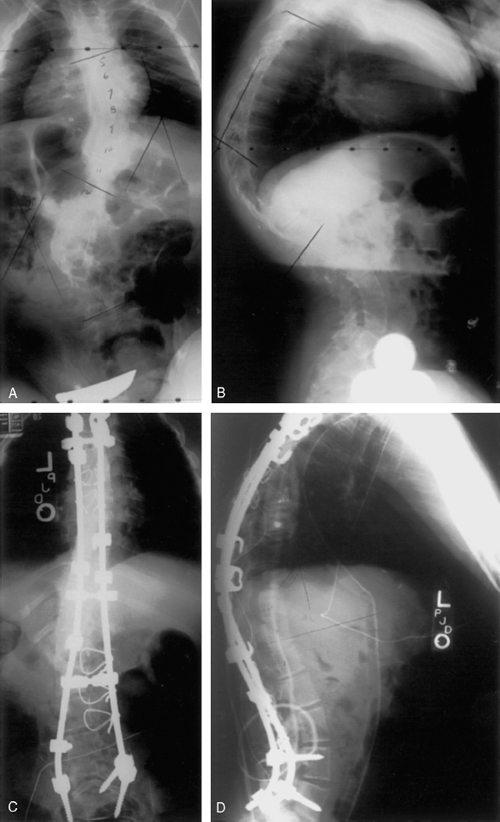
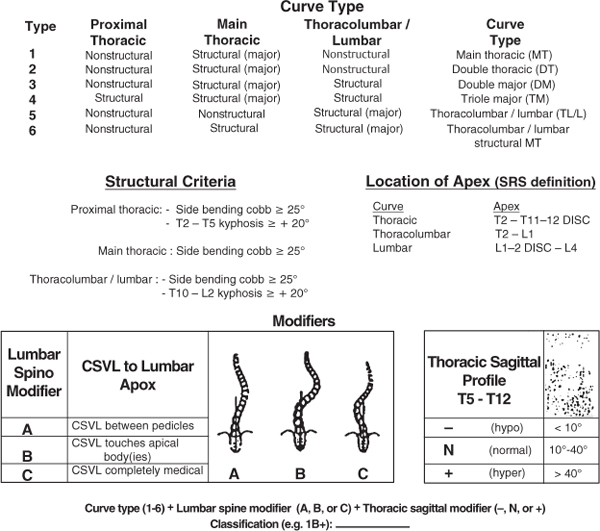
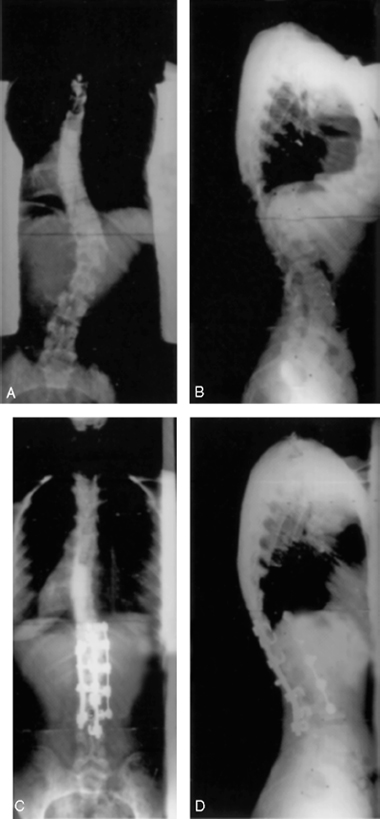
17 I. Classification A. Nonstructural: postural, sciatic, inflammatory, and compensatory B. Structural (Scoliosis Research Society) 1. Idiopathic (85%) a. Infantile (<3 years) b. Juvenile (3 to 10 years) c. Adolescent (10 years through maturity) 2. Neuromuscular a. Neuropathic: cerebral palsy, syringomyelia, poliomyelitis, spinal muscular atrophy, Freidrich’s ataxia b. Myopathic: arthrogryposis, muscular dystrophy, myotonia dystrophica 3. Congenital: diastematomyelia, spina bifida, hemivertebra, wedge vertebra, unsegmented bar with contralateral hemivertebra, block vertebra 4. Neurofibromatosis 5. Mesenchymal disorders: Marfan’s, Ehlers-Danlos 6. Rheumatoid disease 7. Trauma (fracture, surgery, radiation) 8. Extraspinal contractures (burns, thoracic surgery) 9. Osteochondral dystrophies 10. Infection 11. Metabolic disorders 12. Related to lumbosacral joint 13. Tumors I. Etiology A. Neuromuscular 1. Changes in the muscle fiber types and muscle spindles have been demonstrated. B. Hormonal C. Connective tissue 1. Elastic and collagen fibers are the primary elements that support the spine. 2. Abnormalities in the collagen/proteoglycan in the intervertebral disks have also been shown. D. Genetic: 5:1 female preponderance (>10-degree curves), familial (20 times greater in families) with monozygotic twin concordance rate of 73%, genetic (sex-linked trait with incomplete penetrance and variable expressivity) E. Melatonin or serotonin abnormalities II. Anatomic characteristics A. Lateral curvature or deformity in the coronal plane B. Decreased thoracic kyphosis or thoracic hypokyphosis (deformity in the sagittal plane) 1. Earlier accelerated spinal growth as compared with normal individuals may be related. C. Vertebral rotation: spinous process rotates toward concavity (deformity in the axial plane and causes rib hump) D. Patterns of thoracic scoliosis (King classification is frequently used, but not every thoracic curve fits into this classification) 1. Double major right thoracic and left lumbar (King I): lumbar curve is larger than the thoracic curve. 2. Right thoracic and compensatory left lumbar (King II): thoracic curve is larger than the lumbar curve. 3 Right thoracic (King III): left lumbar curve does not cross the midline. 4. Right thoracolumbar (King IV) 5. Double thoracic (King V) E. Classification is newer, more extensive and classifies the curves based on curve type, lumbar modifier, and thoracic sagittal profile (Fig. 17–1). F. Isolated lumbar or thoracolumbar curves III. Natural history and prognosis A. Prevalence: 25/1000 (2.5%) exhibit greater than 10-degree curves and (0.4%) 4/1000 exhibit greater than 20-degree curves. B. Factors contributing to curve progression 1. Curve magnitude: the greater the angulation and rotation, the greater tendency for progression. For example, a 20-degree curve has a 20% likelihood of progression, and a 40-degree curve has a 60% likelihood of progression. 2. Age: younger age is a more important prognostic factor than gender or family history. Ninety percent of spinal growth has occurred at puberty; however, this age has the highest risk of progression. 3. Risser score of skeletal maturity: score of 1 or less has a higher likelihood of progression 4. Shorter curves progress more 5. Location: the lower the curve is in the spinal column, the greater the likelihood of progression (thoracic < lumbar). 6. Flexibility: stiffer curves in immature individuals and more flexible curves in mature individual are more likely to progress. 7. Gender: girls are more commonly affected, especially for larger curves. 8. Positive family history 9. Slender spines IV. Diagnosis A. Screening: generally occurs in school children between age 10 and 14 1. Leads to a substantial number of referrals 2. One third of all referrals have scoliosis to some degree. B. History: age, gender, onset of menarche, pain, family history 1. Pain occurs in up to 30% of patients with IAS. 2. Peak growth in girls at age 11 to 12 and boys at age 13 to 14 C. Physical examination: 1. Observation: a. Asymmetry of shoulder level, breasts, waist, or pelvis b. Protruding scapula or ribs c. Loss of thoracic lordosis d. Adams forward bend test (1) Patient bends at the waist to 90 degrees. (2) During the process, assess for asymmetry in bending and rotational deformity of thoracic and lumbar curves. 2. Measurements a. Scoliometer is used to measure rib hump (rotational deformity on forward bending). b. Plumb line dropped from C7 indicates coronal balance relative to gluteal cleft. c. Leg length discrepancy 3. Neurological examination a. Deep tendon reflexes b. Abdominal reflexes (1) Check for symmetrical umbilical movement upon lateral to medial light stroke on the abdomen. (2) Asymmetrical movement correlates with neural axis pathology. D. X-ray examination 1. Cobb angle is used to measure the magnitude of the curve. The upper and lower end vertebrae of each curve are identified. A line is drawn at the upper end of the cranial end vertebra along the end plate or by marking the upper or lower margin of the pedicles. A line is then drawn at the lower end of the caudal vertebra of the curve, using the end plate or pedicles. A right angle to this line is then drawn. The angle to be measured is the angle formed by the two lines at the end vertebrae. 2. Risser sign indicates ossification of the iliac epiphysis, which starts at the anterior iliac spine and progresses posteriorly. A Risser 5 indicates the epiphysis has fused with the iliac crest. A Risser 4 indicates completion of spine growth. 3. Stable vertebra is determined by the center sacral line. 4. Ring apophysis fusion indicates cessation of all vertebral body growth potential. 5. Bone age is evaluated by X-ray of the left wrist and hand. The X-ray is compared with standards in the Greulich and Pyle Atlas. E. Pulmonary function test: greater than 70-degree curves have decreased vital capacity, particularly with hypokyphosis. F. Magnetic resonance imaging (MRI) indications 1. Neurological abnormalities 2. Congenital vertebral abnormalities 3. Juvenile and infantile onset 4. Rapid progression 5. Cutaneous manifestations of dysraphism V. Management A. Goals of treatment 1. Prevent progression and maintain balance 2. Maintain respiratory function 3. Reduce pain and preserve neurological status 4. Cosmesis B. Nonoperative treatment 1. Most patients with scoliosis do not have severe enough progression to require treatment. 2. Observation is indicated for curves <25 degrees in immature patients and >50 degrees in mature patients. b. A significant change is a progression of >10 degrees in curves <20 degrees and >5 degrees in curves >20 degrees. 3. Exercise: indicated only as an adjunct treatment especially for patients with obesity, back pain, lumbar hyperlordosis, flexible kyphosis, trunk and extremity muscle tightness 4. Orthosis: curve >30 to 45 degrees (first visit) and >25 degrees with documented progression in immature patients (Risser 3 or less) a. Not for cervicothoracic curves and hypokyphotic thoracic curves b. The goal is to prevent progression: Eighty-five percent of compliant patients do stop progression and improve (~50% correction), but most return within 5 degrees of original curve after the brace treatment is ceased. c. Protocol: the patient must wear the brace 23 hours a day until 2 years after menarche or Risser 4 and wean off in 1 year (part-time wear is also reported). d. Orthosis types (1) Thoracolumbar Sacral orthosis (Boston overlap) (a) Appropriate up to T8 apex (b) All curve types (c) Medium compliance (2)Bending brace (Charleston) (a) Thoracolumbar and lumbar curves (25 to 35 degrees) (b) Best compliance (3) Cervico Thoracolumbar Sacral orthosis (CTLSo) (Milwaukee) (a) Thoracic curves with apex above T7 (b) Low compliance 5. Electrical stimulation treatment has been abandoned. I. Indications for surgery A. Progressive curves >40 to 45 degrees in growing children B. Failure of bracing C. Progressive curves beyond 50 degrees in adults II. Goals of surgery A. Spinal and pelvic balance is more important than curve correction. B. Prevent respiratory compromise. C. Prevent back pain. D. Cosmesis III. Choice of posterior fusion level A. Curve patterns (King types) 1. Type I (S-shaped curve, where lumbar curve is larger and less flexible): fuse both thoracic and lumbar curve, but not below L4. 3. Type III (thoracic curve where lumbar curve does not cross the midline): fuse thoracic curve down to the stable vertebra. 4. Type IV (long thoracic curve where L4 tilts into the curve): fuse the entire curve down to the stable vertebra, L4 or L3. 5. Type V (double thoracic curves): fuse both curves from T1-T2 to the stable vertebra, particularly if the left shoulder is higher than the right shoulder. B. Distal extent of fusion 1. Should include Harrington stable zone, which is determined by two perpendicular lines from the sacral pedicles 2. Should include neutral vertebra, which is the nonrotated vertebrae 3. Generally, the distal vertebra is the stable vertebra, which is determined by the center sacral line. 4. If possible, avoid fusion beyond the L4 vertebra to preserve distal motion segments. 5. For type I and IV curves, the fusion may be stopped at one level above the stable vertebra if bending radiographs reveal the end vertebra becomes nonrotated and aligned within the Harrington stable zone. 6. Junctional kyphosis may result if the fusion is stopped at T12 in those curves with preoperative kyphosis at T12–L1 junction. 7. To prevent postoperative coronal decompensation, particularly in type II curves, overcorrection of the thoracic curve should be avoided. 8. For type IV, one level above stable vertebra can be fused. C. Upper level 1. Upper hook should be higher if hypokyphosis is present to correct the sagittal deformity. 2. Upper thoracic curve should be fused if the curve is structural, T1 is out of balance, and the left shoulder is high. IV. Indications for anterior fusion A. Isolated short and flexible thoracolumbar or lumbar curves without associated kyphosis may be treated with anterior fusion with anterior instrumentations such as Zielke rod, Texas Scottish Rite Hospital (TSRH) system, Isola and Moss-Miami. The area of fusion includes only the vertebrae of the structural curve. In performing anterior fusion of the lumbar spine, preservation of lordosis is important. B. A combined anterior and posterior procedure is indicated in the following thoracic curves. 1. A severe curve >90 degrees that is stiff and unbalanced. 2. Presence of predisposing factors to develop crankshaft phenomenon, which are Risser 0, Cobb angle >60 degrees, and apical rotation >20 degrees. 3. The procedure of choice is anterior discectomy and fusion with posterior fusion and instrumentation. V. Instrumentations A. Harrington rod technique utilizes distraction on the concavity and compression on the convexity of the curve. Sagittal correction is not well achieved. C. Luque rod with segmental sublaminar wires is still effective in paralytic scoliosis or cases with predominant thoracic lordosis. (Luque-Galveston technique is used to correct pelvic obliquity.) D. Multiple hook systems such as Cotrel-Dubousset, TSRH, Isola, Moss-Miami, etc. 1. More powerful in correcting deformities and have better results in reducing coronal and sagittal plane lmbalance 2. May be used so that either derotation or translation with cantilever bending forces are applied, followed by segmental fixation with hooks and/or screws 3. In performing any spinal instrumentation techniques, the goals of surgery must be remembered, which are obtaining solid fusion and balance. 4. Rigid instrumentations have advantages such as saving distal motion segments, avoidance of postoperative bracing, and facilitation of postoperative rehabilitation. a. Thoracic/lumbar pedicle screws (1) Provide three-column control (2) Allow for rotational/deformity control E. Anterior systems include Zielke, TSRH, Moss-Miami, anterior ISOLA, and Kaneda rods. 1. Most commonly used for thoracolumbar or lumbar curves 2. Anterior instrumentation may save one to two levels as compared with using posterior instrumentation systems. 3. Endoscopic anterior instrumentation a. Reduced morbidity VI. Surgical technique A. Intraoperative cell saver system B. Spinal cord monitoring and wake-up test or motor evoked potentials C. Fusion technique 1. Subperiosteal dissection out to the tips of transverse processes 2. Decortication, facet cartilage excision 3. Iliac crest autograft or rib graft from thoracoplasty D. Instrumentation techniques: Most deformity corrections are now performed using the pedicle screw based systems. VII. Postsurgical care, outcomes, and complications A. Bracing after surgery is not required. B. Patient slowly advanced in their activities until full recovery in 6 to 12 months. C. Depending on instrumentation used, correction percentage varies from 50 to 75%. D. Fusion below L3 increases the incidence of lower back pain. E. Posterior spinal instrumentation has a reoperation rate of 5 to 19%. F. Other complications 1. Delayed infection a. Incidence of 1 to 7% b. Requires hardware removal and antibiotics 2. Late-onset surgical pain a. Incidence of 5% b. Requires hardware removal 3. Pseudarthrosis a. Incidence of 3% b. Compression instrumentation or bone graft needed for treatment. VII. Idiopathic infantile scoliosis A. Usually detected at 2 to 3 months of age B. Greater incidence in boys than girls C. More common in England D. Ninety percent left thoracic E. Prognosis 1. Sixty to 70% resolve spontaneously. 2. Two types of progressive curves a. Benign curves are typically characterized by <1 year onset, double curves, and greater flexibility. b. Malignant curves are characterized by <1 year onset, thoracic location, and rigid curves. 3. Good prognosis if Mehta angle (rib-vertebral angle) is less than 20 degrees and the convex rib does not overlap the vertebral body on the posteroanterior radiograph (phase I). In phase II, there is an overlap between the rib and vertebral body, and the prognosis is worse. F. Treatment is bracing for curves over 30 degrees. If the curve is progressive, surgery is recommended. Options include subcutaneous rod or telescoping rod without fusion or combined anterior and posterior fusion. VIII. Idiopathic juvenile scoliosis A. Right thoracic pattern is most common. B. Variable progression: one third are observed, one third are braced, and one third require surgery. C. Brace if greater than 30 degrees. D. Surgery if progressive curve >45 degrees despite brace treatment, especially during puberty IX. Congenital scoliosis (Fig. 17–2) A. Failure of segmentation or formation or both B. Associated anomalies: genitourinary X. Paralytic scoliosis XI. Neurofibromatosis XII. Adult scoliosis A. General considerations a. Risk factors for lumbar curve progression (1) Lateral and rotatory listhesis (2) Large apical rotation 2. Spinal stenosis, disk disease, and osteopenia are associated pathology: asymmetrical loss of disk height and vertebra may contribute to the increase in Cobb angle. 3. Etiology of pain in adult scoliosis may be multifactorial. a. Pain often originates on the convexity of the curve due to muscle fatigue. This is followed by facet degeneration on the concave side. b. There is increased incidence of low back pain if lumbar curve is greater than 45 degrees. c. It is necessary to rule out other sources of pain such as abdominal aneurysm, renal stones, tumors, as well as disk disease and spinal stenosis. d. Pain, in the absence of a progressive curve, is rarely an indication for surgery. 4. Sciatica may result from nerve root compression in the concavity of the curve. 5. Respiratory compromise may occur resulting in dyspnea, pulmonary hypertension, and cor pulmonale. 6. Adults often have other medical comorbidities that make the surgery more risky. B. Evaluation 1. Careful history and examination including previous evaluations for scoliosis 2. X-rays: standing anteroposterior and lateral to measure magnitude of curve. These X-rays should be compared with any previous X-rays to document progression. Bending films are useful for determining the flexibility of the curve for preoperative planning. Further diagnostic testing, such as myelogram and computed tomography or MRI scan, is indicated when signs of nerve root compression are present. 3. Discography is sometimes utilized to localize pain in selected cases. 4. Ferguson view X-rays a. Special view X-ray used to examine the lumbosacral junction b. Beam is directed 30 degrees cephalad and focused on the L5–S1 junction. C. Treatment 1. Conservative treatment is indicated for nonprogressive curves causing localized back pain. The treatment plan incorporates the general principles of treating back pain including brief period of rest, nonsteroidal antiinflammatory drugs, stretching, exercise program, and nerve blocks. 2. Bracing is occasionally helpful for pain relief but not for sciatica, curve progression, or respiratory compromise. 4. Techniques a. Relatively flexible thoracic curves or balanced double major curves require posterior fusion and instrumentation. b. Rigid and severe unbalanced thoracic curves (greater than 80-degree curves) require anterior release and fusion followed by posterior fusion and instrumentation. c. Relatively flexible thoracolumbar or lumbar curves require anterior fusion with instrumentation (if there is no kyphosis and the curve is limited to T10 to L4). d. Severe and rigid thoracolumbar or lumbar curves >75 degrees redundan statement and associated kyphosis require anterior release and fusion followed by posterior fusion and instrumentation. e. Degenerative scoliosis with radiculopathy requires posterior laminectomy and fusion with transpedicular instrumentation of the lumbar spine with or without anterior fusion. 5. Complications a. Higher than adolescent spine, especially pulmonary problems b. Pseudarthrosis is less for combined anterior and posterior approach than posterior fusion alone. c. Flatback syndrome (loss of lumbar lordosis) may result if the posterior surgical techniques produce a distractive force or if the anterior technique produces significant compression force along the lumbar spine. Segmental instrumentation and preservation of the lumbar lordosis and sagittal balance are critical. d. Infection (1) Incidence of 0.5 to 8% (2) More common with posterior surgery e. Neurological complications (1) Incidence 1 to 5% (2) Most common with combined posterior and anterior surgery f. Pulmonary embolism (1) Incidence 1 to 20% XIII. Neuromuscular scoliosis (Fig. 17–4) A. General considerations 1. Bracing does not prevent the natural progression of the scoliosis. 2. Differences in surgical approach include longer fusions and operating on smaller curves. 3. Hooks and screws are used more frequently. 4. Segmental Luque are wires used. 5. Increased rates of complications B. Cerebral palsy 1. Scoliosis affected by the imbalance of the paraspinal muscles 2. Surgery a. Curves greater than 50 degrees
Scoliosis
♦ Idiopathic Adolescent Scoliosis
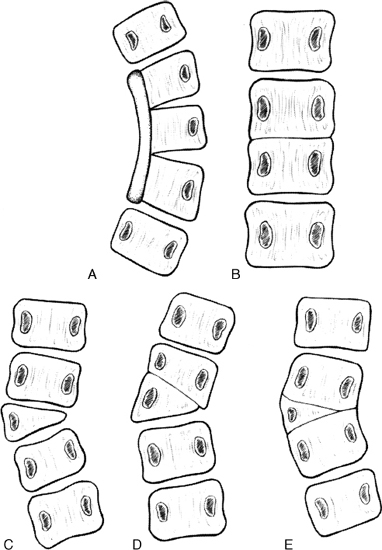
♦ Operative Treatment of Idiopathic Scoliosis (Fig. 17–3)
Neupsy Key
Fastest Neupsy Insight Engine