Chapter 16 Sciatic Nerve
The Sciatic Nerve in the Pelvis
Anatomy
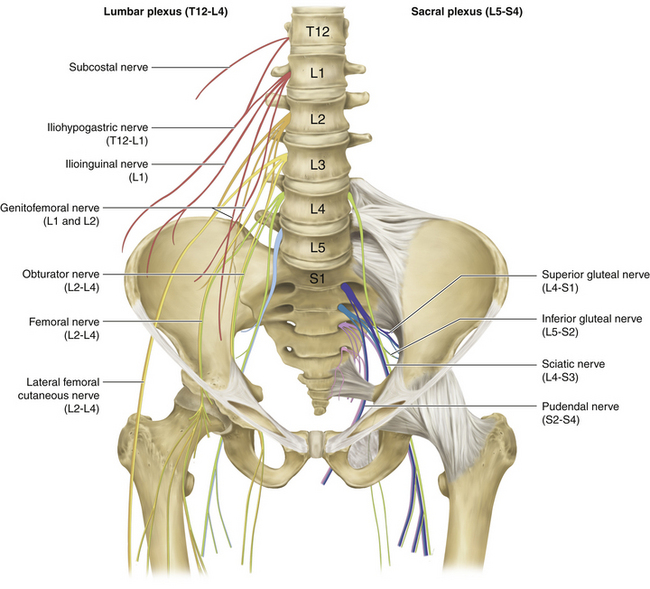
• The sciatic nerve takes its origin from the ventral divisions of the anterior primary rami of L4, L5, S1, S2, and S3. The lumbar contribution (L4 and L5) runs down anterior to the sacroiliac joint to join the sacral plexus (Figure 16-1). The sacral plexus lies behind the pelvic fascia and in front of the piriformis. Parasympathetic fibers are derived from S2, S3, and S4, close to their exit from the foramina.
• The main trunk of the sciatic nerve supplies the hamstring compartment and then separates into the tibial and common peroneal nerves, which are bound together by a common sheath of connective tissue. The sciatic nerve, formed by a confluence of the spinal nerves, escapes the pelvis by running through the greater sciatic foramen.
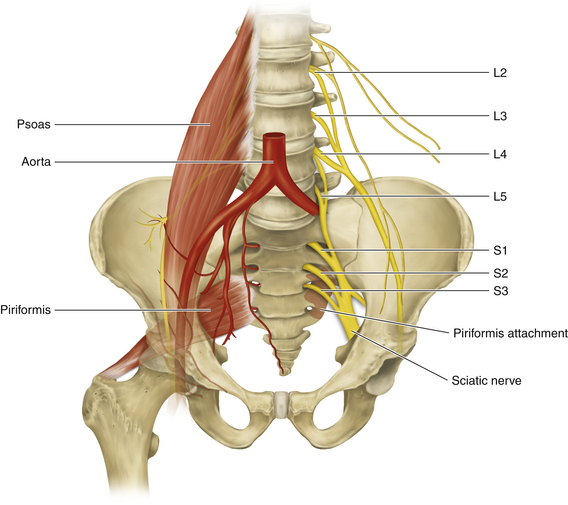
• The slips of origin of piriformis interdigitate with the anterior sacral foramina (Figure 16-2).The muscle exits the pelvis through the greater sciatic foramen, with the superior gluteal nerve and vessels above it and the remaining nerves and vessels below.
• The iliac vessels lie anterior to the pelvic fascia, and the ureter descends, anterior to the bifurcating vessels, in line with the sacroiliac joint.
• The sigmoid colon has a short mesentery, and the upper rectum is covered by peritoneum on its front and sides. Further distally, the rectum is covered only in the front by the peritoneal reflection.
• A significant venous plexus drains the bowel and other pelvic viscera.
Surgical Technique
• Operations on the pelvic plexus are especially difficult, and when nerve injury or a tumor is involved, they can be very challenging. Images should be carefully studied, so that the surgeon understands the exact position of the nerve tumor relative to the surrounding bony and soft tissue anatomy.
• The surgeon should have a thorough knowledge of each spinal nerve distribution, in case consideration has to be given to sacrificing a neural element during tumor resection.
• The true pelvis, when containing a nerve tumor, presents a very cramped operating arena. The nerve surgeon needs assistance from an individual experienced and skilled in protecting the ureter, vessels, and bowel. That individual will be used to define the correct planes of dissection to avoid or control significant venous plexus bleeding.
The Sciatic Nerve in the Buttock
Anatomy
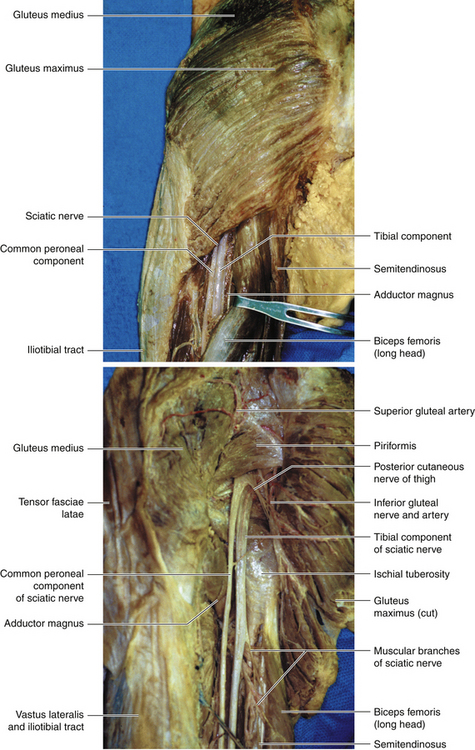
• The gluteus maximus (inferior gluteal nerve) has a dual insertion into the femur and, with the tensor fasciae latae (superior gluteal nerve), into the iliotibial tract. The superior border of the gluteus maximus is contiguous with the inferior border of the gluteus medius (superior gluteal nerve).
• The plane deep to the gluteus maximus is relatively avascular, and the entire muscle can be lifted to display the underlying anatomy.
• The piriformis originates from the front of the sacrum and is inserted into the femur. The points of insertion of both the piriformis and gluteus maximus into the femur should be clearly understood.
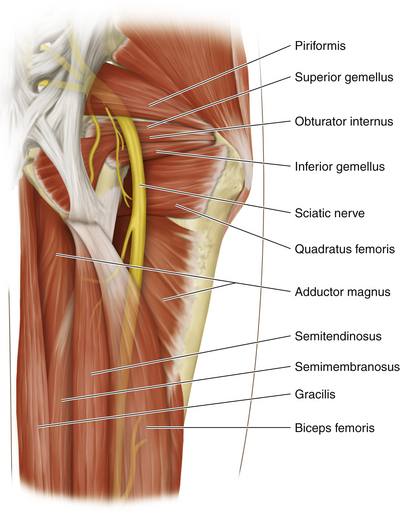
• The sciatic nerve enters the gluteal region through the greater sciatic foramen below the piriformis and comes to lie on the ischium (Figure 16-3). The nerve to quadratus femoris is deep to the sciatic nerve, and the posterior cutaneous nerve of the thigh lies superficial to the sciatic nerve. The sciatic nerve descends between the greater trochanter and the ischial tuberosity, crossing posterior to the obturator internus and the gemelli.
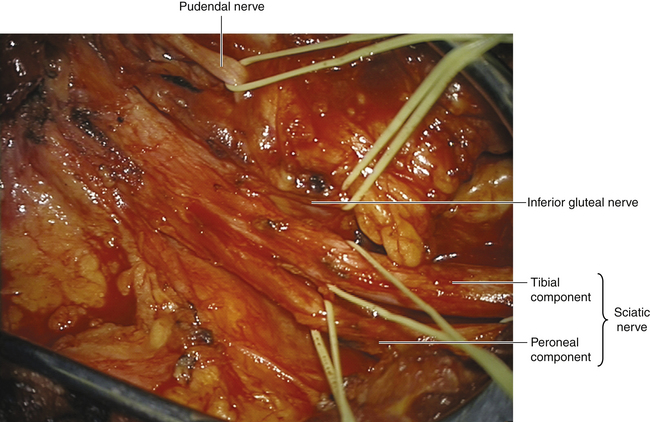
• The inferior gluteal nerve arises from L5, S1, and S2 ventral rami, and leaves the pelvis via the greater sciatic foramen, below the piriformis. The inferior gluteal nerve divides into branches that sink into the deep surface of the gluteus maximus (Figure 16-4).
• The pudendal nerve is the chief nerve of the perineum and of the external genitalia. Only a small segment of this nerve is seen in the gluteal region (Figure 16-5). The pudendal nerve arises from the anterior surfaces of S2, S3, and S4 rami, passing back between the piriformis and coccygeus muscles, medial to the pudendal vessels. The pudendal nerve and its accompanying vessel exit the greater sciatic foramen to enter the pudendal canal through the lesser sciatic foramen, having passed over the ischial spine. The spine can be palpated per vaginam, and this serves as the guide for local anesthetic injection, even if the fetal head is low in the pelvis. The nerve runs forward into the ischiorectal fossa to lie in the lateral wall of the fossa.
Surgical Technique
Patient Positioning
• For a buttock-level procedure, the patient is placed prone with a folded sheet under the pelvis on the operated side.
• The knees are slightly bent and padded, and care is taken to protect the ankles and feet.
• The lower leg or legs are prepped, and are draped as well if harvesting of sural nerves for grafts is anticipated.
Incision
• A variety of incisions is available. In many cases the pathology is at the sciatic notch, so it is crucial that this region be clearly seen. Localized muscle-splitting incisions may be fashioned through the gluteus maximus, provided the surgeon knows with certainty that the nerve injury is localized to that position (e.g., a stab wound) (Figures 16-6 and 16-7). In complex injuries of uncertain extent (e.g., after previous hip surgery), the classic operation is employed.
• The preferred incision begins just inferior to the posterior inferior iliac spine. It lies close to the upper free border of the gluteus maximus and then turns downward over the lateral insertions of that great muscle. If the upper thigh portion of the sciatic nerve is needed to define normal nerve distal to the injury, the incision is carried into the buttock crease and then distally, between the hamstring muscles (Figure 16-8).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree