Solitary Parenchymal Calcification
Anne G. Osborn, MD, FACR
DIFFERENTIAL DIAGNOSIS
Common
Neurocysticercosis
Tuberculosis
Cavernous Malformation
Oligodendroglioma
Ganglioglioma
Diffuse Astrocytoma, Low Grade
Pilocytic Astrocytoma
Less Common
Arteriovenous Malformation
Ependymoma
Parasites, Miscellaneous
Rare but Important
Physiologic Calcification, Brain
“Brain Rock”
Calcified Embolus
Saccular Aneurysm
Metastasis, Parenchymal
TORCH Infection
DNET
Meningioangiomatosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Solitary brain calcification includes
True parenchymal calcification
Some lesions that may look like they are in brain itself but are not actually in parenchyma
Lesion in deep sulcus (neurocysticercus cyst)
Lesion in vessel (calcified embolus, saccular aneurysm)
Key question: Is Ca++ solitary focus or are there multiple calcified foci in solitary mass-like lesion?
Solitary “dot-like” or globular Ca++
Typically infectious (neurocysticercosis, TB, occasionally other rare parasites)
Less common
Physiologic (habenular commissure, unilateral basal ganglia)
Vascular (AVM, cavernous malformation, Ca++ embolus)
Rare = brain “rock”
Solitary mass-like lesion with clustered Ca++
Neoplasm (many)
Cavernous malformation
Helpful Clues for Common Diagnoses
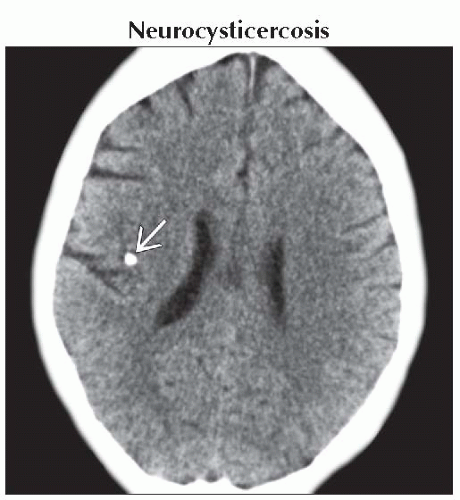
Neurocysticercosis
Nodular calcified (healed) stage
Multiple (“starry sky”) > solitary lesions
Most NCC cysts are actually cisternal (within depths of superficial sulci) > brain parenchyma, ventricles
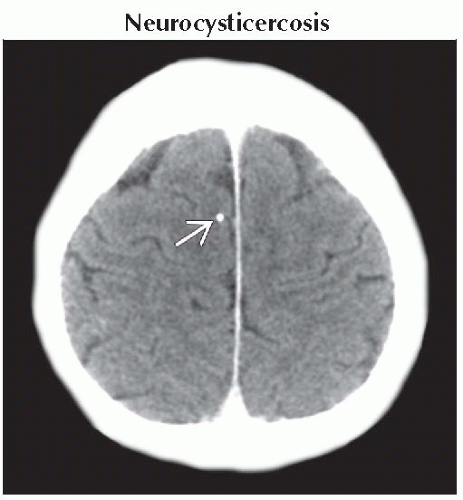
Tuberculosis
Healed granuloma
Can be single or multiple
Many fewer lesions than NCC
Occasionally solitary tuberculoma can be mass-like, mimic neoplasm
Cavernous Malformation
Solitary > multiple
Ca++ can be dot-like, clumped, or scattered within single lesion
Do MR with T2* scan (GRE, SWI) to look for hemorrhage, multiplicity
Oligodendroglioma
Cortical/subcortical mass
Slow-growing; may erode adjacent skull
70-90% calcify (nodular, clumped)
Adult > child
Ganglioglioma
Slow-growing, cortically based neoplasm
Child/young adult with epilepsy
Common: Ca++ nodule, ± cysts
May erode/remodel adjacent skull
Diffuse Astrocytoma, Low Grade
Hemispheres > posterior fossa
Solid > > cystic mass
10-20% calcify
Infiltrates brain
Intrinsic tendency to undergo malignant degeneration
Pilocytic Astrocytoma
Cerebellum > optic nerve/chiasm, 3rd ventricle > pons
Cyst with nodule (cerebellum)
Solid mass (optic chiasm/hypothalamus, pons)
Ca++, hemorrhage uncommon (unless pilomyxoid variant)
Helpful Clues for Less Common Diagnoses
Arteriovenous Malformation
Little/no mass effect unless hemorrhage
Look for enlarged feeding arteries, draining veins
Occasional Ca++ in nidus, draining veins (phlebolith)
Ependymoma
3rd most common posterior fossa neoplasm in children (after medulloblastoma, pilocytic astrocytoma)
2/3 infratentorial (4th ventricle)
1/3 supratentorial (extra-ventricular, hemispheric WM)
Large, extensively calcified cystic/solid hemispheric mass in young child? Think ependymoma first!
50% of all ependymomas calcify
Cysts, hemorrhage also common
Parasites, Miscellaneous
Except NCC, parenchymal Ca++ rare
Any healed parasitic infection can calcify
Helpful Clues for Rare Diagnoses
Physiologic Calcification, Brain
True solitary, unilateral normal parenchymal Ca++ unusual
Basal ganglia usually bilateral, occasionally unilateral
Habenular commissure may Ca++
“Brain Rock”
Dense globular parenchymal Ca++
No infection, neoplasm, degeneration
Calcified Embolus
In artery within sulcus, not brain parenchyma
Saccular Aneurysm
Huge, bizarre-appearing, extensively calcified mass in adult? Think partial/completely thrombosed giant saccular aneurysm
Metastasis, Parenchymal
Untreated metastases rarely calcify
Breast, mucinous carcinoma, osteosarcoma metastasis may calcify spontaneously
TORCH Infection
Multiple > > solitary
CMV most common
Cortical
DNET
Almost all patients < 20 years
Chronic epilepsy
Well-delineated, “bubbly” appearing cortical mass
May remodel overlying skull
Gross Ca++ uncommon, hemorrhage rare
< 20% enhance
May have adjacent cortical dysplasia
Meningioangiomatosis
Child/young adult with seizures
Hamartomatous cortical/leptomeningeal malformation
Meningovascular proliferation along perivascular spaces (PVSs)
50% associated with neurofibromatosis
Cortical mass with Ca++ (often gyriform)
T2 hypointense
Plaque-like pial, linear enhancement along PVSs
Image Gallery
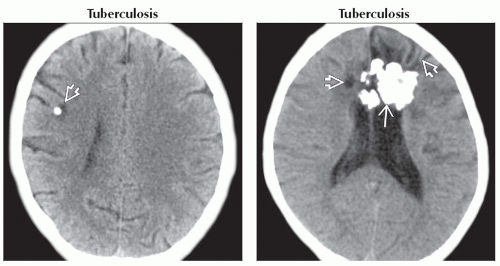 (Left) Axial NECT in patient with known TB shows parenchymal calcification
 with surrounding hypodensity, characteristic of healed caseating granuloma. (Right) Axial NECT shows large bifrontal densely calcified lesion with surrounding hypodensity, characteristic of healed caseating granuloma. (Right) Axial NECT shows large bifrontal densely calcified lesion  without mass effect. Note encephalomalacia without mass effect. Note encephalomalacia  in adjacent parenchyma. Solitary tuberculoma was found at surgery. in adjacent parenchyma. Solitary tuberculoma was found at surgery.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|