♦ Preoperative
Clinical Evaluation of Patient for Signs of Shunt Infection or Malfunction
- Fever, tachycardia, hypotension, elevated white blood count, C-reactive protein, or erythrocyte sedimentation rate
- Altered mental status, headache, vomiting, cranial nerve deficit(s)
Imaging
- Computed tomography (CT) scan to evaluate ventricular size–useful to have prior imaging for comparison
- A CT scan with contrast shuold be considered when evaluating for possible intracranial abscess or ventriculitis.
- Radiographic shunt series with plain films tracking entire shunt tubing to evaluate for possible disarticulations in the system, kinks, or breakage in the tubing distally
Shunt Evaluation
- If CT scan shows adequate fluid surrounding proximal shunt catheter, shunt bulb can be assessed for ability to depress and refill easily
- If there is suspicion of shunt infection, shunt shuold be sterilely tapped and the fluid sent for cytology, cell count, glucose, protein, gram stain, and culture
Medical Management
- If infection is suspected, recommend empiric broad spectrum antibiotic coverage (i.e., vancomycin and cefepime/ceftriaxone) until further specia-tion from cerebrospinal fluid (CSF) culture specimen. If possible, obtain CSF sample prior to starting antibiotic therapy.
- If distal shunt obstruction is suspected and patient is clinically stable while awaiting surgery, dexamethasone or acetazolamide may be helpful in alleviating symptoms, as well as high volume shunt tap.
♦ Intraoperative
- Generally done in the operating room (OR) under general anesthesia
- Consider bedside shunt externalization if patient is unstable for immediate OR transfer or if needed as a temporizing measure while awaiting OR availability
- Advantages: quick bedside procedure that can be done in potentially unstable patient; no anesthesia risks; no extrinsic factors affecting timing of surgery (i.e., OR staffing, room availability)
- Disadvantages: may be uncomfortable for patient, especially if distal catheter is difficult to find; limited exposure and shunting options; no cautery available
- Advantages: quick bedside procedure that can be done in potentially unstable patient; no anesthesia risks; no extrinsic factors affecting timing of surgery (i.e., OR staffing, room availability)
Positioning
- Patient shuold be placed supine with head turned shunt side up; small roll placed under the ipsilateral shuolder to help elevate the clavicle and straighten the neck
Planning of Sterile Scrub and Prep
- Strongly consider prepping out entire shunt system site in preparation for revision of any component of the shunt
Planning of Incision
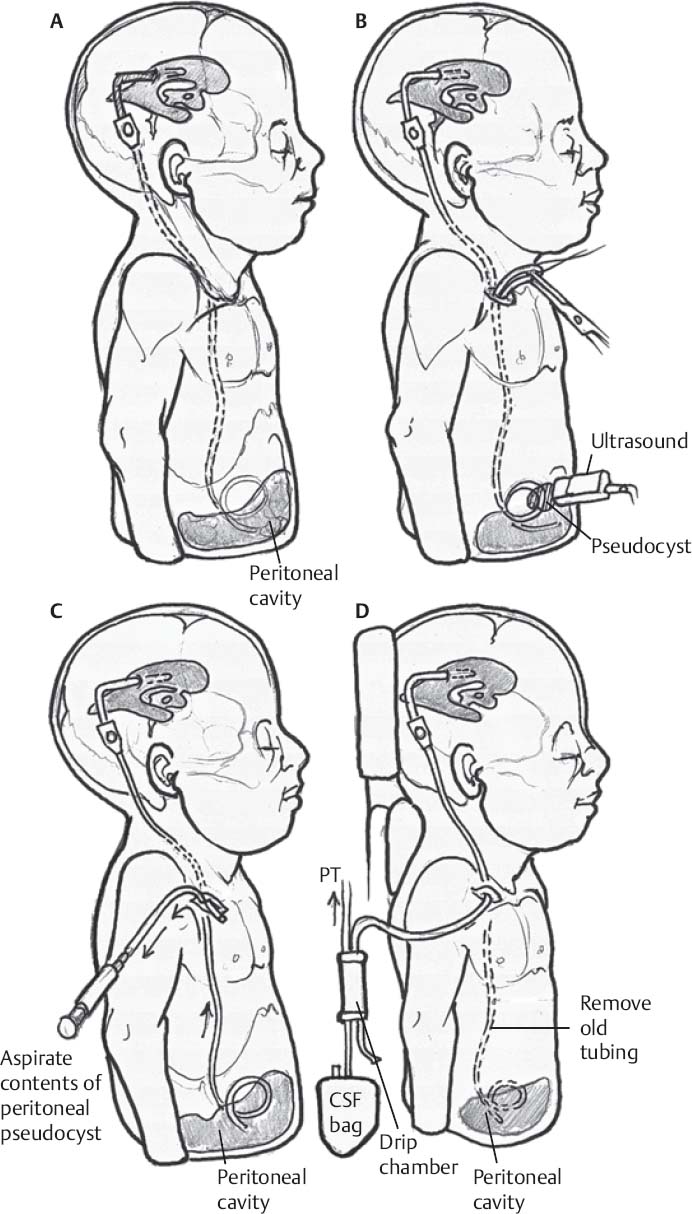
- Shuold be placed over area of skin where distal catheter is palpable–usually over clavicle (Fig. 82.1A)
- Infiltrate area over planned incision with 1 to 2% lidocaine, with care taken not to puncture shunt tubing
Externalization
- Once catheter is identified, gently pull out catheter distally (Fig. 82.1B). If catheter does not come easily, do not force it as this may represent abdominal adhesions that may result in bowel strangulation.
- If an abdominal pseudocyst exists, the catheter can be divided and peritoneal fluid aspirated via the distal catheter (Fig. 82.1C) prior to its removal.
- Once externalized, evaluate catheter for CSF flow.
- If no CSF flow, patient will need more extensive shunt revision/exploration.
- If patient undergoes a more extensive shunt revision, the distal catheter is tunneled out of the skin, usually through a distal incision already present.
- Hook distal catheter to sterile CSF collection bag; set pop-off to desired setting (usually 0 mm Hg) (Fig. 82.1D).
- Close incision with purse string nylon suture, taking care not to obstruct tubing with suture.
♦ Postoperative
- All patients with externalized shunt systems shuold be closely monitored for changes in neurologic status and CSF output
- Antibiotic treatment as outlined earlier; monitor CSF profile for infection clearance over few days
Only gold members can continue reading. Log In or Register to continue







