Shunt Settings
First, ventriculoperitoneal (VP) shunt placement is the treatment of choice for patients with NPH.1 Alternatives, such as endoscopic third ventriculostomy, have not been proven to match the clinical results achieved by shunt placement. Ventriculoatrial (VA) shunts may be used as an alternative, but they should be used only in patients with impairment of abdominal absorption capacity (e.g., following extensive abdominal surgery or peritonitis); otherwise, the risk of surgery and the time consumed by the procedure favors the use of VP shunts.
Second, the initial opening pressure of the valve should be low. In my practice, the valve is always set to 5 cm H2O opening pressure. Some evidence suggests that clinical improvement after shunt implantation is significantly better with a low opening pressure.2,3 This low opening pressure is beneficial for the patient, and there is no reason for not providing this benefit to patients.
Third, if the initial opening pressure is low, then there is an increased risk for overdrainage. To reduce this risk, the shunt should carry a gravitational unit or another device that reliably prevents overdrainage. Therefore, a standard gravitational unit with an opening pressure of 20 cm H2O is recommended for patients with idiopathic NPH (iNPH).
Fourth, adjustability plays an emerging role in today’s shunt technology, and physicians and patients demand it. Adjustability (note that “adjustability” is not the same as the term “programmable” here, because shunts today are not truly programmable, only adjustable) may prevent the need for revisional surgery if the shunt does not fit perfectly well. At the time of publication, there has not been a randomized, controlled prospective study confirming the advantage of an adjustable versus a fixed-pressure valve. However, empirical data and clinical experience favor adjustability over fixed-pressure valves.
In iNPH, adjustability plays a role at the 3-year or 4-year follow-up period when the condition of patients is likely to have deteriorated compared with the improved status initially seen after the shunt was placed. At this time, the opening pressure can be lowered to 0 to 3 cm H2O. Patients may benefit from the further reduction of the opening pressure, at least for a certain amount of time. Again, patients are likely to be protected from overdrainage by the gravitational unit or by another adequate device.
In patients with iNPH, there is no need to adjust the valve immediately after surgery. NPH is chronic and long lasting, so improvement will take some time (usually weeks or months). Therefore, it is recommended to perform the first valve adjustments—if any—3 months after surgery.
In summary, the optimal setting for the treatment of a patient with iNPH is a VP shunt with an opening pressure of 5 cm H2O and a gravitational unit (shunt assistant, proSA), which will prevent overdrainage, at 20 cm H2O. Adjustability is beneficial for the patient, and the first adjustments should be performed at about 3 months after surgery.
10.2 Shunt Settings
There are a number of shunts and valves with different pressure settings. The literature gives no clear evidence-based answer about the best shunt system; however, there are many logical reflections and experiences that may help when choosing the appropriate valve. Naturally, a place for discussions and improvements will remain. Currently, there is no exclusive “right way” to perform a shunt or to select the shunt components, so there will be more than one good solution. The following sections will explain how to choose the correct shunt and components and detail the reasons for my decisions. Besides theoretical considerations, the author (U.K.) will also reflect upon economic aspects. The decision-making process will be divided into these parts:
Select:
VA versus VP shunt
Frontal or occipital bore hole
Valve:
Opening pressure
Programmable or fixed valve
Shunt configuration
Catheter material
10.2.1 Ventriculoatrial versus Ventriculoperitoneal Shunt
The selection between a VA and a VP shunt must be decided in favor of the VP shunt because both shunts have about the same frequency of complications, but complications in VA shunts are potentially more severe.4,5,6 This is especially true in the elderly patient population with chronic heart and lung disease, chronic obstructive pulmonary disease, and pulmonary hypertension; the presence of cardiac complications are even more dangerous. Of course, if there are any contraindications (e.g., ascites, extensive peritoneal scarring), then VA shunts are an appropriate alternative.
10.2.2 Frontal versus Parietal/Occipital Bore Hole
There are no clear data to support one approach or the other for the ventricular catheter. However, there are three main reasons why a frontal bore hole should be used, namely:
The probability of hitting the ventricular system with the ventricular catheter is higher, because the tolerable diversion from the optimal angle where the ventricle is still hit is wider in the frontal region than in the occipital region (▶ Fig. 10.1, ▶ Fig. 10.2).
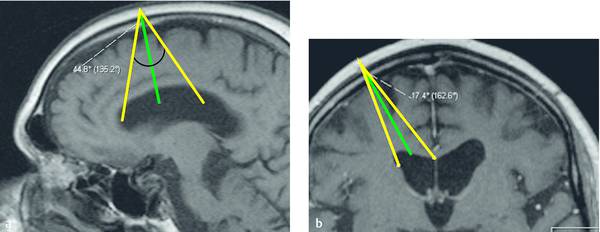
Fig. 10.1 Magnetic resonance imaging (MRI) with optimal track for a frontal ventricular catheter (green line) with tolerance of track deviation where the catheter still enters the ventricle (yellow lines) in the (a) sagittal and (b) coronal planes. The wider the angle of the extremes of the tolerated tracks, the lower the risk of failed ventricle puncture (compare also ▶ Fig. 10.2).
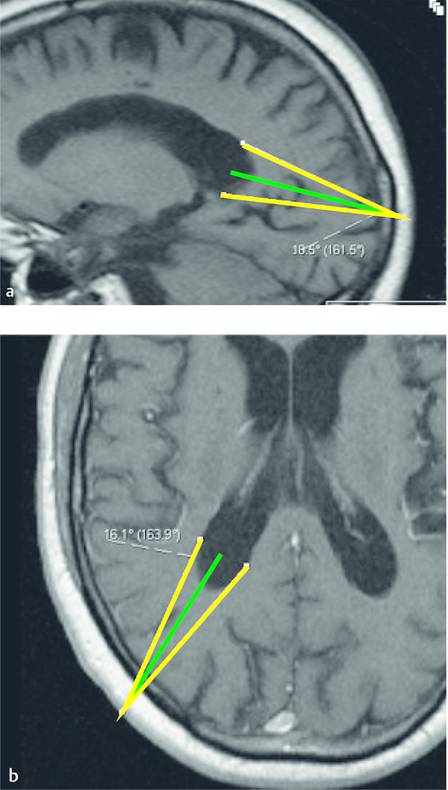
Fig. 10.2 Magnetic resonance imaging (MRI) with optimal track for a occipital ventricular catheter (green line) with tolerance of track deviation where the catheter still enters the ventricle (yellow lines) in the (a) sagittal and (b) axial planes.
The tip of the catheter is—if approached from the anterior—easy to locate in the frontal choroid plexus free zone of the lateral ventricle. Plexus invasion is a commonly described cause of shunt obstructions.7 Using the occipital approach, the ventricular catheter must be very long to reach with its perforations in the frontal located free plexus zone; this makes it more difficult.
Shunt revisions are associated with additional risk of intraventricular hemorrhage due to adherence to the choroid plexus.8
For these reasons, the frontal approach is preferable.
10.2.3 Selection of Valve Opening Pressure
Boon et al have shown clearly that we should use a low-pressure valve in patients with NPH,9 and, to counterbalance overdrainage, we should also use a gravitational device (Section ▶ 10.4).27
The Boon study9 supports the theoretical consideration that normal intracranial pressure (ICP) should be achieved with the shunt. Calculating the resulting ICP in a VP-shunted patient, the hydrostatic pressure difference between the head and the peritoneal cavity in an upright position, the abdominal pressure, and the valve opening pressure (VOP) should be considered. In the horizontal position, the hydrostatic pressure difference can be neglected, being almost 0. According to the equation,
 (20)
(20)
(see Box: ▶ Equation for calculating ICP and VOP in patients with VP shunts), the VOP should be around 0 to 5 cm H2O to achieve a physiologic ICP (of 5–10 cm H2O) in a horizontal position. In the upright position, a gravitational device should be implanted to counterbalance the difference in hydrostatic pressure. Usually a gravitational device with a resistance of 30 to 35 cm H2O is sufficient in patients with a body height of 160 to190 cm (5.3–6.2 ft).
Equation for calculating ICP and VOP in patients with VP shunts
 (21)
(21)
Abbreviations: GD, setting of gravitational device; HPD, hydrostatic pressure difference between ventricle and abdomen; IAP, intra-abdominal pressure; ICP, intracranial pressure; VOP, valve opening pressure; VP, ventriculoperitoneal.
Clinical experience supports a valve selection with a very low opening pressure (0–5 cm H2O) and a hydrostatic component of 30 to 35 cm H2O.
10.2.4 Should the Valve and/or the Gravitational Device be Programmable?
The equation for calculating the ICP and determining the VOP suggests that the choice of the valve is clearly defined so that a fixed valve is sufficient. However, the values of different parameters may change over time; for example, intra-abdominal pressure with increasing weight or constipation may influence the resulting ICP. In such cases, an adjustment of the valve would be desirable. However, adjusting a differential pressure valve has an important shortcoming: downregulating the differential valve not only results in improved drainage in the horizontal position but also accelerates drainage in the upright position, threatening overdrainage (see Chapter 9). Increasing the VOP would improve the drainage in the upright position but will worsen the drainage in the horizontal position. Therefore, an adjustment of the gravitational device would be advantageous: because the programmable gravitational shunt assistant (proSA) works in the upright position only, an adjustment can be performed with an effect in the upright position only, and not simultaneously interfere when in the horizontal position. However, the high prices of adjustable valves make routine use with low reimbursements difficult.
Theoretical considerations motivate us to use programmable shunt assistants rather than programmable differential pressure valves. The economic situation affects the selection also: In uncomplicated cases, we initially use (the cheaper) nonprogrammable valves with low opening pressures and hydrostatic pressure compensation around 30 to 35 cm H2O (see above). In revision surgeries or shunt implantations, when we expect problems, we select (the expensive) programmable valves.
10.2.5 Shunt Configuration (with or without a Cerebrospinal Fluid Reservoir)
If the shunt works well, no additional devices are needed. However, unfortunately, not all shunts work as well as they should. In those cases, an additional cerebrospinal fluid (CSF) reservoir is very helpful: CSF reservoirs permit through palpation, pumping, and even puncturing a rough diagnosis of the cause of shunt malfunction (see also Fig. 15.6). Below are brief diagnoses of the causes of a shunt malfunction:
If the reservoir can be pressed out by simultaneous occlusion of the proximal catheter, then this means that the valve and the distal catheter are not totally blocked. (However, a differentiation between mild, moderate, or distinct elevated opening pressure is not possible.)
If the reservoir does not refill promptly after lifting the finger from the proximal catheter after the first procedure, then the diagnosis of a proximal catheter obstruction or slit ventricles is made. This provides a hint of where to search further.
By “pumping” the reservoir (compressing the proximal catheter during pumping to avoid a reflux to the ventricle), a fibrin clot or debris, which may have occluded the valve or distal catheter, may be mobilized and the shunt function can be restored (in a few cases).
“Pumping” can be used as a noninvasive tap test: instead of a spinal tap test for re-evaluating the situation, about 100 to 200 “pumps” can pull a substantial volume (depending on the size of the pumping reservoir) from the ventricles.
In unclear cases, puncture of the CSF reservoir makes it possible to perform microbiologic examinations, ICP measurements, and a shuntogram.
For additional information, see Section ▶ 15.4.
The advantages of a reservoir during shunt failure are so convincing that the author (U.K.) almost always uses such a reservoir. He prefers the large Sprung Borehole Reservoir from Miethke (Potsdam, Germany), which has an integrated antireflux valve that eases pumping in higher volumes (the antireflux valve helps pumping because no additional occlusion of the proximal catheter is necessary). The disadvantage is its size and, consequently, the cosmetic aspect in patients who are bald (using a frontal approach).
10.2.6 Selecting Catheter Material
Usually the clinician has only a few choices for the catheter. Currently, there are two main different catheters, namely, antibiotic impregnated (BACTISEAL) or nonimpregnated catheters. Silver-impregnated catheters are expected soon for shunts. Presently, the shunt infection rates in patients with NPH are low, at around 3% to 4%.12,13 However, this rate is still too high. The first studies with antibiotic-impregnated shunts have reported promising results13,14; however, there is still a worry about increasing resistance to antibiotics with all their negative side effects.15 The next obstacle to the use of these impregnated catheters in all patients is their high cost. However, if the reduction of CSF shunt infections can be proved without creating new problems with regard to antibiotic resistance, their use will be a must. Currently, antibiotic-impregnated catheters are used in only those patients who are at risk of noncurable infections.
10.2.7 The “Optimal” Shunt Setting
The optimal shunt would be an antibiotic-impregnated shunt with a programmable differential pressure valve, with a programmable gravitational device, and a CSF reservoir with an integrated ICP teletransducer. The teletransducer could guide us on how to properly adjust the valves. However, the costs would be higher than the reimbursement by most health insurance companies, thus making hydrocephalus treatment a money-losing business. This could lead to an extreme conservative indication for shunt surgery, thus withholding beneficial therapy from many patients. The future must show evidence-based results that detail what is really necessary and what is not. Responsible economic and medical indications and the use of sophisticated shunt devices are all necessary for us to help as many patients as possible without burdening the entire society.
10.3 Shunt Settings
The implantation of a valve-regulated shunt as the therapy of first choice is indisputable in patients with iNPH. The VP shunt for adults has gained wide acceptance internationally. Following more than 50 years of experience worldwide with valve-regulated shunt therapy of internal hydrocephalus, there are still substantial therapeutic problems that derive from the nonphysiologic principles of construction of these valves. These difficulties are reflected by the fact that more than 200 different valves are in the market today, with different construction principles, different characteristic curves for different valves, and different modes of operation.16,17
Conventional differential pressure valves have the disadvantage, particularly for patients with iNPH, that when set up in a vertical position, they tend to open suddenly, remaining open for too long while generating a suction force on the CSF space of the already atrophic, previously damaged brain. The fundamental question then becomes whether such suction phenomena, with consequent overdrainage complications, can be reduced or prevented by the use of gravitational valves.
10.3.1 Why Use Gravitational Valves?
Effective therapy of disease-specific symptoms following the implantation of a differential pressure valve with a lower valve setting in patients with iNPH has the disadvantage of a significantly greater overdrainage rate.2 The fundamental problem that the pressure gradient is increased when positioning the body axis in the vertical direction by the addition of a hydrostatic pressure component has, in the past, been countered using a variety of strategies. Early on, it was found that differential pressure valves with high opening pressures could prevent overdrainage, which, in particular, comes into effect in the vertical body position. However, this happens only at the expense of permanent underdrainage in the horizontal position when, because of the absent hydrostatic pressure component and the high opening pressure, drainage of CSF no longer takes place.18,19,20 Therefore, the occurrence of pressure peaks at night could not be compensated. The use of differential pressure valves does provide an effective therapy for disease-specific symptoms; however, a substantially greater rate of overdrainage must be accepted.2
With later constructions, such as the antisiphon device, malfunctions resulted because of the surrounding growth of scar tissue.21 The development of adjustable valves did indeed open up the possibility of programming the pressure to a value so high that overdrainage could no longer result, but then a sufficient flow of CSF could not be guaranteed. Only when gravitational valves that are capable of switching from one pressure level for the horizontal position and another for a standing position were developed was the decisive step taken to eliminate the problems previously referred to.22,23
The author (U.M.) has gained experience with gravitational valves since 1996.24 In the beginning, static and nonadjustable gravitational valves, such as the Miethke DUALSWITCH valve Aesculap, were implanted in patients with iNPH.23,25 Since 2004, in the majority of cases, adjustable gravitational valves, mostly the proGAV Aesculap, but also the combination of adjustable MEDOS CODMAN valves with the Miethke SHUNTASSISTANT Aesculap,20,25,26 have been implanted (▶ Fig. 10.3). Both types of valves or valve combinations allowed good intraoperative handling and the possibility of easy adjustment. The crucial disadvantages of a combination of an adjustable MEDOS CODMAN valve with a Miethke SHUNTASSISTANT Aesculap are the unintentional maladjustment of the valve and the necessity of X-ray control after each valve adjustment. With both types of valve, care must be taken to achieve precise vertical orientation of the gravitational valve to ensure trouble-free operation of the gravitational unit and to minimize potential complications of overdrainage.

Fig. 10.3 proGAV (adjustable valve/gravitational unit).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






