Spinal Cord Disorders
A. Acute cord compression is an emergency
Consider this in any pt with rapidly progressive spinal cord sx, especially of bladder or bowel.
1. Exams: Rectal sensory and motor exam, emergent spinal MRI. Do whole spine if cancer suspected.
2. Rx: Consider dexamethasone 100 mg IV push or the methylprednisolone protocol available in most ERs, stat neurosurgery consult, or XRT. Goal is to prevent progression, although deficit can sometimes reverse if it is of recent onset.
3. Blood pressure: Very labile with cord lesions, especially during pain. Overtreating BP (e.g., with nifedipine) can cause hypotension.
4. Cervical cord contusion: High-dose steroids, hard collar unless cervical instability already ruled out with C-spine x-ray (but do not flex/extend if there is a known cord contusion).
B. Pts with back pain and known cancer
Assume cord compression until proven otherwise. see p. 117 for workup.
C. Terminology
1. Bone problems: Spondylosis = degeneration. “Cervical spondylosis” sometimes used as synonym for “stenosis.” Spondylolisthesis = anterior subluxation. Spondylolysis = isthmic spondylolisthesis.
2. Cord problems: Myelopathy and myelitis are spinal cord damage and inflammation, respectively. Cf. myopathy and myositis, which are muscle conditions.
D. History
Radiation of pain, triggers, numbness, weakness, incontinence, weight loss, IVDA, DM, previous surgery, trauma, litigation, degree of disability, assoc. depression. With neck pain, ask about chest pain, shortness of breath, radiation to jaw.
1. Location: Thoracic level suggests metastases.
2. Character: Burning, electric, aching.
3. Precipitants: Walking, sitting, squatting, leaning forward, coughing, time of day.
4. Bladder changes: Frequency, urgency, sensation during voiding, sexual function.
a. UMN lesion: Bladder stretch reflex is disinhibited and spastic, so small bladder and frequent voids.
b. LMN lesion: Retention, sometimes with retention overflow.
E. Exam
Document exam carefully, especially if pt. going to OR, to record presurgical deficit.
1. Reflexes: Spread, finger flexors, Hoffman’s, crossed adductors, clonus, Babinski, abdominals.
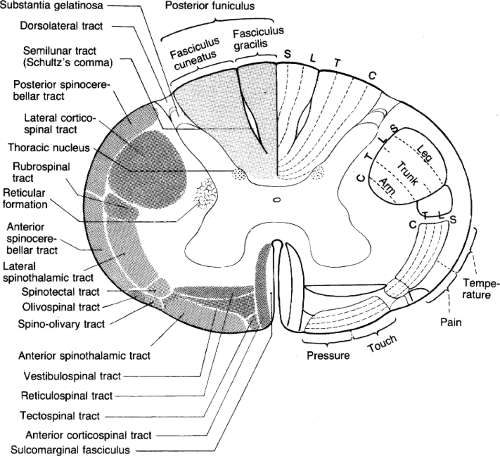
Figure 12. The spinal cord in cross-section. (Reprinted with permission from Duus P. Topical Diagnosis in Neurology. New York: Thieme; 1983: 49.)
2. Straight leg raise (SLR): For L5, S1 irritation. Pain during reverse SLR (extension) suggests L3 or L4 irritation. Pain on palpation, range of motion, posture (anthropoid in stenosis), abdominal reflexes, clonus, pulses, atrophy, fasciculations, café-au-lait spots, Lhermitte’s sign.
3. FABER (Flex-ABduct-Extend-Rotate): Put ankle on opposite knee; rotate knee towards exam table. Positive for hip dz and mechanical low back pain, but not for disc dz.
4. Hysterical back pain: If pain on simulated axial loading (push top of head), or if cannot tolerate straight leg raise, but can sit/put socks on.
5. Bowel/bladder: Prostate, bulbocavernosus (finger in rectum, pull on penis or bladder catheter), cremaster, anal wink, percuss bladder, measure postvoid residual (if residual >100 cc, leave catheter in). Any abnormality may be indication for emergent MRI.
6. Sensory lesions: Look for sensory level, dissociation of sensory modalities. Pinprick is lost first (vs. peripheral nerve injury, where light touch is lost first). See Sensory Loss, p. 111.





