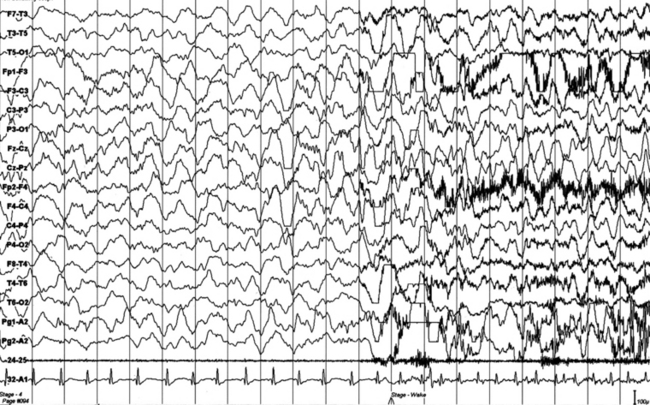
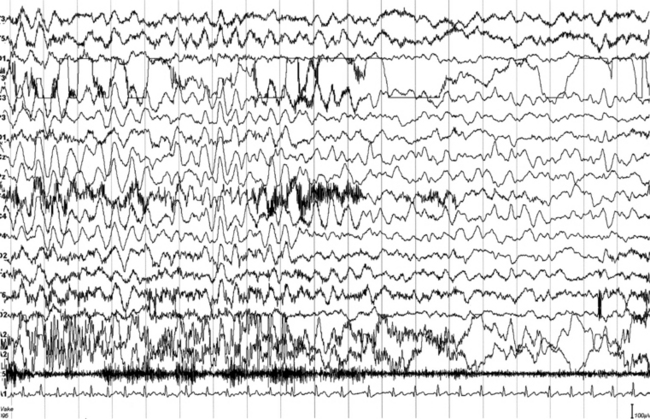
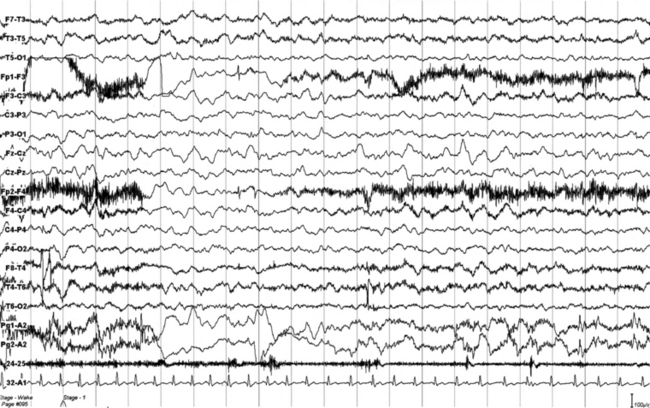
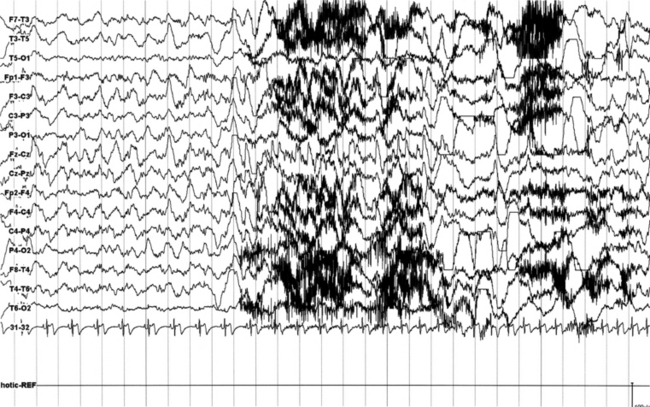
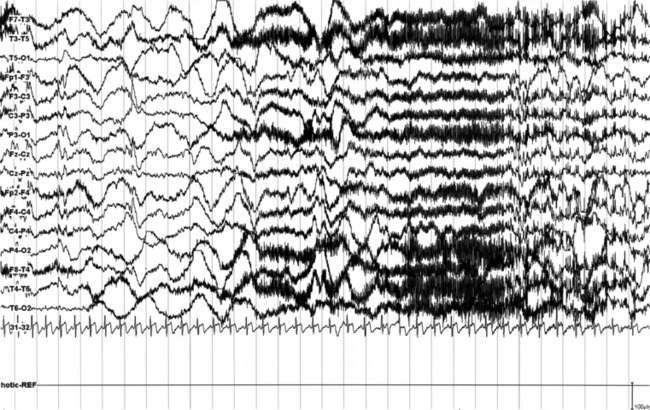
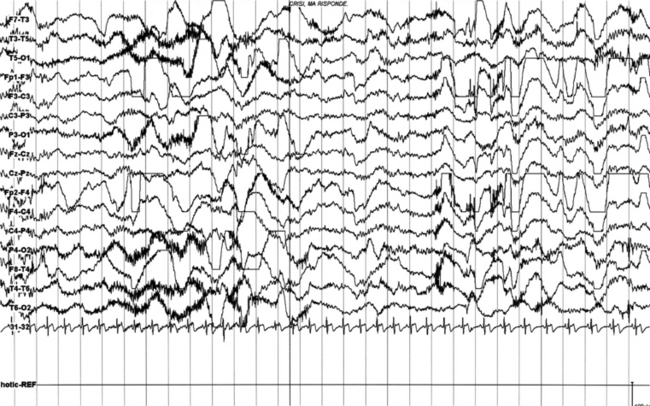
Chapter 11 1. Paroxysmal arousals and awakenings 2. Hypermotor syndrome with choreoathetoid, ballismic, bipedal, bimanual, cycling movements (originally termed nocturnal paroxysmal dystomia) 3. Asymmetric tonic and dystonic posturing 4. Epileptic nocturnal wandering resembling agitated somnambulism Most interictal epileptiform discharges are triggered during NREM stages 1 and 2 but occasionally in stage 3 sleep. In epileptic patients NREM sleep acts as a convulsant, causing excessive synchronization and activation of seizure in an already hyperexcitable cortex. In contrast, rapid eye movement (REM) sleep generally behaves like an anticonvulsant because of inhibition of thalamocortical synchronizing mechanism and tonic reduction of interhemispheric impulse transmission through the corpus callosum. Overnight polysomnography (PSG) using multiple channels of EEG recording combined with simultaneous video recording is the single most important test for evaluating nocturnal seizure. For recognition of epileptiform patterns in the EEG and CSWS see Chapter 2. In this section of the atlas we provide several case vignettes along with overnight EEG and PSG segments showing characteristic patterns (Figs. 11.1 to 11.21). FIGURES 11.1 TO 11.3 Polysomnographic (PSG) sequence of a nocturnal frontal lobe epilepsy seizure in a 10-year-old boy with onset of episodes during sleep at the age of 6½ years and characterized by arousal with sudden elevation of head and trunk, sitting, fearful expression, sometimes jumping ahead or ambulating, and rare similar episodes during wakefulness. Wake electroencephalogram (EEG) is normal, and sleep EEG shows rare sharp waves on Fz-Cz channel. Duration, less than 15 to 20 seconds, sometimes 30 seconds for prolonged episodes; frequency, 7 to 10 per night, with similar morphological characteristics and stereotypical features; good response to carbamazepine. The montage of PSG is EEG (top 16 channels), ROC (Pg 1-A2), LOC (Pg 2-A2), submental electromyogram (24-25), and electrocardiogram (32-A1). Epoch is 20 seconds. FIGURES 11.4 TO 11.6 A seizure during sleep probably arising from frontal lobe emerging from slow wave sleep (SWS) and characterized by awakening followed by choking sensation. We recorded two episodes in that night. PSG shows an awakening from SWS followed after 10 seconds by an epileptiform discharge probably starting from frontotemporal leads (right), spreading bilaterally in the electroencephalogram (EEG). The patient’s episodes had been misdiagnosed as panic attack in the past. He is a 23-year-old man whose episodes started at 12 to 13 years of age. There is no family history of epilepsy. The montage is only EEG and electrocardiogram, and we recorded the episode during a morning video-PSG after sleep deprivation the night before.
Sleep and Epilepsy
Sleep and Epilepsy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree







