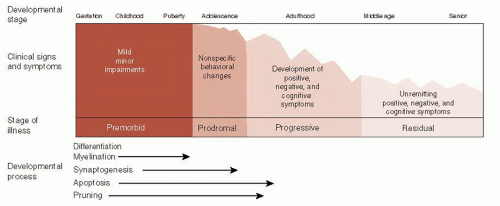
Over 100 years ago, Emil Kraepelin, a German psychiatrist, described the syndrome now called schizophrenia. Bleuler actually coined the term schizophrenia. Kraepelin called it dementia praecox. Kraepelin’s major contribution to psychiatry was recognizing that schizophrenia and manic depression are different disorders. The patient with schizophrenia has a persistent deteriorating course in mental functioning, whereas the patient with manic depression will experience periods of remission. Figure 23.1 shows a modern interpretation of the clinical course of schizophrenia.
Kraepelin was convinced that schizophrenia was an organic disease of the brain and spent considerable time and energy conducting postmortem studies on the brains of patients with schizophrenia. They had a good track record of identifying pathology, as one of his colleagues was the neuropathologist Alois Alzheimer. Unfortunately, Kraepelin was never able to discover a specific abnormality in the brains of schizophrenic patients. This pattern was to continue for a long time.
Numerous postmortem studies were conducted over the next 70 years comparing the brains of schizophrenic patients with healthy controls. Still no distinguishing pathology was isolated. The absence of gliosis in the tissue was of particular interest. Gliosis, sometimes called the glial scar, is considered the hallmark of neurodegenerative disorders and is found with such conditions as Huntington’s or Alzheimer’s diseases as well as with trauma and ischemia.
The absence of any significant neuropathology along with the burgeoning interest in psychoanalytic theory led to psychosocial explanations for schizophrenia. Terms such as the refrigerator mother and the double-bind were developed to explain the psychological turmoil that caused schizophrenia. Some clinicians even speculated
that patients voluntarily chose to be psychotic to avoid conflict in their lives.
that patients voluntarily chose to be psychotic to avoid conflict in their lives.
Although the development of chlorpromazine (Thorazine) in the early 1950s dramatically changed the treatment of schizophrenia, the identification of biologic abnormalities remained elusive. In 1972, Plum summarized the frustration when he called schizophrenia the graveyard of neuropathologists. Schizophrenia was actually dropped from the preeminent neuropathology textbook (Greenfield’s Neuropathology) for the next two editions and only added back in 1997. It was the emergence of significant findings on brain imaging studies that finally ended the debate about whether there are quantifiable (measurable) changes in the brain (more on this in the next section).
Although we follow convention and use the term “schizophrenia,” many researchers are struck by the variations between patients. For example, some patients have no hallucinations and mostly struggle with negative symptoms, while other patients have chronic hallucinations and few negative symptoms. To remind readers of this heterogeneity, some use the term “the schizophrenias.” In this book we will use the standard term schizophrenia.
MODERN EPIDEMIC?
E. Fuller Torrey calls schizophrenia an invisible plague. He believes that schizophrenia is a modern illness that has increased so gradually that the change is not perceptible during any single person’s lifetime. Additionally, the changes in diagnostic criteria that occur over the decades make comparisons between generations difficult. In spite of these difficulties, there is evidence to support Dr. Torrey’s belief.
The ancient Greeks and Romans were astute observers of human behavior. Reviews of the writings from ancient times provide the following descriptions of conditions that we easily recognize:
Epilepsy
Migraine headache
Melancholia
Anxiety
Chronic alcoholism
Delirium
The ancient writers did describe psychotic symptoms including hallucinations and delusions. However, in almost every case the psychosis cleared. There are no reports that describe an initial psychotic break in late adolescence or early adulthood with a chronic unremitting course. The absence of a condition that looks like schizophrenia stands in contrast to the good clinical descriptions of other neuropsychiatric syndromes. This softly suggests that the illness was not present in ancient Greece or Rome.
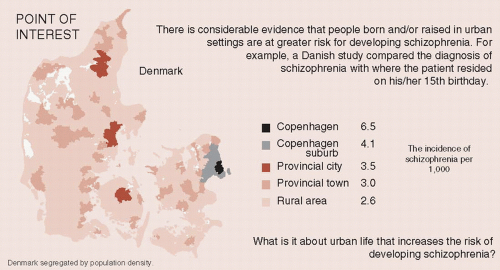
The 19th and 20th centuries saw an explosion in the institutionalization of patients with chronic mental illness. Many of these patients had schizophrenia. Figure 23.2 shows the growth in institutionalized patients as a percentage of the total population in four countries. There are many reasons for confining the seriously mentally ill: industrial revolution, changes in social norms, lack of effective treatments, and so on. An additional explanation is the emergence of a psychiatric epidemic.
Although we may never know for sure whether schizophrenia is a modern epidemic or has been around for ages, the topic raises the issue of etiology. What causes schizophrenia? We will start with what is known about the brain of patients with schizophrenia.
GRAY MATTER
The development of brain imaging techniques provided a way to examine schizophrenic brains in live people. The first computed tomography scans in schizophrenia were published in 1976 and showed enlarged lateral ventricles in a group of patients with chronic schizophrenia. Others quickly replicated this study. However, it was magnetic resonance imaging (MRI), with its ability to differentiate gray and white matter, that finally provided irrefutable evidence of the biologic nature of schizophrenia.
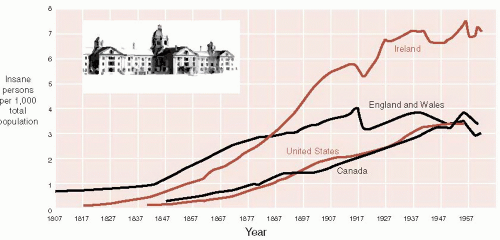
The most famous MRI studies were the original studies on twins. E. Fuller Torrey and Daniel Weinberger et al. at the National Institute of Mental Health recruited monozygotic twins from the United States and Canada. They originally studied 15 sets of twins who were discordant for schizophrenia: one had the illness, whereas the other was unaffected. MRI was done in all 30 participants. The most remarkable finding was that in 12 of the 15 sets of twins the affected individual was easily identified by visual inspection of corresponding coronal scans (Figure 23.3).
The results of the twin study have been replicated and extended. The most common finding remains enlarged ventricles, but better technology has allowed more detailed analysis. Patients with schizophrenia show consistent but subtle decreases
in total brain volume and total gray matter volume. These results provide an explanation for the increased ventricle size; that is, the ventricles expand to fill the void left by the loss of gray matter.
in total brain volume and total gray matter volume. These results provide an explanation for the increased ventricle size; that is, the ventricles expand to fill the void left by the loss of gray matter.
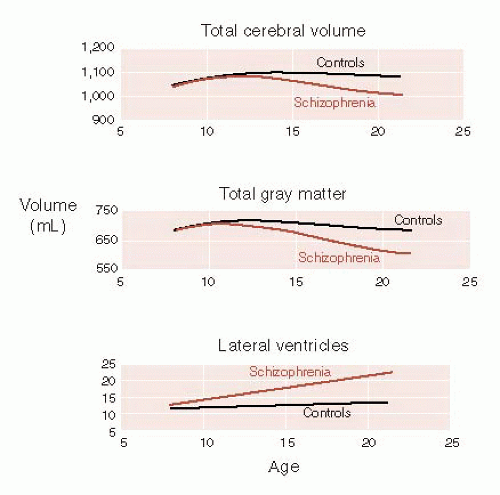
Judith Rapoport’s laboratory performed sequential MRI scans on children with childhood-onset schizophrenia and compared the findings with age-matched controls in an effort to follow up the changes in the brain that occur during adolescence. They found that the rate of change was greater for those children with schizophrenia. Figure 23.4 shows that the children with schizophrenia had striking loss of gray matter along with decreased brain size and increased ventricles.
Adolescence is a time of remodeling of the connections in the brain to create a more efficient organ. Processes such as pruning, apoptosis, and synaptogenesis are accepted features of the maturing brain (see Figures 8.8, 19.4, and 20.8). Studies such as the one described here suggest that schizophrenia may be the result of overly exuberant remodeling of the gray matter.
Certainly, the process of gray matter reduction occurs in the same time frame as the usual onset of schizophrenic symptoms. Although no definitive evidence exists to prove this theory, some genetic studies suggest that altered expression of genes that control synaptic plasticity contributes to the development of schizophrenia.
Reduced Neuropil Hypothesis
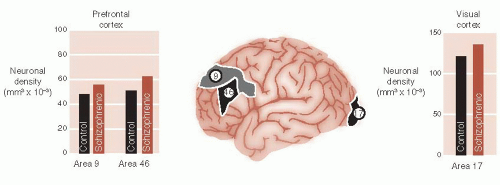
As stated before, traditional microscopic examination of the gray matter of schizophrenics will not identify anything unusual. So it has been difficult to explain the gray matter loss. Investigators at Yale utilized labor-intensive three-dimensional analytic tools to estimate cellular densities. They compared neuronal density in three regions of the brain from patients with schizophrenia and from healthy controls. The regions were Brodmann’s areas 9 and 46 in the prefrontal cortex (PFC) and area 17 in the visual cortex. They found increased density of neurons but not glial cells in the gray matter of schizophrenic patients (Figure 23.5).
It appears that schizophrenic patients have the same number of neurons as healthy controls, but they are packed together in less space—called the reduced neuropil hypothesis. The tighter packaging of the schizophrenic neurons results from reduced cell
size, less branching, and decreased spine formation. Figure 23.6 shows a drawing of this process. Figure 23.7 shows examples of actual spine formation from schizophrenic patients and controls. The key point is that it is not neuronal loss, but rather the loss of the richness of the dendritic connections that causes the reduced gray matter in schizophrenia. Presumably, this also results in deficient information processing.
size, less branching, and decreased spine formation. Figure 23.6 shows a drawing of this process. Figure 23.7 shows examples of actual spine formation from schizophrenic patients and controls. The key point is that it is not neuronal loss, but rather the loss of the richness of the dendritic connections that causes the reduced gray matter in schizophrenia. Presumably, this also results in deficient information processing.
Although the underlying cause of neuronal atrophy remains unknown, recent evidence suggests a role for altered neuronal apoptosis. Apoptosis is usually associated with programmed cell death (see Figure 8.9). However, sublethal apoptotic activity may result in synaptic elimination without frank cell death. Apoptosis is controlled by pro- and antiapoptotic proteins, which may be disturbed in schizophrenia.
One further point worth mentioning is that these studies highlight the extensive whole brain involvement of schizophrenia. That is, it is not a disorder of just one region of the brain. Rather, schizophrenia seems to affect almost the entire cortex.
Functional Brain Imaging
Traditionally, the hallmark of schizophrenia has been hallucinations and delusions. In actuality, the symptoms of schizophrenia are made up of the following three categories of impairment.
Positive symptoms: hallucinations and delusions
Negative symptoms: lack of motivation, apathy, and so on
Cognitive impairment
The cognitive dysfunction, which includes problems with attention, memory, and executive function, may be the most detrimental aspect of the illness. They have a greater negative impact on the individual than the positive symptoms. Likewise, cognitive functioning is the best predictor of longterm outcome from the disorder.
The pattern of cognitive impairment in schizophrenia implicates the frontal cortex. Hypofrontality is a term sometimes used to describe this problem. However, functional imaging studies have given inconsistent results. Weinberger et al. recognized that the function of the frontal lobe must be measured when it is engaged in a cognitive challenge.
To test this theory, patients and healthy controls underwent xenon XE 133 inhalation procedure for regional cerebral blood flow measurements while they were performing the Wisconsin Card Sorting test (Figure 23.8). The control subjects showed increased activation of their frontal lobes while performing the test, but the schizophrenic patients did not. Furthermore, there was a good correlation between the change in blood flow in the frontal cortex and percent errors on the test.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree