Specific Aspects of Spinal Tumors and Traumatisms in Children
Andre J. Kaelin
INTRODUCTION
Spinal tumors and traumatisms are specific in infancy, childhood, and adolescence. The main factor during this period of life is the remaining growth, but etiologies, mechanisms of lesions, types of lesions, and outcomes are very different. In adulthood, most of the spinal tumors are secondary locations or metastases; in young patients, those lesions represent a very large differential diagnosis of primary benign and malign tumors. Spinal cord plasticity allows important tumor development before triggering neurologic deficit; pain, back stiffness, and hamstring tightness are often the initial complaints.
If the mechanism of trauma involves high energy, complete imaging is usually performed, and obvious bone fractures are detected. In childhood, spinal lesions can occur after very low energy trauma, because of bone pathologic or constitutional fragility, delaying diagnosis; pain, back stiffness, and hamstring tightness are again the only symptoms. In case of nonresolving back pain in children, tumor and trauma lesion must be ruled out. We describe only the specific aspects of the care process in tumor and spine trauma in the immature spine. The indications for treatments are described, but techniques of treatments that are mostly the same as those in adults are not addressed.
SPINAL GROWTH
At birth, the mean sitting height measures 35 cm; at the end of growth, this parameter measures 88 cm for girls and 92 cm for boys. The length of the thoracic and lumbar spine is 20 cm at birth and 45 cm at maturity. These 25 cm of growth are shared by 34 apophyseal zones located cranial and caudal to each vertebral body for the anterior spine. In the posterior, a very complex system of apophyseal growth cartilage is situated on the spinous processes, the transverses processes, and the joints.
The neurocentral cartilage increases the size of the medullary canal. It stops its action around the age of 6 years old, and it is the first growth cartilage to ossify.
Balanced growth between the anterior and posterior and the right and left parts of the spine are necessary for keeping a normal morphology. The earlier a growth imbalance occurs, the greater are the risks of deformities. During the first year of life, we see the larger increase, 12.4 cm, and then the growth slows progressively in 3 years to 2.3 cm. At puberty (14 to 15 years for boys, and 12 to 13 years for the girls), the speed increases again at 4 cm per year for 2 years.
The remaining growth for boys at 5 years old is 9.3 cm in the thoracic area and 5.6 cm in the lumbar area; at 10 years old, 6 cm in the thoracic area and 3.6 cm in the lumbar area. For girls at 5 years old, the growth is 7.8 cm in the thoracic area and 4.7 cm in the lumbar area; at 10 years old, 4.2 cm in the thoracic area and 2.5 cm in the lumbar area.
At birth, the spine is very flexible because of the ligamentous laxity, but ligaments are still stronger than bone. In addition, because of the muscular hypotonia; poor active and passive spinal cord protection exists. Progressively, stability increases, and tone increases to the adult standard at the end of puberty.
At birth more than 50% of vertebral bodies are cartilaginous and very soft; ossification reaches the body limit when the child is prone to stand, giving mechanical support.
The morphology of the vertebral plateau is unique; it acts as articular surface and apophyseal growth plate (no epiphyseal nucleus is present). In the limbus area during puberty, a ring apophysis appears with an ossifying nucleus that represents a weak point in the vertebral stability.
The mineral content in children is as low as that in elderly people. Mineralization builds up to a peak in young adulthood, which is why low-energy trauma causes fractures so easily in children.
Posture and the repartition of body weight changes during growth. For the first months, the baby is unable to support its trunk; the head is not actively controlled. Sitting is possible once head control is acquired, but the spine is in global kyphosis. After the acquisition of erect position, the definitive spinal morphology with lumbar lordosis, thoracic kyphosis, and cervical lordosis is obtained after walking.
At birth, the head weight is 25% of the total body weight. This proportion decreases to 5.6% for an adult; heavy heads and weak cervical muscles explain the high risk to the cervical spine in infancy and childhood.
SPINE TRAUMA IN CHILDREN
Patients to the age of 18 years represent 20% of the population, but only 3% of spinal fractures occur in children, which is very low. In a survey in our hospital, the mean age is 11 years old, with two peaks at 9 and 12 years old. Of our patients, 44% have one-level fractures; 20%, two levels; 19%, three levels; and 17%, four levels and more. Most of the time, levels are contiguous. One-level fractures occur mainly in the cervical or lumbar area, and the multilevel fractures in the thoracic area. In 87 cases, the most common level is T6 (30 cases); 84% are wedges and stable fractures, and 16% are burst or combined fracture/dislocation. One patient is definitively paraplegic; one has a regressive nerve root deficit, and two died of polytrauma. Of our patients, 62% were treated functionally (rest, analgesic medication, physical therapy), 26% received also a brace for up to a year; and 12% were treated surgically (cervical, three; thoracic, two; lumbar, three), mainly with a posterior approach.
The etiologies of fractures during the growth period are very different from those in the young adult; each age period has a specific mechanism.
For neonates and young infants, spinal fracture and dislocation are very often associated with head injury; for all unconscious patients, not only cervical but also thoracic and lumbar fractures must be ruled out.
Newborn: Spinal Fractures
Prenatal fracture secondary to osteogenesis imperfecta in association with limbs, ribs, and skull fractures.
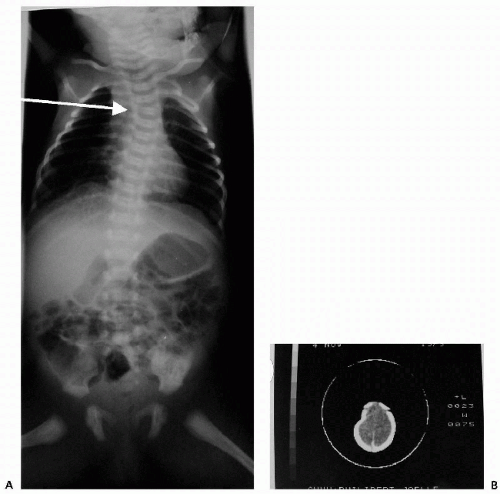
Birth trauma (fetomaternal dystocia or emergency delivery due to fetal distress) associated with shoulder or brachial plexus injury or both (Fig. 3.1)
Infant: Spinal Fractures
Fall from low height
Deceleration traction trauma in cervical and high-thoracic area (Fig. 3.2) (baby installed in a baby seat with four-point fixation), in low thoracic and lumbar area (baby installed in a baby seat with abdominal seat belt)
High-energy polytrauma (car accident)
Battered-baby syndrome (association with head, limbs, skin lesion)
Children: Spinal Fractures
Street trauma
Playground accident
Sports accident
High-height fall
Adolescents: Spinal Fractures
Sports accident
Motor vehicle accident
The type of trauma and the morphology of children’s spines lead to specific lesions.
1. SCIWORA (Spinal Cord Injury Without Radiographic Abnormalities) is rare for children younger than 8 years. Very important flexion/extension movement or axial traction on the hyperlaxe cervical spine causes a direct spinal cord lesion or ischemic lesion. Complete or partial paraplegia appears immediately or could be delayed by some hours. Radiographs and computed tomography (CT) scan are normal. If no magnetic resonance imaging (MRI) modification is found, the outcome is very good; if the MRI shows edema or a hemorrhage, the risk of permanent lesion is high. Rest and immobilization of the cervical spine give a better chance of neurologic recovery.