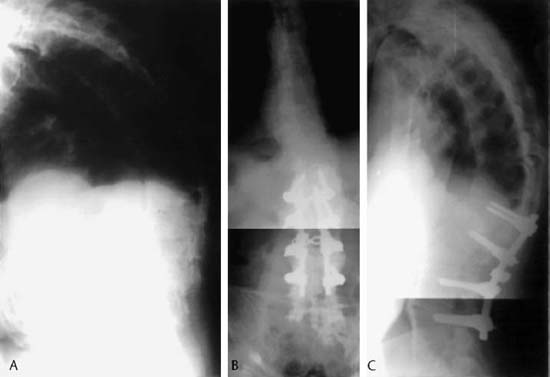
22 I. Ankylosing spondylitis (Fig. 22–1) A. General considerations 1. Affects patients in their second and third decades of life 2. Men and women are affected equally. a. Men typically have a more severe disease expression. b. Prevalence is 1 in 1000. c. Mostly Caucasian (HLA-B27) B. Pathogenesis 1. HLA-B27 positive in 88 to 96% of patients 2. Inflammatory arthritis of the spine that also involves sacroiliac and peripheral joints a. Cartilage destruction and bony erosion b. Earliest changes are in the sacroiliac joints. 3. Enthesitis at tendon and ligament bony insertions a. In the spine, this occurs at the insertion of the anulus fibrosus. C. Clinical findings 1. Insidious onset a. One to 3 years of symptoms before diagnosis 2. Symptoms include low back pain and stiffness, which are worse in the morning and better with activity. 3. Fifteen to 25% have peripheral joint arthritis. 4. Physical findings a. Limitation of lumbar motion (Shober test) b. Decreased chest expansion c. Positive sacroiliac stress maneuver (Patrick’s test) d. Rigid kyphotic spine (1) Most effective measure of spinal deformity is the chin-brow to vertical angle e. Compensatory hip flexion contractures 5. Nonskeletal manifestations a. Aortic insufficiency b. Cardiac conduction defects c. Uveitis d. Pulmonary fibrosis (cause of death in 10% of patients) D. Radiographic findings 1. Sacroiliitis erosion a. Reactive bone and fusion of the joint (on the lower portion of iliac side first) b. Bilateral and symmetric 2. Spine a. Syndesmophyte formation from the margins of the vertebral bodies (“bamboo spine”) (1) Vertical paravertebral ossification b. Erosion of the vertebrae (“squaring of the vertebral body”) c. Osteoporosis, disk and apophyseal joint narrowing 3. Occult fractures a. Occur with minimal trauma b. Plain radiographs can be difficult to interpret c. Computed tomography can be hard to interpret because of the difficulty in obtaining true axial cuts. d. Magnetic resonance imaging is the most reliable test for occult fractures and hematoma evaluation. 1. Nonoperative a. Breathing exercises b. Isometric exercise of the muscles c. Range of motion d. Nonsteroidal antiinflammatory medications 2. Surgical management a. Indications (1) Flexion deformity associated with pain and neurological compromise (2) Loss of horizontal gaze (e.g., chin on chest deformity) (3) Unstable spine fractures b. Spinal deformity in ankylosing spondylitis (1) Loss of lumbar lordosis and increased cervical and thoracic kyphosis (2) Primary location of disabling deformity should be assessed. (3) Osteotomies (a) Cervical (i) Osteotomy at C7–T1 junction with laminectomy from C6 to T2 is considered for primary cervical kyphosis. (b) Thoracic (i) In severe kyphotic thoracic deformity, multiple posterior thoracic resection osteotomies can be done after anterior osteotomies. (ii) Costotransverse osteotomies (iii) Thoracic kyphosis can often be addressed via a lumbar osteotomy. (c) Lumbar (i) Osteotomies are performed typically between L2 and L4. * Closing wedge osteotomy (e.g., pedicle subtraction osteotomy) (ii) High neurological complication rate (up to 9%) * Closing wedge osteotomy appears to be safer than opening wedge. II. Reiter’s syndrome A. Classic clinical triad 1. Urethritis 2. Conjuctivitis 3. Polyarthritis B. Ninety percent of patients HLA-B27 positive C. Microbes implicated in pathogenesis 1. Shigella, salmonella, yersinia, and campylobacter D. Radiographic findings 1. Periostitis in the heel and toes 2. Sacroiliitis (unilateral) 3. Nonmarginal asymmetric syndesmophytes (large and bulky) A. Seven percent of patients with psoriasis B. Arthritis precedes skin lesions in 15% of cases. a. Skin lesions include balanitis circinata, ulcers in the oral mucosa, and keratoderma blennorrhagica. C. Sacroiliitis is unilateral and asymmetric. D. Laboratory findings 1. HLA-B27 positive in 20% E. Treatment 1. Physical therapy 2. Medications a. Aspirin, indomethacin, or naproxen F. Shares many common musculoskeletal findings with Reiter syndrome IV. Enteropathic arthritis (inflammatory bowel disease) A. Shares many musculoskeletal features with Ankylosing Spondylitis (AS). B. HLA B-27 positive in 5% C. More common in Crohn’s disease than in ulcerative colitis D. Spinal involvement independent of bowel disease 1. Peripheral arthritis following disease exacerbations E. Marginal (starting at the end plates) symmetric syndesmophytes F. Sacroiliitis is bilateral and symmetric. Danisa OA, Turner D, Richardson WJ. Surgical correction of lumbar kyphotic deformity: posterior reduction “eggshell” osteotomy. J Neurosurg 2000;92:50–56 Halm H, Metz-Stavenhagen P, Zielke K. Results of surgical correction of kyphotic deformities of the spine in ankylosing spondylitis on the basis of the modified arthritis impact measurement scales. Spine 1995;20:1612–1619 Simmons E. Kyphotic deformity of the spine in ankylosing spondylitis. Clin Orthop Relat Res 1977;128:65–68 Simmons E. The surgical correction of flexion deformity of the cervical spine of ankylosing spondylitis. Clin Orthop Relat Res 1972;86:132–139 Simmons EH, Graziano GP, Heffner R. Muscle disease as a cause of kyphotic deformity in ankylosing spondylitis. Spine 1991;16:S351–S360 Weatherley C, Jaffray D, Terry A. Vascular complications associated with osteotomy in ankylosing spondylitis: a report of two cases. Spine 1988;13:43–46
Seronegative Spondyloarthropathies
Suggested Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







