Fig. 12.1
Classification of occipital condyle fractures according to Jeanneret and Anderson and Montesano: (a) Jeanneret type I (Anderson and Montesano type II) fracture is part of a transverse fracture of the petrosal part of the temporal bone. (b) Jeanneret type II is a ring fracture of the cranial base. (c) Jeanneret type III (Anderson and Montesano type I) is a compression fracture of the occipital condyle. (d) Jeanneret type IV (Anderson and Montesano type III) is an avulsion fracture of the alar ligament and is frequently combined with an atlantooccipital dislocation (AOD). Reprinted with permission from Tscherne and Blauth [3]
Type II (Jeanneret). A ring fracture of the cranial base which has only been observed in victims killed in traffic accidents (Fig. 12.1b).
Type III (Jeanneret) = Type I (Anderson and Montesano). This type is a compression fracture of the occipital condyle and usually does not cause a neurological deficit (Fig. 12.1c).
Type IV (Jeanneret) = Type III (Anderson and Montesano). An avulsion fracture of the alar ligament which is frequently (25 % of the cases) combined with an atlantooccipital dislocation (AOD) (Fig. 12.1d).
Therapy. Type I is usually treated with a soft cervical collar until improvement of the symptoms. Types II and III without AOD are treated with a soft cervical collar for 6 weeks. Types II and III with AOD has to be treated surgically with a craniocervical fixation. If a dislocation of the fracture is seen it might also be treated in a halo fixateur.
12.2.2 Atlantoccipital Dislocation (AOD)
AOD is a severe injury which usually results in death at the scene caused by brain stem or upper spinal cord injury or injuries of the carotid or vertebral arteries. Sometimes surviving patients show cranial nerve deficits. AOD is caused by a disruption of the ligaments between the skull base and C1 (alar ligaments, tectorial membrane, anterior and posterior atlanto-occipital membrane). The extent of the ligamentous injury determines the grade of instability. The direction of dislocation of the skull in relation to the atlas determines the type of AOD (according to Harris [5]; Traynelis et al. [6]).
Type I. The skull is dislocated anteriorly. The ventral dislocation is the most common type of AOD with instability in the sagittal plane alone or combined with axial instability (Fig. 12.2a)
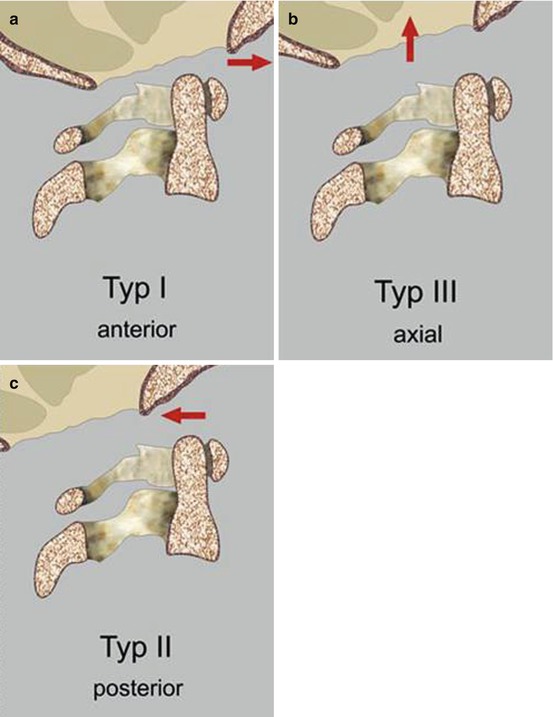
Fig. 12.2
(a) Atlantooccipital dislocation according to Traynelis and Harris. Type I: the skull is dislocated anteriorly (red arrow). (b) Type II (Traynelis), type III (Harris): the skull is dislocated axially (red arrow) – this is the most unstable form of AOD. (c) Type III (Traynelis), type II (Harris): the skull is dislocated posteriorly (red arrow). Reprinted with permission from Kandziora et al. [1].
Type II (Traynelis) = Type III (Harris). The skull is dislocated axially. This is the most unstable form of AOD and is equivalent to a complete separation of the skull from the spine (Fig. 12.2b). There is a high risk of stretch injury of vessels and spinal cord.
AOD is usually diagnosed in a trauma scan. If the patient is stable an MRI of the spine and the skull should be performed to evaluate the brainstem and the brain for infarctions and to give further hints for the prognosis.
Type III (Traynelis) = Type II (Harris). The skull is dislocated posteriorly. Type II is a rare form of AOD (Fig. 12.2c).
Type IV. A lateral dislocation of the skull which was described by Collato and Jevtich.
AOD is usually diagnosed in a trauma scan. If the patient is stable an MRI of the spine and the skull should be performed to evaluate the brainstem and the brain for infarctions and to give further hints for the prognosis.
Therapy. AOD in adults is managed by surgical occipitocervical instrumentation with fusion. In children AOD can alternatively be managed with immobilization in a halo fixateur if a good closed reposition can be achieved. Another treatment possibility in children is a temporary occipitocervical instrumentation without bony fusion. Extension is absolutely contraindicated.
12.3 Upper Cervical Spine
12.3.1 Atlas Fractures
Fractures of the atlas are common injuries with a percentage of up to 13 % of all cervical injuries. The most common classification is that of Gehweiler et al. who differentiated between five types of atlas fractures.
Type 1 is an isolated fracture of the anterior arch of the atlas. The frequency of this type in the literature is given with around 2 % of all atlas fracture. This fracture type is caused by an abrupt contraction of the longus colli muscle in hyperextension injuries. It is generally considered as stable (Fig. 12.3a).
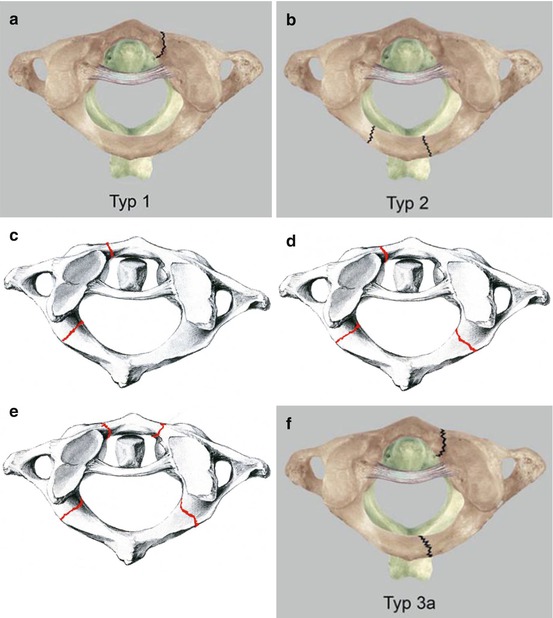
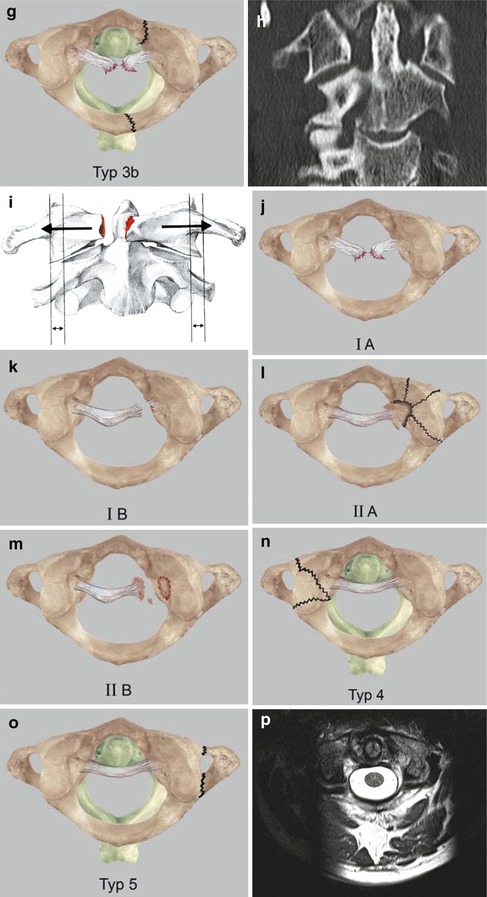
Fig. 12.3
(a) Atlas fractures according to Gehweiler et al. and ruptures of the transverse ligament according to Dickman et al. Type 1 is an isolated fracture of the anterior arch of the atlas, which is stable. (b) Type II is an isolated fracture of the posterior arch occurring always bilaterally. (c–e) Type III is a combined fracture of the anterior and posterior arch of the atlas. (f) Type III a are stable fractures where the transverse ligament is intact. (g) Type IIIb are unstable fractures where the transverse ligament is not intact. (h) Disruption or bony avulsion of the transverse ligament leads to a lateral shifting of the lateral masses (single arrows) which may be seen in plain radiograms and in CT scans. (i ) If the sum of shifting distances on both sides exceeds 7 mm (double arrows) a lesion of the transverse ligament must be assumed (Spence rule). (j, k) Dickman type I encompasses the injuries with an interligamentous rupture. In type Ia the rupture is located centrally in type Ib the rupture site is more laterally near the massa lateralis. (l, m) Dickman type II injuries injuries disconnect the tubercle for insertion of the transverse ligament from the C1 lateral mass involving a comminuted C1 lateral mass (type IIa) or avulsing the tubercle from an intact lateral mass (type II b). (n) Type IIa lesions also belong to the group of the Gehweiler type IV fractures. (o) This type describes an isolated lateral mass fracture. Gehweiler type V fractures are isolated fractures of the transverse process. (p) Besides the indirect signs (Spence rule, ADI, PADI), MRI of the craniocervical junction might be helpful to directly assess the transverse ligament, with a pathological signal in the vicinity of the transverse ligament. Reprinted with permission from Kandziora et al. [2], Tscherne and Blauth [3]
Type II is an isolated fracture of the posterior arch occurring always bilaterally at the thinnest portion of the posterior arch which is usually the sulcus of the vertebral artery (Fig. 12.3b). Unilateral fractures are combined with anterior arch fractures and are classified as type III. The mechanism of injury is a hyperextension combined with an axial compression. Type II atlas fractures are frequently combined with additional injuries or fractures of the cervical spine (e.g. fractures of the dens axis). Involvement of the sulcus of the vertebral artery needs further evaluation (CT angiography, MR angiography) of the vertebral artery to rule out traumatic arterial dissection.
Type III is a combined fracture of the anterior and posterior arch of the atlas. This is the classical atlas ring burst fracture which was first described by Jefferson. The fracture lines can be uni- or bilateral, and therefore two-, three- and four-part fractures are possible (Fig. 12.3c–e). The stability of this fracture form is largely determined by the integrity of the transverse ligament. Type IIIa are stable fractures where the transverse ligament is intact (Fig. 12.3f) and type IIIb are unstable fractures where the transverse ligament is not intact (Fig. 12.3g). Disruption or bony avulsion of the transverse ligament leads to a lateral shifting of the lateral masses which may be seen in plain radiograms and in CT scans (Fig. 12.3h). If the sum of shifting distances on both sides exceeds 7 mm, a lesion of the transverse ligament must be assumed (Spence rule) (Fig. 12.3i). Gehweiler type IIIb can be further subclassified according to Dickman. Dickman type I encompasses the injuries with an interligamentous rupture. In type Ia the rupture is located centrally while in type Ib the rupture site is more lateral near the massa lateralis (Fig. 12.3j, k). Dickman type II injuries are injuries disconnecting the tubercle for insertion of the transverse ligament from the C1 lateral mass involving a comminuted C1 lateral mass (type IIa) or avulsing the tubercle from an intact lateral mass (type IIb) (Fig. 12.3l, m). Type IIa lesions also belong to the group of the Gehweiler type IV fractures (Fig. 12.3n). This type describes an isolated lateral mass. If there is no lesion of the transverse ligament, Gehweiler type IV fractures are stable.
Gehweiler type V fractures are isolated fractures of the transverse process. This is a rare fracture type which is typically caused by punches (Fig. 12.3o). In type III Gehweiler fractures it is of paramount importance to estimate the stability of the transverse ligament. Besides the indirect signs (Spence rule, ADI, PADI), MRI of the craniocervical junction might be helpful to assess directly the transverse ligament (Fig. 12.3p).
Therapy. Stable Gehweiler fractures types I, II, IIIa, V and type IV fractures with minimal or no dislocation can be treated by immobilization in a soft collar for 8 weeks. Type IV fractures with a marked dislocation can be treated by immobilization for 12 weeks in a halo fixateur if a good reposition is achieved and can be maintained. If reposition cannot be achieved or maintained in a halo immobilization, a surgical fixation (either C1/C2 fixation or atlas-osteosynthesis) is indicated. Unstable type IIIb fractures with an interligamentous rupture of the transverse ligament (Dickmann type I) need to be stabilized by C1/C2 fixation. Dickman type 2 injuries can be treated with a mere atlas osteosynthesis or a C1/C2 fixation depending on the degree of dislocation.
12.3.2 Traumatic Atlantoaxial Dislocations
Ligamenteous atlantoaxial dislocations can basically be classified into three groups: translatory, rotatory and axial. Osteoligamentous instabilities such as transdental luxation fractures belong to a different entity.
Translatory atlantoaxial dislocation occurs as consequence of a rupture or bony avulsion of the transverse ligament. As a general rule, the transverse ligament is more stable than the dens axis. On the basis of the anterior atlantodental interval (AADI) (normal value up to 3 mm in adults) which determines the degree of translation Caffinière classified translatory atlantoaxial instabilities fall into three types:
Type I: AADI 4–5 mm (Fig. 12.4a)
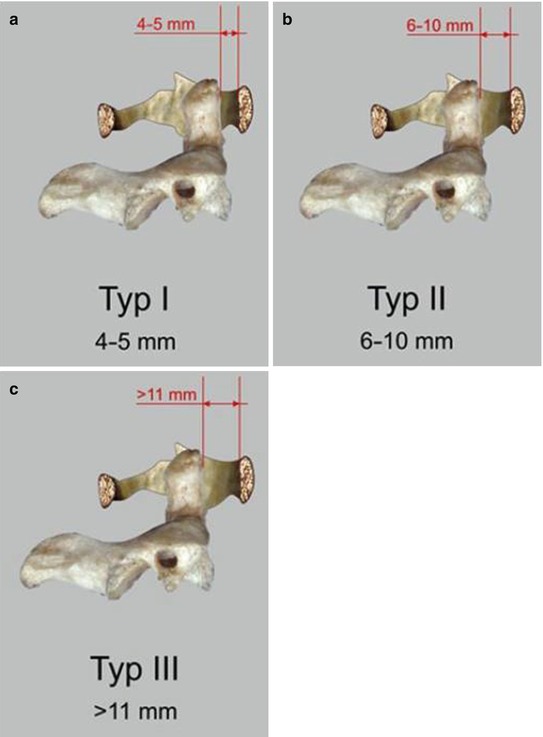
Fig. 12.4
(a) Translatory atalantoaxial dislocations. On the basis of the anterior atlantodental interval (AADI) Caffinière classified translatory atlantoaxial instabilities in three types: Type I: AADI 4–5 mm, (b) Type II: AADI 6–10 mm, (c) Type III: AADI >11 mm. Reprinted with permission from Kandziora et al. [1]
Type II: AADI 6–10 mm (Fig. 12.4b)
Type III: AADI > 11 mm (Fig. 12.4c)
Therapy. For treatment, the differentiation between bony avulsions of the transverse ligament and an interligamentous rupture is important. In cases with minor dislocation and contact, a conservative therapy with immobilization in a rigid collar can be carried out. In cases with severe dislocation or interligamentous rupture which have a very low healing tendency, a surgical atlantoaxial fixation has to be carried out.
Traumatic rotatory atlantoaxial dislocation is caused by rupture of the alar ligaments and additional rupture of the capsules of the lateral atlantoaxial joints, and occurs in children and adults after a sufficiently dramatic trauma. However, there is also a non-traumatic form of rotatory atlantoaxial dislocation which usually occurs in children spontaneously without trauma. Sometimes the medical history of these patients is significant for a surgical procedure of the pharynx or an infection of the upper respiratory tract. The degree of dislocation varies and the etiology of the non-traumatic atlantoaxial dislocation remains unclear.
Fieldings and Hawkins differentiated four types of atantoaxial dislocation:
Type I. Rotatory dislocation without anterior translation of the atlas. The center of rotation is the dens axis, the transverse ligament is intact and the AADI is normal (Fig. 12.5a).
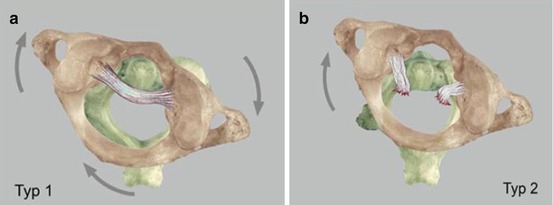
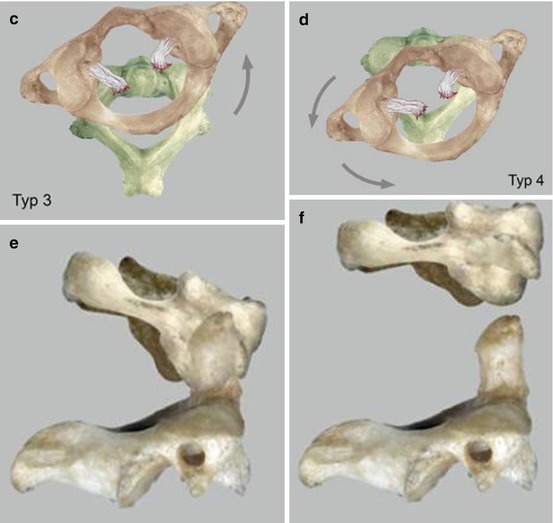
Fig. 12.5
(a) Traumatic rotatory atlantoaxial: Type I: rotatory dislocation without anterior translation of the atlas. The center of rotation is the dens axis, the transverse ligament is intact and the AADI is normal. (b) Type II: rotatory dislocation with anterior translation of the atlas. The sliding distance ranges from 3 to 5 mm. (c) Type III: rotatory dislocation with anterior translation of the atlas of more than 5 mm. (d) Type IV: rotatory dislocation with posterior translation of the atlas (arrows in a–d indicate the direction of rotation). (e) (Axial (cranial) atlantoaxial dislocations are very rare. (f) Partial dislocations are differentiated from complete forms. Reprinted with permission from Kandziora et al. [1]
Type II. Rotatory dislocation with anterior translation of the atlas. The sliding distance ranges from 3 to 5 mm. The transverse ligament may be insufficient. One lateral mass of the atlas is dislocated and the contralateral acts as the center of rotation (Fig. 12.5b).
Type III. Rotatory dislocation with anterior translation of the atlas of more than 5 mm. Besides an insufficiency of the transverse ligament, further ligaments and capsules are ruptured (Fig. 12.5c).
Type IV. Rotatory dislocation with posterior translation of the atlas. This type of dislocation is only possible if an additional instability of the dens is present (Fig. 12.5d).
Therapy. Atlantoaxial dislocations with rupture of the transverse ligament usually have to be treated with an atlantoaxial or occipitoatlantoaxial fixation. In cases with intact transverse ligament, a conservative treatment with immobilization in a rigid collar after repositioning is the therapy of choice. In cases with a tendency of relaxation, a halo should be used for immobilization.
Axial (cranial) atlantoaxial dislocations are very rare, unstable injuries with only a few reported cases in the literature. Partial dislocations with high grade instability are differentiated from complete dislocation (Fig. 12.5e, f).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








