Solitary Hyperdense Parenchymal Lesion
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Cerebral Contusion
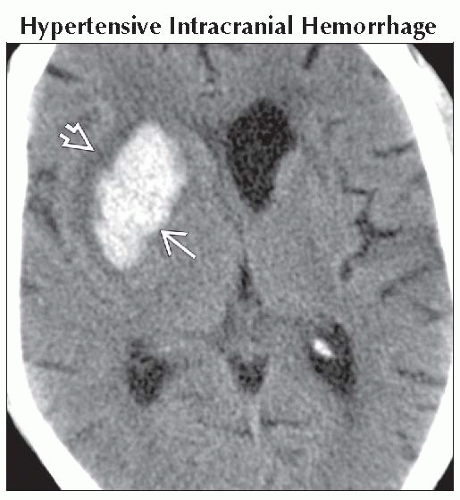
Hypertensive Intracranial Hemorrhage
Cerebral Amyloid Disease
Glioblastoma Multiforme
Metastasis, Parenchymal
Thrombosis, Dural Sinus
Thrombosis, Cortical Venous
Less Common
Cavernous Malformation
Developmental Venous Anomaly
Arteriovenous Malformation
Medulloblastoma (PNET-MB)
Ependymoma, Supratentorial
Melanoma
Ganglioglioma
Lymphoma, Primary CNS
Germinoma
Anaplastic Oligodendroglioma
Rare but Important
Drug Abuse
Tuberculoma
Neurosarcoid
Leukemia
Tuberous Sclerosis Complex
Meningioangiomatosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Hyperdense parenchymal lesions
↑ Attenuation compared to normal brain
Caused by
Clotted blood (most common)
Nonhemorrhagic hypercellular (electron dense) mass (less common)
Calcification (excluded here)
History essential
Age
Trauma, hypertension, drug abuse, dementia, known extracranial primary neoplasm
Sudden onset vs. subacute/chronic
Helpful Clues for Common Diagnoses
Cerebral Contusion
Trauma
Location important
Cortex, subcortical white matter
Anterior inferior frontal, temporal lobes most common
Multiple > > solitary lesion
Evolves over time; 24-48 hours existing lesion may enlarge, become more hemorrhagic
Hypertensive Intracranial Hemorrhage
Older hypertensive patient
Location important
Deep > superficial lesion
Nearly 2/3 striatocapsular
Thalamus 15-25%
Look for multifocal “microbleeds”
1-5%
Best seen on T2* MR
Cerebral Amyloid Disease
Causes 15-20% of all “spontaneous” intracranial hemorrhages (ICHs) in normotensive elderly patients
Classic = lobar hemorrhage (vs. basal ganglia in hypertension)
Look for “microbleeds” (do T2* MR)
Cortical/subcortical vs. basal ganglia, cerebellum (chronic hypertension)
Glioblastoma Multiforme
Necrosis, hemorrhage common
Metastasis, Parenchymal
Can be hemorrhagic or nonhemorrhagic
Hypercellular, electron dense nonhemorrhagic metastases
Thrombosis, Dural Sinus
Multifocal > solitary hemorrhage
Parenchymal clot(s) adjacent to dural sinus (transverse sinus > superior sagittal sinus)
Thrombosis, Cortical Venous
Multifocal > solitary hemorrhage
Can occur with or without dural sinus occlusion
Helpful Clues for Less Common Diagnoses
Cavernous Malformation
Variable presentation
Acute hemorrhage
Common cause of spontaneous ICH in children, young adults
Epilepsy
Hyperdense calcified or noncalcified parenchymal mass
Developmental Venous Anomaly
Hemorrhage rare unless mixed with cavernous malformation
Blood in transcortical draining vein slightly hyperdense to brain
Arteriovenous Malformation
Common cause of spontaneous ICH in children, young adults
Rupture of intranidal aneurysm, stenosis/occlusion of draining veins
Medulloblastoma (PNET-MB)
Electron dense tumor with high nuclear: cytoplasm ratio
Midline hyperdense posterior fossa mass in child? Suspect PNET-MB
Lateral (cerebellar) mass in older child/young adult? Suspect desmoplastic variant of medulloblastoma
Ependymoma, Supratentorial
Most ependymomas are intraventricular, but up to 40% are supratentorial, parenchymal > intraventricular
Large hyperdense calcified solid/cystic hemispheric tumor in young child? Think ependymoma!
Melanoma
Metastatic > primary CNS melanotic lesion
Melanin or hemorrhage → ↑ density
Ganglioglioma
Child/young adult with epilepsy
Most are partially cystic, contain Ca++
Lymphoma, Primary CNS
Corpus callosum, basal ganglia
Hemorrhage rare unless HIV/AIDS
Germinoma
Pineal > infundibulum > basal ganglia
Densely cellular tumor but may also hemorrhage
Hyperdense basal ganglia mass in child/young adult? Think germinoma!
Anaplastic Oligodendroglioma
Mixed density common
May Ca++, hemorrhage
Helpful Clues for Rare Diagnoses
Drug Abuse
Striatocapsular hemorrhage in young/middle-aged adult? Consider drug abuse
Tuberculoma
Granuloma mildly hyperdense
Can mimic intra- or extra-axial neoplasm
Neurosarcoid
Multifocal > solitary
Extra-axial > parenchymal mass(es)
Leukemia
Extra-axial > intra-axial lesion
Hyperdense parenchymal lesion can be hemorrhagic complication (more common) or chloroma (less common)
Tuberous Sclerosis Complex
Cortical, subcortical tubers can be hyperdense &/or calcified
Multifocal > solitary
Solitary large, “lobar-type” hyperdense tuber ± Ca++ can mimic neoplasm
Meningioangiomatosis
Cortical-based, gyriform hyperdensity
May be densely calcified
Can mimic neoplasm!
Image Gallery
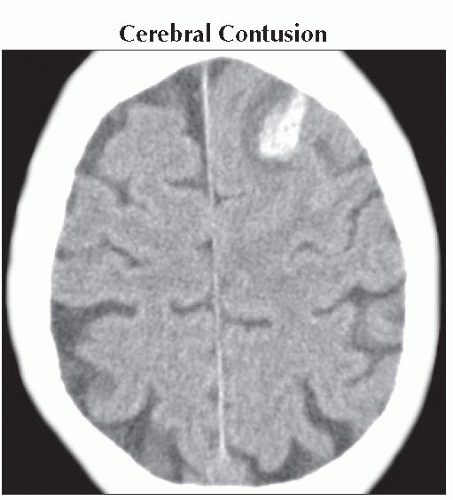 Axial NECT shows a left frontal hyperdensity with surrounding hypodensity, typical of cortical contusion. Note effaced frontal sulci from focal mass effect. |
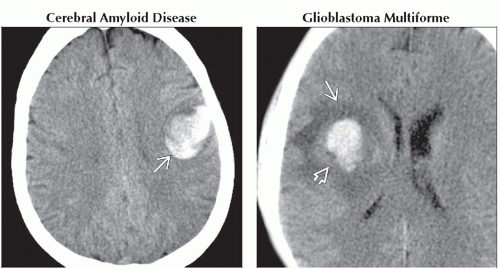 (Left) Axial NECT shows focal lobar hematoma
 in a 68 yo normotensive, mildly demented patient with sudden onset of right-sided weakness. T2* MR scan showed multifocal peripheral “black dots” characteristic of amyloid angiopathy. (Right) Axial NECT shows inhomogeneously hyperdense hematoma in a 68 yo normotensive, mildly demented patient with sudden onset of right-sided weakness. T2* MR scan showed multifocal peripheral “black dots” characteristic of amyloid angiopathy. (Right) Axial NECT shows inhomogeneously hyperdense hematoma  surrounded by edema surrounded by edema  . MR showed thick, irregular enhancing rind of tissue. Surgery disclosed GBM with intralesional hemorrhage of different ages. . MR showed thick, irregular enhancing rind of tissue. Surgery disclosed GBM with intralesional hemorrhage of different ages.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|