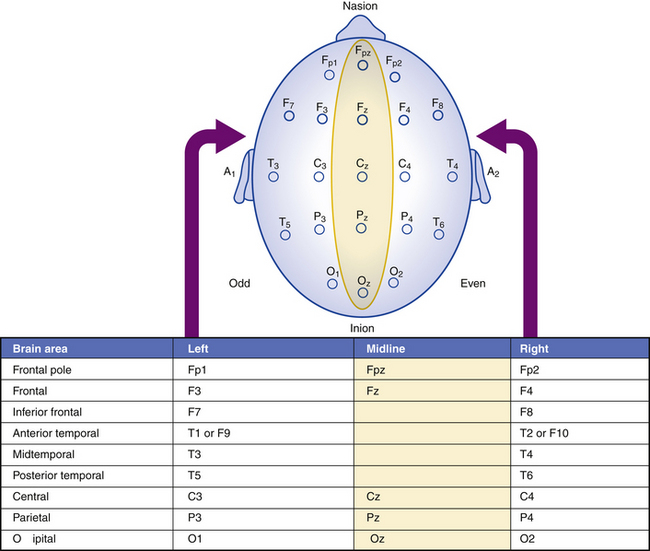
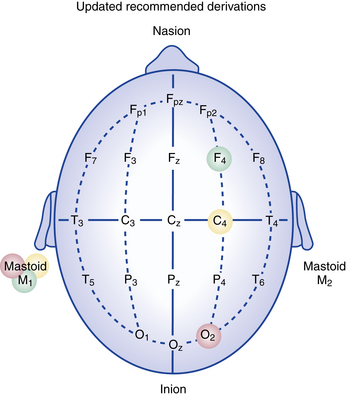
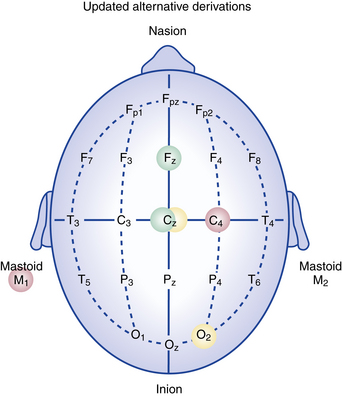
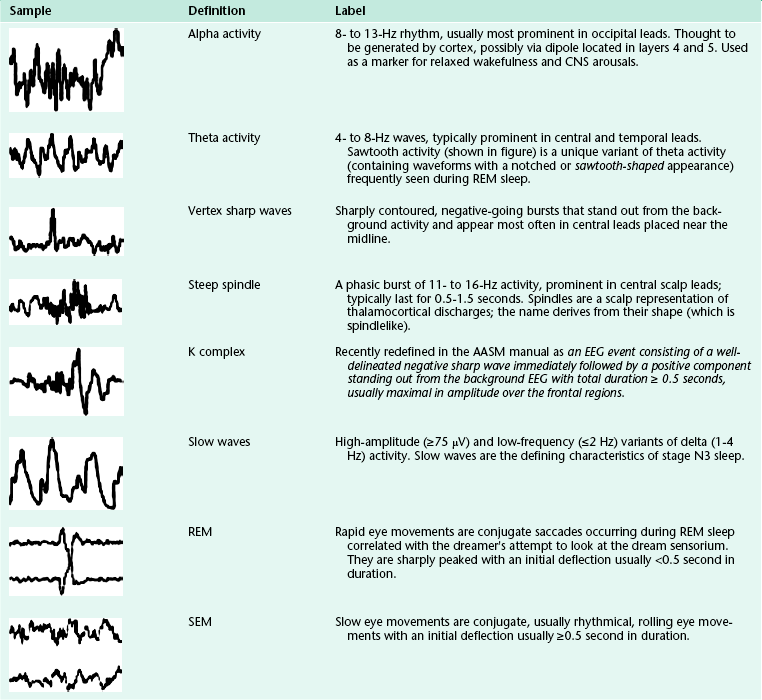
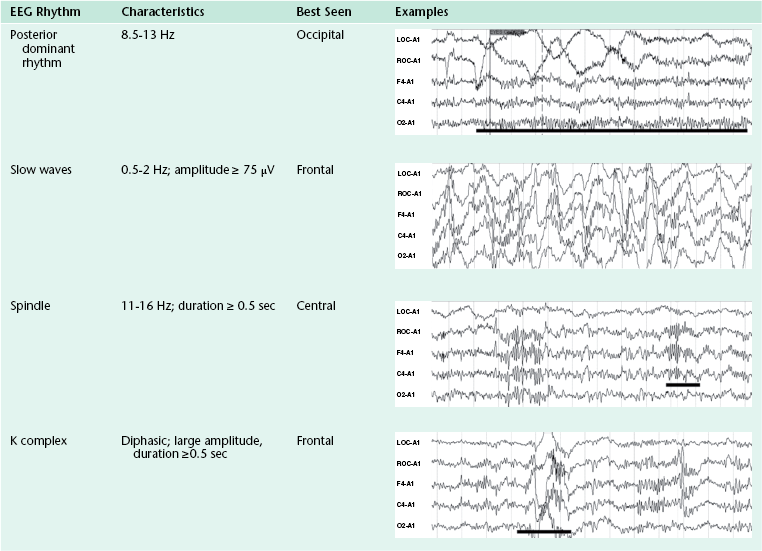
Chapter 3 Particular signals of interest for sleep scoring include those generated from the cerebral cortex (electroencephalogram [EEG]), eye movements (electro-oculogram [EOG]), and the muscles of the face (picked up by chin electromyographic activity). Electrode placement for EEG scoring rules follows the international 10-20 system, which assigns a number to each EEG electrode to specify the location in the left or right hemisphere (Table 3.1). Table 3.1 10-20 Electrode Placement Figures 3.1 and 3.2 depict the updated AASM-recommended derivations for recording the EEG. FIGURE 3.1 Updated American Academy of Sleep Medicine (AASM) recommended derivations for recording the electroencephalogram. Electrode locations as recommended in 2007 by the AASM. (Modified from Kryger MH. Atlas of Clinical Sleep Medicine. Philadelphia: Saunders/Elsevier; 2010.) FIGURE 3.2 Updated American Academy of Sleep Medicine alternative derivations for recording the electroencephalogram. Alternative electrode locations as recommended in 2007. Backup electrode substitutions: O1 for Oz, Fpz for Fz, and C3 for Cz. Fp, Frontopolar or prefrontal; F, frontal; C, central; T, temporal; P, parietal; O, occipital; A, ear or mastoid; F3, left midfrontal; P3, left parietal; T4, right temporal; A1, right ear; Cz, vertex. (Modified from Kryger MH. Atlas of Clinical Sleep Medicine. Philadelphia: Saunders/Elsevier; 2010.) The following abbreviations are used in the PSG samples provided in this chapter: Electro-oculogram electrodes (EOG): Left outer canthus: LOC-A2; right outer canthus: ROC-A1; LOC-A2, ROC-A1, left and right electro-oculogram referred to right and left mastoid leads; M2, right mastoid electrode location; M1, left mastoid electrode location; L/ROC-AVG, left and right electro-oculogram referred to an average reference electrode; E1, left outer canthus eye electrode; E2, right outer canthus eye electrode. Electroencephalogram electrodes (EEG): C3-A2, C4-A1, O1-A2, O2-A1, left central, right central, left occipital, right occipital; electrode location: ground (FPZ), reference (CZ), A1 or M1 and A2 or M2; C3 and O1, left central and occipital, respectively, EEG electrodes; C4 and O2, right central and occipital, respectively, EEG electrodes. The exploring reference electrode (F3, F4, C3, C4, O1, and O2) is chosen on the opposite side of the head from the mastoid electrode (M1, M2) or average (AVG). Electromyogram electrodes (EMG): LtTib1-LtTib2 and RtTib1-RtTib2, left and right tibialis anterior EMG electrodes; Chin1-Chin2, submental EMG signal; chin EMG, Chin1-Chin2; limb EMG (left leg, right leg), LtTib1-LtTib2, RtTib1-RtTib2. Electrocardiogram electrodes (ECG): ECG1-ECG2, ECG2-ECG3. Respiratory electrodes: SNORE, snore sensor sound; OroNs, oronasal airflow or oronasal thermistor; PFLOW, nasal pressure transducer; THOR/CHEST and ABD, chest and abdominal walls motion effort; THOR1-THOR2, thoracic effort channel; ABD1-ABD2, abdominal effort channel; CFLOW, continuous positive airway pressure (CPAP) airflow channel; PCO2, mm Hg of carbon dioxide; SpO2, oxygen saturation by pulse oximetry by finger probe; Pleth, plethysmography; Pt Position, patient position (supine, left, right, prone). Common to all PSG monitoring is the measure of the following three physiological parameters: The EOG signals measure changes in the electrical potential of the positive anterior aspect of the eye, the cornea, relative to the negative posterior aspect, the retina. Horizontal axis electrodes are placed near the outer canthi and vertical axis electrodes 1 cm below (LOC) and 1 cm above (ROC) the eye to measure transient changes in potential during the actual eye movement (Fig. 3.3). During any eye movement the cornea moves toward one electrode, while the retina moves away. When the eye is not moving, the change in relative position is zero, and the eye leads do not record a signal. FIGURE 3.3 The eye can be envisioned as a battery with the positive pole at the cornea and the negative pole at the retina. The electro-oculogram (EOG) consists of a bipolar linkage from the right electro-oculogram (ROC) electrode 1 cm lateral and 1 cm superior to one outer canthus to the left electro-oculogram (LOC) electrode 1 cm lateral and 1 cm inferior to the other outer canthus. The electrode toward which the eyes move becomes relatively positive, the other relatively negative. As the eyes move during sleep, they produce corresponding changes in the electrical field, producing a correlating potential change in the electroencephalogram electrodes. This can be verified by noting corresponding movements in the EOG channels. (From Avidan AY, Barkoukis T, eds. Review of Sleep Medicine. 3rd ed. Philadelphia: Elsevier; 2011.) • EOG voltages are higher than EEG signal. Because the eye is outside of the skull structure, there is no bone to attenuate signal. • The cornea (front) has a positive polarity. The retina (back) has a negative polarity. • EOG placement (LOC and ROC) is on the outer canthus of the eye, offset 1 cm below (LOC) and 1 cm above (ROC) the horizon. • Electro-oculography picks up the inherent voltage of the eye. During eyes-open wakefulness, sharp deflections in the EOG tracing may indicate the presence of eye blinks. The EMG signals are muscle twitch potentials, which are used in PSG to distinguish between sleep stages based on the fact that EMG activity diminishes during sleep. Specifically, during REM sleep, muscle activity is minimal. Compounding the problem of interpreting EMG channels is occasional intrusion of EMG artifact into the record. Some of these intrusions are in the form of yawns, swallows, and teeth grinding (bruxism). • Mental (mentalis muscle) and submental (mylohyoid and anterior belly of the digastrics muscle) placements are acceptable. • These are used to detect muscle tone changes for scoring REM versus NREM sleep. • Muscle tone is high during wakefulness and NREM sleep. It is lower in NREM sleep than in wakefulness. It is generally lower in slow wave sleep then in stage N1 or N2. Six EEG wave patterns are used to differentiate wake and sleep states and classify sleep stages: (1) alpha activity, (2) theta activity, (3) vertex sharp waves, (4) sleep spindles, (5) K complexes, and (6) slow wave activity. These are summarized in Tables 3.2 and 3.3. Table 3.2 Sleep Electroencephalographic Waveforms Modified from Kryger MH. Atlas of Clinical Sleep Medicine. Philadelphia: Saunders/Elsevier; 2010. Table 3.3 Definitions and Examples of Sleep Figures Encountered on an Electroencephalogram Modified from Vaughn BV, Giallanza P. Technical review of polysomnography. Chest. 2008;134:1310-1319. Cortical activity can be characterized by specific frequencies. Frequency is defined as the number of times a repetitive wave recurs in a specific time period (typically 1 second). Frequency is noted as cycles per second (i.e., Hertz [Hz]). EEG activity has been divided into four bands based on the frequency and amplitude of the waveform, and the bands are assigned Greek letters (alpha, beta, theta, and delta). The EEG frequencies are defined slightly differently according to the reference used. The following convention is used to define EEG frequencies: beta is greater than 13 Hz; alpha is between 8 and 13 Hz; theta is between 4 and less than 8 Hz, and delta is the slowest activity at less than 4 Hz. Another EEG activity is gamma, which ranges from 30 to 45 Hz. • Beta EEG is defined as a waveform between 14 and 30 Hz but is usually between 18 and 25 Hz. • It originates in the frontal and central regions but can also occur more diffusely. • It is present during wakefulness and drowsiness. • It may be more persistent during drowsiness, diminish during deeper sleep, and reemerge during REM sleep. • The amplitude over the two hemispheres should not vary by more than 50%. • Enhanced or persistent activity suggests use of sedative-hypnotic medications. • It is also known as posterior dominant rhythm. • It originates in the parietooccipital regions bilaterally. • A normal alpha rhythm is synchronous and symmetrical over the cerebral hemispheres. • It is seen during quiet alertness with eyes closed. • Eye opening causes the alpha waves to “react” or decrease in amplitude. • It has a sinusoidal appearance. • Delta activity has a frequency of 0.5 to 2 Hz for the purpose of sleep scoring. • It is seen predominantly in the frontal region. • Delta activity has an amplitude criterion of 75μV or greater.
Sleep Stages and Scoring Technique
Introduction to Sleep Stage Scoring
The 10-20 system assigns a number to further specify the location in the left or right hemisphere. Location z is used to indicate that the location of the electrode is in the midline or “zero,” meaning that it is neither left hemisphere nor right hemisphere. The electrode placed at Cz is said to be the vertex, meaning that it is the midcentral or at the top of the head. Fpz and Oz are used in achieving the other measurements and can be used as additional electrode placements for localization of activity. Fpz may be used as the location of the common or ground electrode placement.
Parameters for Staging Human Sleep
Eye Movements (Electro-oculogram Activity)
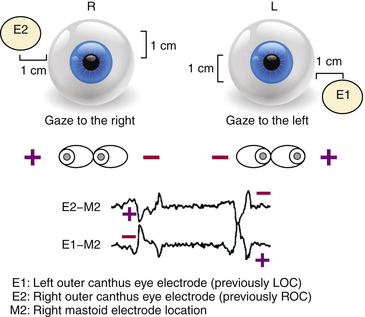
Electro-oculographic Recording
Electromyographic Recording
Submental Electromyographic Recording Criteria
Electroencephalographic Activity During Wakefulness and Sleep
Please note that although all slow waves are in the delta frequency range, not all delta waves are slow waves.
Beta Activity
Alpha Activity (see Table 3.3)
Delta Activity (see Table 3.3)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Sleep Stages and Scoring Technique
Only gold members can continue reading. Log In or Register to continue






