CHAPTER 18 SCHIZOPHRENIA AND SCHIZOPHRENIA-LIKE PSYCHOSIS
The first part of this chapter deals with schizophrenia as a primary illness, and the second describes schizophrenia-like features that appear in the context of other neurological illness.
SCHIZOPHRENIA
Schizophrenia is a brain disease as common as multiple sclerosis that impairs the ability to work, independent living, and interpersonal relationships. The effect of schizophrenia on health care budgets is substantial and accounts for 1.5% to 3% of total national health care expenditure.1
Kraeplin2 introduced the term dementia praecox to refer to a cluster of symptoms that included catatonia and paranoia and carried a poor prognosis. The term schizophrenia was first used by Bleuler,3 who believed that certain “fundamental symptoms” were present in all affected patients. Current diagnostic classifications, such as the International Classification of Mental and Behavioural Disorders, 10th revision (ICD-10)4 and the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV),5 still require the presence of a cluster of symptoms, in the absence of drug abuse or other organic brain disease, to establish the diagnosis (Table 18-1).
TABLE 18-1 Key Symptoms of Schizophrenia with Exclusion Criteria
Rights were not granted to include this table in electronic media. Please refer to the printed book.
Epidemiology
The incidence of schizophrenia is rather similar across different countries, with rates between 0.16 to 0.42 per 1000 and with a prevalence around 1% when narrow diagnostic criteria are used.6 There are some remote populations with an increased incidence and prevalence, such as the Afro-Caribbean population in the United Kingdom (incidence ratios above 7),7 and others with reduced rates, such as the Hutterites of South Dakota (ratio of observed to predicted mean rates, 0.48),8 and genetic and environmental factors probably contribute to this variability. Schizophrenia is common in men and women equally, and its onset may occur at any age, although it often starts between the ages of 15 and 45, with an earlier onset in men.9
Clinical Features and Natural History
Schizophrenia is characterized by a multitude of symptoms that vary between patients and encompass a variety of mental functions such as perception, emotion, and language (see Table 18-1). The symptoms of schizophrenia are often categorized as positive and negative. Positive symptoms include delusions, passivity phenomena, and hallucinations. Negative symptoms include apathy and social withdrawal. Functional imaging studies (positron emission tomography) have suggested that auditory hallucinations are accompanied by increased blood flow10 in subcortical nuclei, limbic structures, and paralimbic regions, and functional magnetic resonance imaging (MRI) demonstrates increased activation in the inferior frontal and temporal cortex.11 The neural correlates of other symptoms are less well understood.
Psychotic symptoms usually start in late adolescence or early adulthood,12 tend to persist throughout the illness,13 and are often associated with poor psychosocial functioning.14
For many patients, schizophrenia starts with a prodromal period lasting from months to years. The symptoms of the prodromal stage may include depression, anxiety, dysphoria, social withdrawal, and cognitive underfunctioning, as well as attenuated psychotic symptoms.15
The outcome of schizophrenia is variable. Harrison and Eastwood16 found that one third of patients had recovered at follow-up 15 or 25 years later and that for many patients, schizophrenia is a relapsing-remitting disorder. The study also showed that lack of improvement early in the illness is predictive of persistence of symptoms and long-term disability. Other studies have revealed that an early onset of psychosis is associated with a more severe illness, irrespective of duration of illness.17
Cognitive Deficits
Cognitive impairment is an integral feature of schizophrenia. Attention, executive function, and memory are most commonly impaired.18 Cognitive deficits are already present at the onset of psychosis19,20 and are present irrespective of medication.21 Some patients appear to undergo a decline in general intellectual function in the prodromal stages of the illness or during the onset of psychosis.22,23 After the onset of psychosis, cognitive impairments do not generally deteriorate further, which suggests that they are independent of clinical symptoms and the effects of medication.24 Large-scale studies have found that schizophrenic patients perform worse than healthy controls across a range of cognitive tasks,25,26 that cognitive impairment in a given function is predictive of impairment in all others,27 and that this impairment is global, variation between patients being a matter of degree. Other studies have found evidence for a subgroup of patients with isolated executive dysfunction.22,28 Deficits in executive function may be related to an increased genetic susceptibility to schizophrenia29 and may be part of the schizophrenia endophenotype.30 Similarly episodic memory deficits may be associated with an earlier age at onset,29 and this may suggest that early brain insults (e.g., hypoxia) that constitute a risk factor for young age at onset may, through their action on the amygdala and hippocampus, may also be responsible for the memory deficits.
Functional imaging studies have shown reduced blood flow (positron emission tomography31,32) and reduced activation (functional MRI33) in the dorsolateral and other prefrontal areas of the cortex in schizophrenic patients in comparison with normal controls in response to executive function tasks. The neural correlates of other cognitive deficits are less well understood.
The effect of typical neuroleptics on cognition is still controversial, although the blockade of dopamine D2 receptors achieved by these drugs may have a negative effect on cognition.34 In contrast, atypical neuroleptics, with antipsychotic effects not mediated by D2 blockade, may preserve or enhance cognition.35
Genetics
Twin studies in schizophrenia have shown concordance rates of 41% to 65% in monozygotic pairs and 0% to 28% in dizygotic pairs and a heritability rate of 80% of 85%,36 which are suggestive of an important genetic contribution. The genetic risk for an individual increases with the degree of relation to the affected relative: 40.8% if there is an affected monozygotic twin, 5.3% in siblings of affected patients,37 and a lifetime risk ranging from 3.1% to 16.9% in first-degree relatives of schizophrenic probands.38 A younger age at onset is associated with a higher familial risk for schizophrenia.39
Of the susceptibility genes possibly associated with schizophrenia, catechol-O-methyl-transferase (COMT) is the most likely. COMT is predominantly expressed in prefrontal and hippocampal neurons and implicated in interneuronal monoaminergic signaling, especially dopamine. Hemideletion of chromosome 22q11, where COMT maps, results in the velocardiofacial syndrome40 with a greatly increased risk (24% in a study sample of patients with velocardiofacial syndrome) of schizophrenia-like psychosis.41
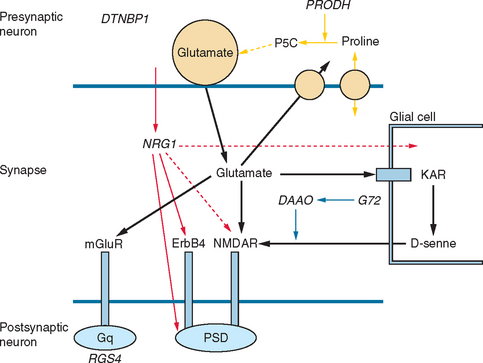
Other possible susceptibility genes, suggested by association studies, are DISC1 (“disrupted in schizophrenia”), a complex gene with effects on cytoskeletal proteins, cell migration, and membrane trafficking of receptors likely to influence hippocampal structure and function42; neuregulin 1 (NRG1) with effects in signaling and hence in neuronal development and plasticity; dysbindin (DTNBP1), widely expressed in neurons, including those in the dorsolateral prefrontal cortex, hippocampus, and substantia nigra, with effects on trafficking and tethering of receptors N-methyl-d-aspartate [NMDA], nicotinic acid, and γ-amino butyric acid A [GABAA]), and likely to contribute to glutamatergic hippocampal pathology; the regulator of G protein signaling 4, expressed in the dorsolateral prefrontal cortex involved in signaling; and the metabotropic glutamate receptor gene (GRM3), expressed presynaptically in neurons, astrocytes, and oligodendrocytes and likely to affect glutamatergic neurotransmission in the hippocampus and prefrontal cortex. Other genes associated with glutamatergic transmission and implicated in schizophrenia include G72 and d-amino acid oxidase (DAAO), which appear to directly affect NMDA receptors, and proline dehydrogenase (PRODH), which affects glutamatergic synapses by several mechanisms (Fig. 18-1).43,44
Most of the susceptibility genes so far identified have an effect on the molecular biology of the synapse, particularly glutamatergic synapses, but also influence the dopaminergic and GABAergic systems, thus causing malfunction of cortical microcircuits, which probably explains the pattern of symptoms and cognitive deficits that characterize schizophrenia.44
Neuropathology
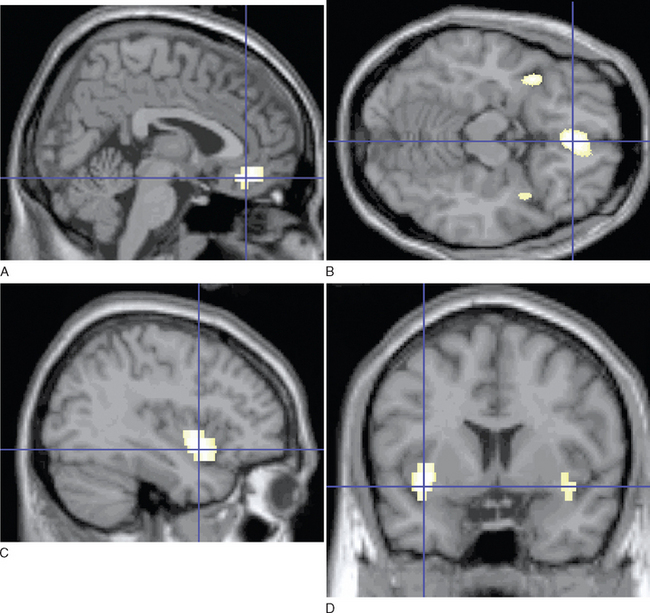
Imaging studies have demonstrated loss of brain volume in schizophrenic patients in comparison with controls45,46 and have highlighted pathological changes in the hippocampus and prefrontal cortext47 and in the superior temporal cortex and thalamus.46 More recent studies with magnetization transfer imaging, a technique sensitive to subtle neuropathological changes (e.g., changes in cell membranes and myelin) have demonstrated diffuse cortical abnormalities in patients with chronic schizophrenia.48 In patients with first episodes,49 these abnormalities are limited to the medial prefrontal cortex, insula, and fasciculus uncinatus in the absence of atrophy. Imaging abnormalities are already evident before or at the time of the first episode of illness (Fig. 18-2)50 and may be present in unaffected relatives,51 which suggests that these abnormalities may be related to the genetic predisposition or early environmental factors, rather than to the illness itself. These changes, modest and often nonspecific, are not diagnostic of schizophrenia and may be present in other psychoses.
The most consistent histological findings are decreases in neuronal size in the hippocampus and neocortex with reduced dendritic arborization and synaptic abnormalities.52 Levels of N-acetyl aspartate, a marker of neuronal integrity, measured in vivo with magnetic resonance spectroscopy, are reduced in the hippocampus53 and prefrontal cortex,54 which is in keeping with these findings. Neuronal loss in the dorsomedial nucleus of the thalamus and pulvinar have been less consistently reported.55 Reduction in the number of oligodendrocytes, important in myelination and synaptic integrity, whether primary or secondary to these neuronal changes, have also been reported.56 These quantitative alterations of the normal neural circuitry may result in subtle loss of cortical volume and thickness.16
Longitudinal imaging studies have not provided clear evidence of progression of brain abnormalities (see Shenton et al [2001]46 for a review), although loss of cortical volume may occur in the early stages of the illness in subgroups of patients with early onset and severe symptoms.57 Other investigators, using diffusion tensor imaging, have described axonal and myelin abnormalities in the corpus callosum of patients with chronic schizophrenia,58 which are absent at the onset of schizophrenia.59 Neuropathologically, astrogliosis and neurodegenerative changes, including those of Alzheimer’s disease, are not overrepresented in schizophrenia, which suggests that apparent clinical deterioration may be difficult to explain as a result of a neurodegenerative process.60–62 In contrast, abnormalities of neuronal migration, evidenced by aberrantly located neurons in the lamina II of the entorhinal cortex and neocortical white matter, are strongly suggestive of disruption of normal brain development (for a review, see Harrison [1999]63).
Further evidence for schizophrenia as a disorder of normal brain development is found in epidemiological studies that suggest early environmental factors that increase the risk for schizophrenia in later life. Evidence points toward a small winter-spring excess of births among patients with schizophrenia,64 as well as exposure to the influenza virus prenatally.65,66 Obstetrical complications are also linked to this risk, although the mechanisms are uncertain.67
Neurochemistry
The dopamine hypothesis has been the chief neurochemical hypothesis in schizophrenia since the early 1960s68 and is supported by observations that dopamine D2 receptor blocking is common to all antipsychotic drugs.69 The mechanism and exact location of dopaminergic abnormalities in schizophrenia still remain unclear, and the dopamine hypothesis has undergone some revision since its initial inception. According to the hypothesis as it stands now, there exists a dopaminergic imbalance between the hyperactive subcortical, mesolimbic dopamine pathways (resulting in positive symptoms), and the hypoactive mesocortical dopaminergic connections to the prefrontal cortex (resulting in negative symptoms and cognitive impairment).70 The alternative glutamate hypothesis is based on the observation that the NMDA glutamate receptor antagonist phencyclidine causes psychosis that resembles both the positive and negative symptoms of schizophrenia.71 The glutamate hypothesis in its most simplified form is that a reduction in glutamate neurotransmission at the NMDA receptor results in symptoms of schizophrenia.72 However, the dopamine and glutamate hypotheses are not mutually exclusive, inasmuch as reciprocal synaptic relations between forebrain dopaminergic projections and glutamatergic systems have been described.73
There is also evidence of dysfunction of the GABAergic system in schizophrenia (see Benes and Berretta74): namely, the reduction of specific GABAergic interneurons (paralbumin-immunoreactive cells) in the prefrontal cortex and hippocampus.75 Various subtypes of GABA neurons provide both inhibitory and disinhibitory modulation of cortical and hippocampal circuits believed to be involved in schizophrenia. The evidence for the role of the serotonergic system in schizophrenia is unclear, although there are serotonergic hallucinogens that block 5-hydroxytryptamine 2 receptors,76 and 5-hydroxytryptamine 2A receptor antagonism may contribute to the efficacy of atypical neuroleptics.77
The Pathophysiology of Schizophrenia
One of the greatest challenges facing psychiatry today is to propose an explanatory theory that encompasses the often disparate facts known about schizophrenia and is able to accommodate emerging knowledge. There is evidence for a genetic predisposition, and a number of possible candidate genes with effects on the molecular biology of the synapse, as well as on the dopaminergic and GABAergic systems, have been identified.44 Histological findings such as aberrant neuronal clusters in the entorhinal cortex and an absence of gliosis also imply a neurodevelopmental etiology. Early environmental insults are additionally implicated, and these include complications of pregnancy and delivery.67 Abnormalities in cortical circuitry, induced by developmental and environmental factors, may limit neuronal information-processing capacity, and demands made on this malfunctioning system later in life may result in the emergence of psychotic symptoms and cognitive deterioration. The neurodevelopmental theory presupposes that pathological changes are not progressive and that changes in brain volume detected during the illness may be the consequence of disease-related changes in neuroplasticity (e.g., unstimulating environments, medication).78
Treatment of Schizophrenia
Drug Treatment
Neuroleptics have been used in the treatment of acute and chronic psychosis since the 1950s. The antipsychotic effect of the first-generation typical neuroleptics such as haloperidol and chlorpromazine depends on their action on the dopamine D2 receptors, and hallucinations are blocked when about 70% of the D2 receptors are occupied by neuroleptic drugs.79 Dopamine D3 and D4 receptor antagonism does not appear to be as important for antipsychotic effects.79 Antipsychotic agents may also affect brain structure directly: There are reports, albeit with a small sample size, of reversal of the superior temporal gyrus volume loss with neuroleptic treatment in a 1-year follow-up.80
Although typical antipsychotics have beneficial effects on positive symptoms, they are less effective in treating negative symptoms and cognitive impairment.81 They also have serious unwanted effects, such as extrapyramidal side effects (EPSEs), tardive dyskinesia, and neuroleptic malignant syndrome (NMS).
Clinical EPSEs include acute dystonia, subjective feelings of restlessness (akathisia), and parkinsonism. Positron emission tomographic studies suggest that EPSEs are related to dopamine D2 occupancy in the range of 75% to 80%,82 but D1 antagonism has also been implicated.83 Although traditional neuroleptics do not necessarily lead to EPSEs, the therapeutic window between therapeutic effect and EPSE is small, and thus many patients receiving these medications have EPSEs.
Tardive dyskinesia is a potentially irreversible side effect of long-term treatment with neuroleptic drugs and is characterized by abnormal involuntary hyperkinetic movements such as grimacing, lip smacking, tongue protrusion, and rapid eye blinking. Involuntary rapid movements of the fingers, arms, legs, and trunk may also occur. Various hypotheses, including overactivity in the striatal dopamine system,84 abnormal GABA-related striatal neurons,85 and free radical production73 have been proposed as pathophysiological mechanisms. Epidemiological data indicate that increasing age86 and female gender are risk factors for tardive dyskinesia.87 The outcome of tardive dyskinesia is more favorable in younger patients.87 Discontinuation of neuroleptic drugs or the use of a drug with fewer EPSEs (e.g., clozapine) is the first action of treatment.
NMS is a life-threatening syndrome characterized by fever, muscular rigidity, and raised serum creatine kinase concentration. The incidence has been estimated to be between 0.07 and 0.9,88,89 and onset can occur within hours but is usually 4 to 14 days after starting neuroleptic therapy. The mechanism of NMS is uncertain, but the most widely accepted mechanism is of blockage of dopamine receptors in the nigrostriatal tracts.90 An alternative hypothesis suggests an imbalance between serotonin and dopamine.91 Risk factors for developing NMS include dehydration, male gender, the presence of organic brain disease or mental retardation, and rapid escalation of ingestion of neuroleptic drugs.92,93 The mortality rate has been reported at 8%,94 but most patients recover within 14 days.93 In NMS, antipsychotics should be discontinued, and, in general, intensive care treatment is required. Drugs that have been used in the treatment of NMS include dopamine agonists such as bromocriptine and apomorphine. If restarting a neuroleptic is deemed necessary, it is worth switching to a neuroleptic in a different chemical class and with a lower D2 affinity than the drug that produced the NMS.95
Maintenance treatment with antipsychotic medication decreases relapse rates96; however, a substantial proportion of patients suffer relapse despite taking medication, and poor compliance is also a problem.
A second generation of so-called atypical neuroleptics (e.g., clozapine, risperidone, quetiapine, olanzapine) has been developed with a spectrum of receptor effects different from those of typical neuroleptics and less severe side effects, resulting in better compliance and improved therapeutic outcome.97
Clozapine is the prototype of this class of neuroleptic. Kane and colleagues98 established the antipsychotic efficacy of clozapine in previously treatment-resistant patients without side effects, and this has been confirmed in other studies.99,100 Clozapine also has an effect on negative symptoms and cognitive functioning.100 One of the properties of clozapine is its high dissociation constant at the D2 receptor, which results in fewer EPSEs.101 Clozapine also has affinities for other nondopamine receptors such as 5-hydroxytryptamine 2, and its α2-adrenoceptor antagonism is believed to contribute to the freedom from EPSEs (see Reynolds102 for review). Clozapine may cause potentially fatal agranulocytosis, and regular blood monitoring is required. Other unwanted effects include hypersalivation, weight gain, and a lowering of the seizure threshold. The increased risk of stroke in older adults with dementia has also been linked to atypical antipsychotics.103
Recent developments in understanding the mechanism of action of antipsychotic medications has led to the development of the partial D2 and 5-hydroxytryptamine 1A receptor agonist aripiprazole,104 which is antipsychotic and possibly without EPSEs.105 Future drug treatments may continue to focus on partial agonism to improve antipsychotic symptoms or focus on NMDA-glutamatergic modulators.106
In the United Kingdom, the guidelines of the National Institute of Clinical Excellence recommend the use of atypical neuroleptics as first-line treatment, because of fewer side effects and efficacy comparable with those of typical neuroleptics, and the use of clozapine in treatment-resistant patients. Early treatment is recommended because of the possible association between a longer duration of untreated psychosis and poor outcome.107
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree