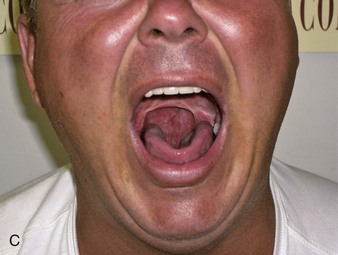
Chapter 13 13.1 Examination of the Patient with Suspected Sleep Apnea Sleep apnea can occur in any age group, in both genders, and in all ethnic groups. It often runs in families. Many patients do not fit the stereotype of the obese middle-aged man; the child shown in Figure 13.1-1 had sleep apnea caused by enlarged tonsils. The mother and her son in Figure 13.1-2 both had sleep apnea; she had hypothyroidism (see Chapter 14.1), and her son was obese. The two brothers shown in Figure 13.1-3, A, had sleep apnea, as did both of their parents. In some patients, inspection of the face can reveal the disease—for example, thyroid disease (see Chapter 15.1) or acromegaly (see Chapter 15.2)—that may be causing sleep apnea. Inspection can also give insight into physiologic abnormalities. Hyperpigmentation on the forehead, resembling acanthosis nigricans, may be present in the patient with sleep apnea (child or adult) who sleeps sitting up with the forehead resting on a forearm resting on a table (see Fig. 13.1-3, B). This is often found in patients with very severe apnea because it is the only position they can sleep in. In many instances sleep apnea is apparent at the first meeting with the patient. For example, drooping eyelids suggest sleepiness (Figs. 13.1-4 and 13.1-5, A). Floppy eyelids have also been associated with sleep apnea (see Fig. 13.5, B). Arched eyebrows can be a sign that the patient is trying to open her eyelids. Figure 13.1-5 Eyelids of patients with sleep apnea. The patient shown in Figure 13.1-6 is obese, cyanotic, and has bloodshot eyes. The latter finding was related to polycythemia. Obesity hypoventilation syndrome or overlap syndrome should be suspected when a patient has these findings. All patients with Down syndrome should be suspected of having sleep apnea (Fig. 13.1-7). Abnormalities in the skeletal structures of the face can lead to an abnormal position of the adjacent structures or attached soft tissues. Such abnormalities can obstruct the nasal or pharyngeal airways (Figs. 13.1-8 and 13.1-9). Figure 13.1-9 Facial structure and sleep apnea. Congenital facial abnormalities may be pervasive and may affect the development of the maxilla, mandible, and other structures that include those involved in the auditory system (see Fig. 13.1-10). Such patients may also be born with a cleft palate. The patient shown in Figure 13.1-11 appeared on initial inspection to have a prognathic mandible; note the concave facial profile. In fact, he has a large fat pad over his chin that gives the appearance of a prognathic mandible. More detailed examination of his facial features indicated that he has maxillary insufficiency (note his flat face and small cheekbone, or zygomatic bone); crowding of the mandibular anterior teeth may be indicative of an undersized mandible (Fig. 13.1-12). The 8-year-old child shown in Figure 13.1-13, A, was referred because of sleepiness, poor school performance, high blood pressure, and a family history of sleep apnea. He responded to continuous positive airway pressure treatment. He has a small lower jaw (mandibular retrognathia) that was only apparent when his bite was examined. Note the convex facial profile, which is a feature of a child with an underdeveloped mandible. Men with a retrognathic jaw often grow a beard in an attempt to improve their appearance (see Fig. 13.1-13, B). Retrognathia causes the patient’s tongue to rest in a more posterior and superior position, thus impinging on the pharyngeal airway. Figure 13.1-13 Retrognathia. Thus a receding chin is a sign of mandibular insufficiency. Such patients usually have an overjet with mandibular anterior teeth excessively lingual (or posterior) to the maxillary anterior teeth. Figures 13.1-14 and 13.1-15 demonstrate the overjet during a lateral exam. Figure 13.1-16 shows a patient with complete overlap of the maxillary over the mandibular anterior teeth (excessive overbite) when fully in occlusion on the posterior teeth. Patients with protrusive maxillary anterior teeth (“buckteeth”) frequently have retrognathic mandibles. Some patients have an anterior open bite that may be the result of a severe tongue thrust or even a consequence of severe thumb sucking (Fig. 13.1-17). Patients with abnormal maxillary and mandibular arches and with asymmetry or crowding may have a micrognathic (small) mandible and may be at risk for sleep apnea. The crowding of the lower arch causes inadequate space for the anterior portion of the tongue to move anteriorly. This in turn may cause the posterior part of the tongue to “bunch up.” Such patients may develop a scalloped tongue from the tongue constantly pressing anteriorly (Figs. 13.1-18 through 13.1-21). The patient shown in Figure 13.1-22 has severe rosacea. This disease can lead to nasal obstruction and sleep apnea. Diseases that affect the nasal turbinates, such as allergic rhinitis, can also lead to nasal obstruction (Fig. 13.1-23). Other abnormalities that may be found include a deviated nasal septum, which in some patients can be associated with a high-arched palate. The patient shown in Figure 13.1-24 had severe trauma from a gunshot wound to his face that required extensive reconstructive surgery. His nose was entirely reconstructed. It does not have an airway leading to the nasopharyngeal airway, so he breathes exclusively via his oral airway, which has also had reconstructive surgery. The patient shown in Figure 13.1-25, A, had a broken nose; note the asymmetry. The patient shown in Figure 13.1-25, B, had been a boxer. The region below the nasal bone is wide and was hard to palpation; note the cyanosis of the lips. Figure 13.1-26, A, shows examination of the nares from below in a patient with a previous nasal fracture. Bulging of the septum in the left nostril is apparent. Note the size of the left nasal airway after application of an external nasal strip (Fig. 13.1-26, B). A high-arched palate is frequently present in patients with a narrow dental arch (see Fig. 13.1-27). It must be kept in mind that the nasal airway sits above the arch of the palate, and a high arch may impinge on the size of the nasal airway and cause a deviation of the nasal septum. Children with such anatomy may benefit from rapid maxillary expansion. Class I: Soft palate, fauces, uvula, and posterior and anterior pillars are visible (Fig. 13.1-28). Class II: Soft palate, fauces, and uvula are visible (Fig. 13.1-29). Figure 13.1-29 Mallampati class II. Class III: Soft palate, fauces, and only base of uvula are visible (Fig. 13.1-30). Figure 13.1-30 Mallampati class III. Class IV: Soft palate is not visible (Fig. 13.1-31). Tonsil size is graded on a scale from 0 (no tonsils) to 4 (“kissing tonsils” that touch at midline): Grade 0: Tonsils are absent. The uvula is abnormally wide and almost bifid. This is a variant of normal (Fig. 13.1-32). Grade 1: Tonsils are hidden behind tonsillar pillars. Grade 2: Tonsils extend to the pillars. In Figure 13.1-33, the right tonsil is grade 1, and the left is grade 2. Grade 3: Tonsils are visible beyond the pillars (Fig. 13.1-34). Grade 4: Tonsils are enlarged to midline (Fig. 13.1-35). In Figure 13.1-35, D, the right tonsil is much larger than the left and extends beyond the midline. It was initially difficult to visualize because it extended behind the uvula. This would be classified as equivalent to grade 4 enlarged tonsils. In Figure 13.1-36, a nubbin of left tonsillar tissue can be seen. This patient frequently awakened with a sore throat, and the pharyngeal tissues show evidence of trauma (redness) as a result of snoring. Figure 13.1-37 shows an unexpected finding in a sleep apnea patient: a tiny neoplastic lesion just to the right of the uvula. The most common surgical procedure involving the upper airway is uvulopalatopharyngoplasty, which usually involves removal of the uvula and variable amounts of the soft palate (depending on the surgeon), tonsils, adenoids, and redundant tissue in the pharynx. In the cases shown in Figures 13.1-38 and 13.1-39, uvulopalatopharyngoplasty was unsuccessful in treating the apnea. Note the differences in anatomic outcome in these examples. A large neck collar size is a robust statistical predictor of obstructive apnea, although more so in men than in women. The patient shown in Figure 13.1-40 has a neck collar size of 49 cm, or 19.3 inches. Most obese patients with apnea have a neck collar size of at least 43 cm, or 17 inches. Figure 13.1-40 Measuring neck collar size. Congenital abnormalities that involve the neck can also lead to sleep apnea. The patient shown in Figure 13.1-41 had severe sleep apnea as a result of Klippel-Feil syndrome. She also had polycystic ovary syndrome (see Chapter 16.1); note the acne on the face. Findings in the neck are also seen in diseases of the thyroid gland (see Chapter 15.1). Central obesity is a very common finding in sleep apnea patients. Note the striae in Figure 13.1-42. Bariatric surgery is commonly done to treat morbid obesity and may result in resolution of sleep apnea. The patient shown in Figure 13.1-43 continued to have sleep apnea after having lost more than 100 kg. Note the abdominal scar and redundant tissue in this male patient. In very obese patients who spend most of their time in bed, edema might not always be maximal in the ankles and feet (Fig. 13.1-44). When edema is very severe in a patient with a sleep breathing disorder, it is almost always in the context of a hypoventilation syndrome (Fig. 13.1-45). Chronic edema results in discoloration and may result in infections that are difficult to treat (Figs. 13.1-46 and 13.1-47). 13.2 Sleep Apnea in the Adolescent and Adult Sleep breathing disorders encompass a wide variety of respiratory problems that appear exclusively in sleep, affect sleep, or are exacerbated by sleep. The classification schemes presented in the International Classification of Sleep Disorders (ICSD) and in the ninth and tenth editions of the International Classification of Disease (ICD-9 and ICD-10) appear in Box 13.2-1 and Table 13.2-1. More sleep breathing disorders are listed in the ICSD than in the ICD, which can be a source of confusion. Also, not all the diseases in ICD-9 map to ICD-10. This chapter reviews these disorders in patients older than 10 years. Chapter 13.3 covers these disorders in younger children. Table 13.2-1 Sleep-Related Breathing Disorders ICD, International Classification of Disease. Among the obstructive SDB disorders, the line between normal and pathologic is at times unclear (Box 13.2-2). The mildest form of an obstructed sleep-related breathing disorder is intermittent snoring, which may be a nuisance but is without significant health sequelae. (Evidence is accumulating, however, that chronic snoring may have consequences similar to those of frank obstructive sleep apnea.) The most severe form of SDB is the obesity-hypoventilation syndrome, formerly called Pickwickian syndrome, which is associated with severe morbidity and very high mortality. Between these two extremes are disorders of gradually increasing impact on morbidity and mortality: persistent snoring, upper airway resistance syndrome (UARS), and obstructive sleep apnea (OSA) syndrome. In contrast to obstructive SDB, central sleep apnea (CSA) typically occurs in the absence of respiratory effort and has very different risk factors and morbidities than OSA. The different pathophysiology of the two apnea types is reviewed in Chapter 3.6. Symptoms have generally been present for years before the diagnosis is made. The cardinal symptoms of OSA appear in Box 13.2-3 and in Chapter 8. An interview of the patient or the patient’s bed partner or parent (see Chapter 13.3) will shed light on the symptoms and how they affect the patient’s life. The physical examination of the patient with SDB is covered in detail in Chapter 13.1. In OSA, the primary findings in adults are obesity, a crowded posterior airway, hypertension (especially difficult-to-control hypertension), and other abnormalities that may narrow the airway, such as retrognathia, an enlarged tongue, or a “birdlike face,” as seen in Treacher Collins syndrome. The comprehensive overnight polysomnogram is currently the most widely used diagnostic test to document sleep apnea. Home sleep testing is being increasingly used for diagnosis in patients with a high pretest probability of having sleep apnea (see Chapter 18). The current American Academy of Sleep Medicine (AASM) scoring manual specifies the use of an oronasal thermal sensor to assess airflow for apnea and a nasal pressure transducer to assess airflow for hypopnea. Information from a nasal pressure transducer may be misleading in a mouth breather, and the signal from a temperature sensor is not linear. Measuring end-tidal CO2 adds an additional dimension of helpful information. The reader is encouraged not to slavishly follow the manual at all times but rather to examine all the available data to assess and understand the physiologic abnormalities. Synchronized digital video is often invaluable in assessing the patient (see Chapter 21). In adults (those aged 18 years or older), both apneas and hypopneas must last at least 10 seconds. Apnea occurs when oronasal airflow is reduced by 90% or more from baseline, and hypopnea occurs when the nasal pressure transducer signal is reduced by 30% or more from baseline with a 3% or greater drop in arterial oxygen saturation (SaO2). An alternative rule for hypopnea requires a 50% or more reduction in nasal pressure transducer signal with a 4% or greater drop in SaO2 associated with an arousal. If respiratory effort is present during the event, the hypopnea is classified as obstructive; if effort is absent, it is classified as central. Figure 13.2-1 demonstrates a respiratory event that meets criteria for a hypopnea, with a marked reduction in the pressure transducer signal, but not the airflow or thermal sensor signal, and a drop in SaO2 from 90% to 86%. In children younger than 13 years, the length of the event changes from 10 seconds to two missed breaths as determined by the baseline respiratory rate (see Chapter 13.3). The scoring rules are flexible for ages 13 to 18 years and allow scoring either by adult or pediatric criteria. Figure 13.2-2 demonstrates a hypopnea in which the SaO2 has fallen to 90%. In Figure 13.2-3, the somewhat arbitrary nature of these definitions, as well as the difference in thermal and pressure signals, is demonstrated. The term respiratory effort–related arousal was coined to capture respiratory events that do not qualify as apneas or hypopneas (Fig. 13.2-4). However, although the 2012 scoring manual calls for either respiratory inductance plethysmography or polyvinylidene fluoride film signal or an esophageal pressure manometer to assess respiratory effort, the latter device is almost never used in routine clinical practice. Figure 13.2-1 Hypopnea. Figure 13.2-2 Hypopnea. Figure 13.2-3 Apneas and possible hypopnea. Figure 13.2-4 Respiratory effort–related arousal (RERA).
Sleep Breathing Disorders
Overall Inspection of the Patient
Facial and Jaw Structures
Inspection of the Face

A, Drooping eyelids in middle-aged man. B, Floppy eyelids in a middle-aged woman. Notice the arched eyebrows.
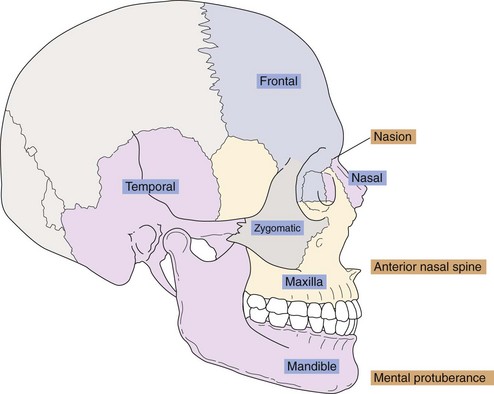
Bony Structures
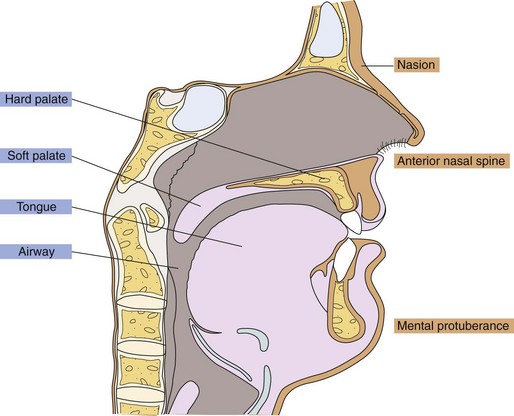
Landmarks (in orange) and anatomy (in blue), sagittal section.
Pervasive Facial Abnormalities
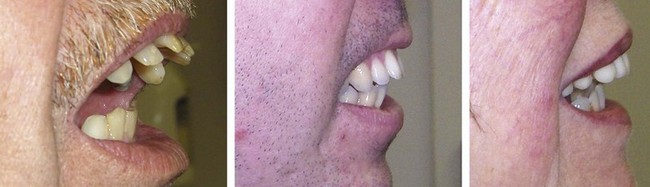
Maxillary and Mandibular Insufficiency
Small Lower Jaw


A, Child with retrognathia and sleep apnea. B, Male adults with retrognathic mandibles often grow beards.
Nasal Airway
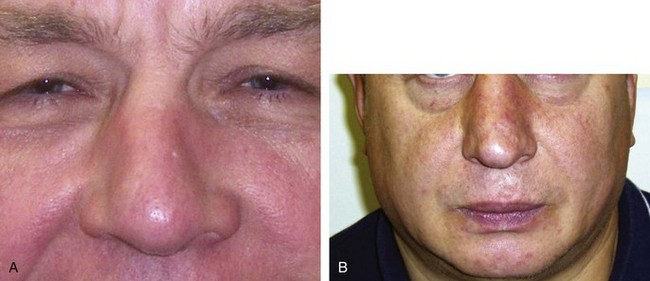
Diseases of the Nose and Nares
Trauma to the Nose and Nares
Traumatic Injury to the Nose
Examination of the Palate
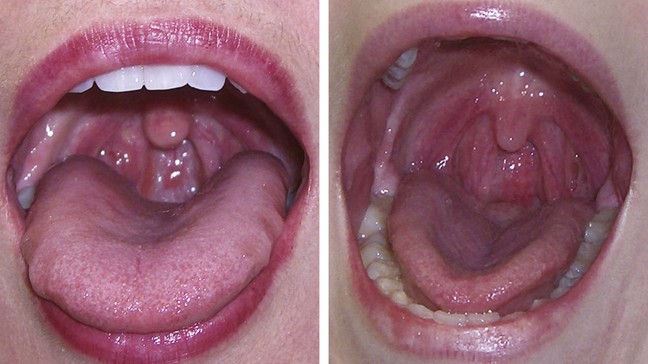
Examination of the Pharynx
Mallampati Classification


A, Posterior pillars and much of uvula are not visible. B, Tip of the uvula is not visible.


A, Only the base of the uvula is visible. B, The base of the uvula is barely visible.
Examination of the Tonsils
Variants and Abnormal Airway Pharyngeal Findings
Examination of the Neck

Neck collar size in excess of 43 cm is associated with sleep apnea.
Examination of the Abdomen
Examination of the Extremities
Peripheral Edema
Overview
DISORDER
ICD-9 CLASSIFICATION
ICD-10 CLASSIFICATION
Primary central sleep apnea
327.21
G47.31
Central sleep apnea as a result of Cheyne-Stokes breathing
786.04
R06.3
Central sleep apnea in conditions classified elsewhere
327.27
G47.37
Central sleep apnea because of a drug or substance
327.29
G47.39
Primary sleep apnea of infancy
770.81
P28.3
Obstructive sleep apnea, adult and pediatric
327.23
G47.33
Idiopathic sleep-related nonobstructive alveolar hypoventilation
327.24
G47.34
Definitions
Clinical Assessment
Symptoms
Examination
Laboratory Evaluation
Data Obtained in a Sleep Study
Scoring of Respiratory Events
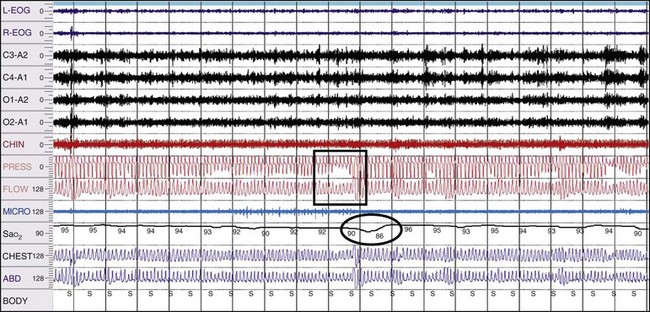
A 10-minute compressed epoch demonstrates the features of a standard hypopnea, with reduction to about 30% of baseline of the pressure transducer signal and 4% oxygen desaturation. Also shown is the difference in the pressure transducer and thermal sensor (flow) signals, with noticeable change in the former but little change in the latter.
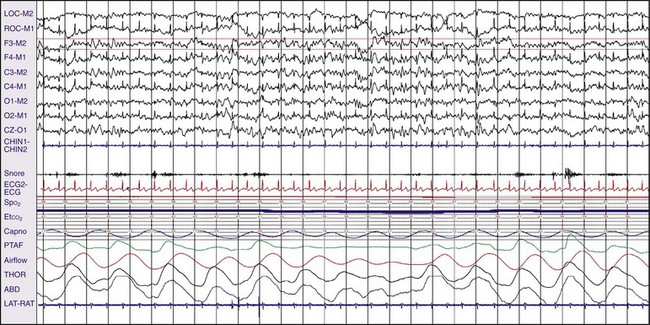
A 30-second epoch demonstrates a hypopnea with a fall in oxygen saturation (SaO2) from 98% to 90%. Flow measured by thermocouple is not quite reduced by 90%. The associated changes in heart rate and SaO2 are similar to what would be seen in an apneic episode; thus the separation between apnea and hypopnea is often arbitrary, and the two events are combined to generate the apnea-hypopnea index to show the number of events per hour of sleep.
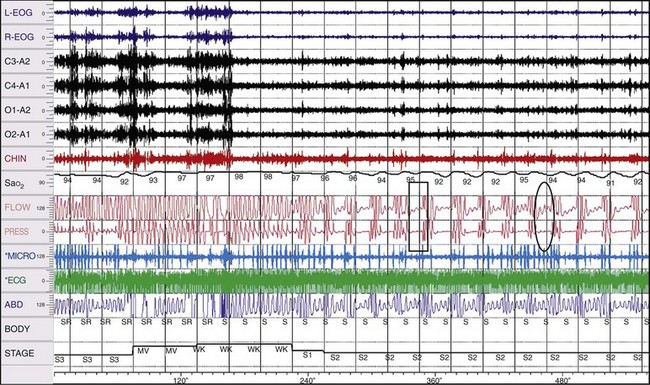
In this 10-minute compressed epoch, the FLOW channel represents the thermocouple signal, and the PRESS channel is nasal pressure. The event marked with the rectangle meets the criteria for an apnea because the flow signal is reduced by more than 90% of baseline for more than 10 seconds (~15 seconds). The oval marks an event that does not qualify as either an apnea or a hypopnea; the oxygen saturation falls by only 1% (from 95% to 94%), which precludes designating it as a hypopnea. The thermocouple signal is reduced by about 80% of baseline, and by standard criterion, a fall by 90% or more on the thermocouple (not flow transducer) channel is required for an apnea.
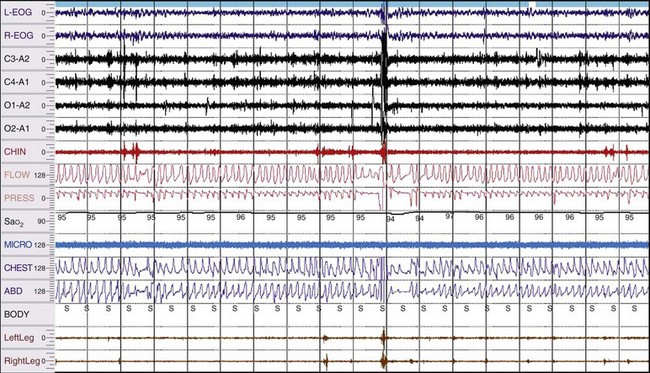
The difference in the sensitivity of pressure transducers (PRESS) and thermocouples (FLOW) is demonstrated in this figure, in which a reduction of the pressure transducer signal to much less than 10% is evident but the reduction in the flow channel is minimal. According to the scoring rules of the American Academy of Sleep Medicine this event does not qualify as either an apnea or a hypopnea because assessment of flow for apneas is supposed to be done by a thermal sensor. This cannot be a hypopnea by the scoring rules because there is only a 1% oxygen desaturation. There is, however, an impressive arousal, including a leg jerk, and it is hard to argue that this event is not significant. This most likely represents an RERA, but it does not meet scoring criteria for RERA either. The current rules define RERA as “a sequence of breaths lasting at least 10 seconds characterized by increasing respiratory effort or flattening of the nasal pressure waveform leading to an arousal from sleep when the sequence of breaths does not meet criteria for an apnea or hypopnea.” However, the scoring manual calls for use of an esophageal pressure manometer or respiratory inductance plethysmography to assess respiratory effort, but these devices are not commonly used in clinical practice.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sleep Breathing Disorders
Only gold members can continue reading. Log In or Register to continue