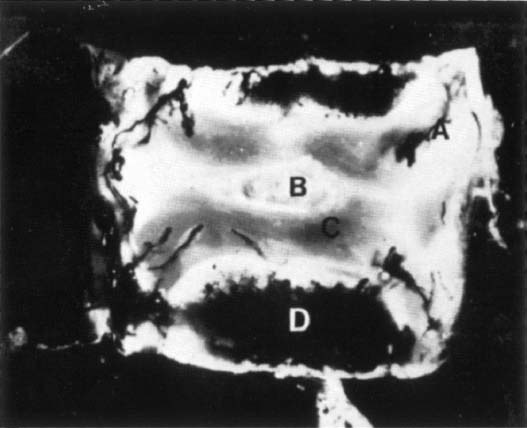
20 I. Incidence/risk factors A. Approximately 2 to 7% of all osteomyelitis (1 to 2% in children) B. Lumbar > thoracic > cervical C. Males > females (2:1) D. More common after the 5th decade (>50% of cases) E. More common in young intravenous drug abusers, diabetics, and immunocompromised (chronic steroids, HIV, malnutrition) II. Etiology A. Hematogenous spread is the most common route for vertebral osteomyelitis. 1. Urinary tract most common source (urinary tract infections, transient bacteremia from genitourinary procedures) 2. Soft tissue infections 3. Respiratory infections B. Unidentified source C. Direct inoculation (penetrating trauma, invasive spinal procedure) D. Causative bacteria (in order of frequency) 1. Gram-positive aerobic cocci (>80%) a. Staphylococcus aureus (>50%) (1) Methicillin-resistant S. aureus (7%) b. Streptococcus (10 to 20%) c. Coagulase-negative staphyloccus (10%) 2. Gram-negative aerobic cocci (15 to 20%) a. Most common origin is from the urinary tract (Escherichia coli, Pseudomonas aeruginosa, Proteus) 3. Gastrointestinal tract organisms a. Salmonella (rare) (1) More common in patients with sickle cell III. Pathology A. Inoculation 1. Hematogenous spread to the vertebral metaphysis most likely occurs via rich arterial anastamosis (nutrient artery) (Fig. 20–1). a. Batson’s valveless venous plexus is not considered to play a significant role in bacterial hematogenous seeding. b. Vertebral metaphysis is a low-flow environment that may allow for the direct spread of bacteria into and across the intervertebral disk. B. Spread to the intervertebral disks 2. Bone/disk destruction (Fig. 20–2) a. Bacteria produce enzymes that digest disk tissue. b. Bone resorption by osteoclasts activated by various inflammatory mediators C. Soft tissue extension 1. Psoas abscess 2. Paraspinal muscle abscess 3. Epidural abscess a. May result in neurological compromise secondary to direct compression of the spinal cord and nerve roots IV. Clinical findings A. Delay in diagnosis is common. B. Back or neck pain is the most common presenting complaint (90%). 1. Symptoms are typically present for more than 3 months in 50% of patients. 2. Acute presentation with septicemia and toxemia extremely rare C. Localized pain and tenderness with a decreased range of motion are the most consistent findings. D. History of fever >100°F (with or without chills) is present in over 50% of patients. E. In children, a limp and refusal to walk are characteristically present. V. Laboratory findings (Table 20–1) VI. Radiographic imaging studies (Table 20–2) VII. Treatment A. Goals 1. Establish a tissue diagnosis and identify the organism. 2. Eradication of the infection 3. Provide long-term pain relief. 4. Prevent or relieve any neurological deficits. 5. Restore spinal stability/alignment. B. Principles 1. Medically optimize the patient a. Nutritional supplementation b. Treat laboratory abnormalities 2. Treat extraspinal sources of infection a. Urinary tract b. Cardiovascular (infected thrombus) c. Gastrointestinal 3. Avoid antibiotic therapy prior to identification of the organism if possible. a. Except in septic patients where broad-spectrum antibiotics are indicated
Spinal Infections
 Vertebral Osteomyelitis
Vertebral Osteomyelitis

| Test | Findings |
| ESR | Elevated at presentation in more than 80% of cases. ESR normalizes in ⅔ of patients adequately treated. |
| WBC | >10,000/mm3 in more than 50% of cases. WBC count has a low sensitivity for diagnosis. |
| CRP | More sensitive and specific than ESR for monitoring postoperative spine infections. |
| Blood cultures | Most useful in children with vertebral pyogenic osteomyelitis. Only positive in ~35% of patients. Reliable in detecting the offending organism. |
| Needle biopsy | False-negative examinations are common when patient is on antibiotics. |
| Open biopsy | Indicated if needle biopsy is negative, nondiagnostic, or both despite high clinical suspicion. Lower false-negative rate than closed biopsy. |
ESR, erythrocyte sedimentation rate; WBC, white blood cell count; CRP, C-reactive protein.
| Imaging Study | Findings |
| Plain radiographs | Findings lag behind clinical presentation (at least 2 weeks from the onset of infection)
|
| Nuclear imaging | Effective as an initial screening tool
Indium-111-labeled leukocyte (white blood cell) scans are not sensitive in the spine
|
| Computed tomography | Best modality for identifying bone destruction |
| Magnetic resonance imaging | Imaging modality of choice for spine infections
Best imaging modality to differentiate infection versus tumor |
4. Antibiotic therapy should be specific to the organism identified.
5. Erythrocyte sedimentation rate (ESR) and C-reactive protein levels are useful to obtain prior to therapy.
a. May be followed as an indication of treatment efficacy.
C. Operative treatment
1. Indications
a. Cases that have failed nonoperative management.
b. Progressive neurological deficit
(1) Due to direct compression from the infection
(2) Due to progressive deformity or instability
c. Abscess or granuloma formation
(1) Antibiotics are ineffective.
d. Intractable pain not responsive to conservative measures
2. Technique
a. Anterior approach is the most useful for vertebral body debridement (corpectomy).
(1) Laminectomy alone for decompression is contraindicated because of the potential for spinal destabilization.
b. Autogenous bone graft is the gold standard for reconstruction (iliac crest, rib, or fibula).
(1) However, autograft-filled titanium cages and cortical strut allograft have demonstrated good clinical results.
c. Thoracic and lumbar vertebral osteomyelitis may be treated by a single posterior approach (debridement and fixation) using an interbody technique.
 Epidural Abscess
Epidural Abscess
I. Etiology
A. Associated with vertebral pyogenic osteomyelitis in 28% of cases
B. S. aureus most common causative organism (~60%)
C. Regional or location frequencies
1. Thoracic (50%)
a. Neurological deficits more common
2. Lumbar (35%)
3. Cervical (14%)
D. Most cases are in adults (rare in children).
1. Postoperative (16%)
II. Clinical presentation
A. Highly variable, leading to misdiagnosis and delayed treatment in >50% of patients
B. Localized spine tenderness more common
C. Nuchal rigidity and other meningeal signs possible
D. With or without neurological deficit
A. ESR elevated in >98% of cases
B. White blood cell count (WBC)—unreliable
C. Magnetic resonance imaging (MRI) is the imaging modality of choice.
1. Intense focal signal on T2.
2. Epidural metastasis and subdural abscess should be considered in the differential.
IV. Treatment
A. Epidural abscess requires urgent surgical attention.
B. Epidural abscess in the presence of a worsening neurological deficit is a surgical emergency.
1. Exceptions
a. May consider nonoperative treatment consisting of antibiotic therapy with close monitoring if surgery would endanger the patient’s life
 Disk Space Infections
Disk Space Infections
I. Epidemiology/etiology
A. May occur as a result of direct inoculation
1. Surgical procedures
a. Discogram
b. Discectomy
c. Intradiscal Electrothermal Therapy
B. Hematogenous spread
1. This is the route most commonly encountered in the pediatric population.
a. Blood supply from the disk is from the surface of the adjacent vertebral bodies.
C. Lumbar spine most commonly involved
II. Clinical findings
A. Typical patient is between 2 and 7 years of age.
1. Patients may not complain of back pain.
2. Limping, refusal to walk, or hip pain may be presenting symptoms.
B. ESR and WBC are elevated.
C. MRI or bone scan are positive early in the disease.
1. Plain radiographs may demonstrate narrowing of the intervertebral space, sclerosis, or bony erosion.
III. Treatment
A. Surgery is rarely indicated or needed.
B. Immobilization with a brace
C. Antibiotic therapy
D. Biopsy indicated if antibiotics are not effective
 Tuberculosis of the Spine
Tuberculosis of the Spine
I. Epidemiology/etiology
A. Most common granulomatous infection in the world
B. Hematogenous spread is the most common source (pulmonary or gastrointestinal infections).
C. Spine is the most common source of skeletal involvement.
1. Most involve the anterior spine.
2. Involvement of adjacent levels from expansion through the disk space
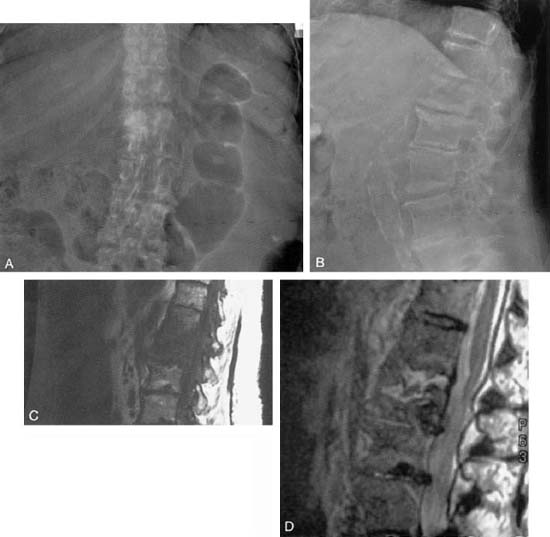
3. Fifty percent of infections are localized and can be categorized (Fig. 20–3).
a. Peridiscal (most common)
(1) Starts in the metaphysis and spreads under the anterior longitudinal ligament
(2) Central (rare)—starts within a single vertebral body
(3) Anterior (rare)—starts under the anterior longitudinal ligament
II. Clinical presentation/diagnosis
A. Pain present with evidence of systemic illness
1. Fevers, malaise, and weight loss
B. Local tenderness, muscle spasm, and limited range of motion
C. Tissue biopsy can by difficult because of the long incubation period for mycobacterium.
1. Fifty percent false-negative rate
D. Differential diagnosis
1. Neoplasms
2. Sarcoidosis
3. Charcot spine
III. Radiological evaluation
A. MRI is the modality of choice.
1. Unique characteristics of tuberculosis versus pyogenic infections
a. Disk space often spared
b. Involvement of anterior bodies over contiguous segments
c. Paraspinal abscesses and granulomas distinguished with the use of gadolinium
IV. Surgical treatment (Fig. 20–4)
A. The Hong Kong procedure
1. Anterior approach for anterior pathology
2. Radical debridement and removal of all necrotic tissue
3. Strut graft/fusion using autograft or allograft restoring anterior column support
4. Posteriorly supplemented instrumentation in more than two levels anteriorly
B. Laminectomy alone is contraindicated.









