Spinal Anatomy and Surgical Technique
1. How many pairs of spinal nerves do humans have?
There are 31 pairs of spinal nerves: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal
2. What percentage of people will experience low back pain at sometime in their lives?
80%1
3. What is the definition of acute low back pain?
Pain of 6 weeks or less duration2
4. What are some of the nonsurgical treatments for spinal stenosis?
• Nonsteroidal antiinflammatory drugs (NSAIDs), such as aspirin, naproxen2, ibuprofen, or indomethacin, to reduce inflammation and relieve pain
• Analgesics, such as acetaminophen, to relieve pain
• Corticosteroid injections into the outermost of the membranes covering the spinal cord and nerve roots to reduce inflammation and treat acute pain that radiates to the hips or down a leg
• Anesthetic injections, known as nerve blocks, near the affected nerve to temporarily relieve pain
• Restricted activity (varies depending on extent of nerve involvement)
• Prescribed exercises and/or physical therapy to maintain motion of the spine, strengthen abdominal and back muscles, and build endurance, all of which help stabilize the spine. Some patients may be encouraged to try slowly progressive aerobic activity such as swimming or using exercise bicycles.
• A lumbar brace or corset to provide some support and help the patient regain mobility. This approach is sometimes used for patients with weak abdominal muscles or older patients with degeneration at several levels of the spine.
5. Define radiculopathy.
Irritation of the lower motor neuron due to a mechanical or chemical insult to the nerve root in a single spinal level. It can result in burning pain and numbness along with weakness and loss of reflex in the corresponding nerve’s motor and sensory distribution.
6. What is the name given for compression when more than one nerve root is affected?
Polyradiculopathy
7. What is the Lasègue sign?
The straight leg raise test (SLR). This test is done during the physical examination and is positive when pain is elicited on lifting the leg passively off the table by the examiner.
8. In the cervical spine, which nerve root will be affected in case of a disk herniation?
The lower nerve root will be affected. For example, if there is a disk herniation at C4–C5, then the C5 nerve root will be affected.
9. What is a Spurling test?
In cases of radiculopathy, cervical extension with axial compression and rotation of the head to the pathology side decreases the size of the neural foramen and compresses the exiting nerve root resulting in increased pain or symptoms along the arm. A Spurling test is positive if the maneuver results in arm symptoms along the specific nerve distribution.3
10. What is cervical myelopathy?
It is caused by chronic pressure on the cervical spinal cord mostly due to a degenerative process. Myelopathy presents with the lower motor neuron symptoms in the upper extremity like loss of manual dexterity and muscular atrophy especially in the intrinsics. It can be accompanied by upper motor neuron signs in the lower and upper extremities such as hyperreflexia and spasticity. Neck pain and stiffness along with shuffling or waddling gait might also be present. Other physical signs may include clonus greater than 3 to 4 beats and positive Hoffman or Babinski signs.
11. What are the red flag symptoms in spinal evaluation?
Red flags indicate that further evaluation is needed and there might be a serious underlying pathology. The red flags include fever, pain in recumbent position, unexplained weight loss, bowel or bladder dysfunction, trauma, history of cancer, saddle anesthesia, osteoporosis, age > 50, failure to respond to standard treatment, and drug abuse.4
12. What is a Schober test?
It measures the movement of the lumbar spine eliminating the hip flexion: 10 cm proximal and 5 cm distal to the line between the posterior superior iliac spines in the midline are marked. The distance between them in flexion should be at least 5 cm more than in extension.
13. What is the appropriate test to perform in a malnourished patient with symmetric paresthesias in the feet and hands and poor proprioception on physical examination?
B12 level to rule out subacute combined degeneration5
14. The L4 reflex is elicited by which joint?
The knee
15. The Achilles reflex and sensation on the sole of the foot is supplied by which nerve root?
S1
16. In lateral recess stenosis, is a SLR positive or negative?
Negative
17. Can a positive SLR exclude the diagnosis of Guillain-Barré syndrome (GBS)?
No. The straight leg raise is often positive in GBS. Typically, a patient presents with back pain, radiculopathic symptoms, and a positive SLR. A history of a viral antecedent event, peak of symptoms at 4 weeks, areflexia, autonomic dysfunction, and high cerebrospinal fluid (CSF) protein help to make the diagnosis of GBS.
18. What is a Patrick test used in the examination of the lower extremities?
A test for arthritis of the hip. The thigh and knee of the supine patient are flexed, and the external malleolus of the ankle is placed over the patella of the opposite leg. The test is positive if depression of the knee produces pain. It is also called the FABER test for flexion, abduction, and external rotation.
19. What nerve roots are tensed by a straight leg raise maneuver?
L5 and S1
20. What type of nerves are contained in the dorsal ramus of the nerve root?
The dorsal ramus contains nerves that serve the dorsal portions of the trunk carrying visceral motor, somatic motor, and sensory information to and from the skin and muscles of the back.
21. What type of nerve root is located in the ventral ramus of the nerve root?
The ventral ramus contains nerves that serve the remaining ventral parts of the trunk and the upper and lower limbs carrying visceral motor, somatic motor, and sensory information to and from the ventrolateral body surface, structures in the body wall, and the limbs.
22. How is the pain from lateral recess stenosis and herniated lumbar disk affected by sitting?
Lateral recess stenosis pain is relieved by sitting, whereas herniated lumbar disk pain is exacerbated by sitting.
23. Why does a C5 radiculopathy follow anterior or posterior decompression in a minority of cases even if the case was done without obvious complication?
A C5 radiculopathy (deltoid weakness) may be related to traction on the nerve root from posterior migration of the cord after decompression because the C5 nerve has the shortest length from the foramen to muscle ending.
24. What urinary metabolite is elevated in Paget disease?
Hydroxyproline. The majority of pagetic lesions are symptomatic with lesions detected on radiographs for unrelated issues. The most common complaint in patients is back pain. Pagetic vascular steal is the compromise of vascular supply to the nerves of the spinal cord due to reactive vasodilatation of nearby vessels.
25. Which spinal tract is most responsible for lower limb subconscious proprioception from muscles, joints, and skin?
The spinocerebellar pathways
26. What is the significance of the intercristal line on anteroposterior (AP) and lateral x-rays?
It usually confirms the location of L5 and often the L4–L5 disk level.
27. What conditions may have L’Hermitte phenomenon as part of the patient’s history?
Multiple sclerosis, cervical myelopathy, and subacute combined degeneration
28. What type of nystagmus is present in compressive lesions of the craniocervical border?
Downbeat nystagmus
29. What type of traumatic spinal lesion results in a cape-like sensory deficit?
A central cord lesion damages the second sensory neuron crossing to join the lateral spinothalamic tract. Pain and temperature sensations are impaired bilaterally. Because sacral fibers are located most peripherally in the lateral spinothalamic tract, there is sometimes sacral sparing with central cord lesions. As the lesion expands, anterior horn cells may become involved and weakness may result.
30. How can it be possible for a C5–C6 disk to cause C7 symptoms?
This may be attributable to a prefixed brachial plexus in which normal levels of innervation are aberrant by one level. Normally, a C5–C6 disk herniation results in C6 nerve root compression and/or symptoms.
31. How can one differentiate mechanical back pain from ankylosing spondylitis-related back pain?
Rest usually relieves mechanical back pain; however, mild activity relieves the pain of ankylosing spondylitis. Patients with ankylosing spondylitis are frequently young men with the HLA-B27 genetic marker, morning stiffness (sometimes nocturnal pain), and sacroillitis.
32. Why are disk herniations usually posterolateral?
The presence of the posterior longitudinal ligament in the center prevents the disk from herniating directly posteriorly (Fig. 6.1).
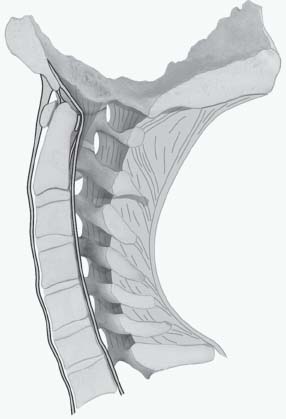
Fig. 6.1 A diagram showing the posterior and anterior longitudinal ligaments. These ligaments are strongest in the midline. (Source: Thieme Publishers.)
33. What makes up the annulus fibrosis?
Layers of fibrocartilage
34. What is the most common extraarticular manifestation of ankylosing spondylitis?
Acute anterior uveitis
35. What are the types of spondylolisthesis?
Congenital, ischemic, degenerative, traumatic, pathologic, and iatrogenic/postsurgical
36. Which type of spondylolisthesis is thought to result from a stress fracture of the pars interarticularis?
Isthmic spondylolisthesis
37. What are the main causes of thoracic myelopathy from degenerative disease?
Herniated disks, ossification of the posterior longitudinal ligament, ossification of the ligamentum flavum, and posterior bone spurs
38. What are some musculoskeletal conditions that can mimic lumbar spine problems?
Osteoarthritis of the hip joint can mimic anterior thigh pain due to the L2–L3–L4 radiculopathies. This can be distinguished by a hip range of motion examination especially with internal rotation, as well as by a Stinchfield test. Vascular insufficiency of the lower limb can cause claudication similar to spinal stenosis. This can be diagnosed by a peripheral vascular examination and differentiating the exacerbating and ameliorating factors between vascular and neurogenic claudication. Piriformis syndrome and inflammatory sacroillitis can mimic S1 radiculopathy with buttocks pain and radicular pain in the S1 distribution.
39. How long must elective surgery wait for a patient who has been taking Clopidogrel?
At least 7–10 days
40. What is the laboratory test needed to test coagulation for a patient taking clopidogrel?
Bleeding time. Remember that prothrombin time/partial thromboplastin time/international normalized ratio (PT/PTT/INR) may be normal in a patient taking clopidogrel; therefore, a bleeding time is necessary.
41. What is the cervical level of the inferior edge of mandible, the hyoid bone, thyroid cartilage, and cricoid ring?
Inferior edge of mandible: C2, hyoid bone: C3, thyroid cartilage: C4–C5, and cricoid ring: C6
42. Which is the largest and strongest cervical vertebra?
C2
43. Which vertebra has no body?
C1
44. Which vertebra is considered the cervicothoracic inflection point (the point where cervical lordosis becomes thoracic kyphosis)?
T3
45. What is the best way to verify (using anatomic landmarks) the T7 area when the patient is positioned prone on the operating table?
Drawing a line from one scapular tip to another best approximates the T7 lamina when radiographs cannot be used due to patient size or x-ray quality.6
46. What is the normal range of motion in the cervical spine?
• Flexion: 45 degrees
• Extension: 55 degrees
• Lateral bending: 40 degrees
• Rotation to each side: 70 degrees
47. Describe the sensory (s) and motor (m) distribution and reflex(r) of the cervical nerve roots?
• C5 = s: lateral arm; m: deltoid; r: none
• C6 = s: lateral forearm; m: wrist extension, biceps; r: brachioradialis
• C7 = s: middle finger; m: triceps, wrist flex, finger extension; r: triceps
• C8 = s: small finger; m: finger flexors; r: none
• T1 = s: medial arm; m: interossei; r: none
48. Which nerves arise from the lateral cord?
The lateral pectoral nerve to the pectoralis major muscle, the musculocutaneous nerve that innervates the biceps muscle, and partly the median nerve
49. Which nerves arise from the posterior cord?
The upper subscapular nerve (C7 and C8) to the subscapularis muscle, the lower subscapular nerve (C5 and C6) to the teres major muscle, the thoracodorsal nerve (C6, C7, and C8) to the latissimus dorsi muscle, the axillary nerve (sensation to the shoulder and motor to the deltoid muscle), and the radial nerve (the triceps brachii muscle, the brachioradialis muscle or musculus brachioradialis, the extensor muscles of the fingers and wrist)
50. What is the motor and sensory distribution of each lumbar nerve?
• L1: Sensation of the anterior thigh and innervation of the psoas muscle
• L2: Sensation of the anterior thigh and groin and innervation of the quadriceps muscle
• L3: Sensation of the anterior and lateral thigh and innervation of the quadriceps muscle
• L4: Sensation of the medial leg and foot and innervation of the tibialis anterior muscle
• L5: Sensation of the lateral leg and dorsal foot and innervation of the extensor hallucis longus muscle
• S1: Sensation of the lateral and plantar foot and innervation of the gastrocnemius and peronealis muscles
51. During a thoracolumbar spine procedure, dissection of the psoas muscle should take into account which nerve on the anterior surface of the muscle?
The genitofemoral nerve
52. Where and how does a disk herniation cause radiculopathy?
The exiting nerve root courses beneath the pedicle of the corresponding cephalad vertebra and above the caudad-intervertebral disk. The traversing nerve root courses medial to the pedicle of the cephalad vertebra over the intervertebral disk and then below the pedicle of the caudad vertebra. So a posterolateral disk herniation will compress the traversing nerve root of the motion segment, whereas a lateral herniation will compress the exiting nerve root. Large central disk herniation can affect a single or multiple caudal nerve roots and is a common cause of cauda equina syndrome. A central disk bulge can be asymptomatic and is different than a central disk herniation. For example, a posterolateral L4–L5 disk herniation affects the L5 root and a lateral L4–L5 disk herniation affects the L4 root (Fig. 6.2).
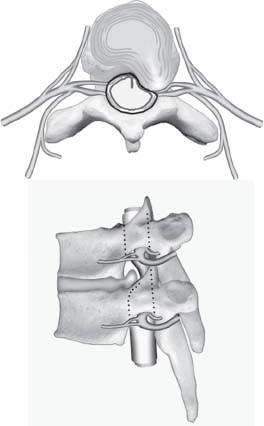
Fig. 6.2 A diagram of a disk herniation. For example, a L4–L5 disk usually compresses the L5 nerve root. (Source: Thieme Publishers.)
53. What is a superficial abdominal reflex?
They are performed by stroking each four quadrants of the abdomen and the normal response is the movement of the umbilicus toward the stroked segment. It is an upper motor neuron reflex and asymmetry suggests intraspinal (upper motor neuron) pathology. It should be evaluated with thoracic magnetic resonance imaging (MRI).
54. What anatomic landmarks are used to verify the location of a lumbar pedicle?
The crest of the transverse process is a good approximation of the center of the lumbar pedicle. Using a Leksell rongeur over this area will expose some cancellous bone that will confirm the center of the pedicle. After a laminectomy is done, feeling the pedicle from inside the canal with a Penfield #3 dissector will confirm the location of the pedicle. When a wide laminectomy is done, seeing the course of the nerve root is reassuring when placing the pedicle screw.
55. What ligaments serve as the ventral extent of safe dissection to avoid injury to the spinal nerve root during exposure and decortication of the transverse processes?
The intertransverse ligaments
56. What is the first vertebra that can safely accommodate a pedicle screw?
C7, there is usually no vertebral artery in the transverse foramen at this level, which often permits safe placement of a pedicle screw (Fig. 6.3).
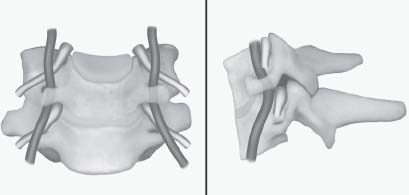
Fig. 6.3 A diagram showing the entrance of the vertebral artery in the foramen transversarium. (Source: Thieme Publishers.)
57. How can the correct placement of a pedicle screw be determined?
• By making sure that the screw is aimed medially
• By confirming placement with an x-ray (AP and lateral) before the screw is placed. Many spine device companies have a tool shaped like a gear shift to perform the initial localization.
• By feeling with a ball probe that bone is present in all areas surrounding the initial pilot hole
• By using neurophysiologic monitoring to test the pedicle screw once placed. The stimulation threshold should be greater than 12 mA.
58. The sympathetic plexus lies slightly ventral to what joint?
The costovertebral joint
59. Sympathetic outflow arises from what nucleus of the cord? At what spinal cord levels?
Sympathetic outflow arises from the intermediolateral nucleus of the spinal cord from T1 to L2.
60. Where is the best place near the nerve root to expose an intervertebral herniated disk?
The shoulder of the nerve root is the best place to expose and remove the disk. An extruded disk may sometimes be found in the axilla of the nerve root.
61. What are the indications for surgery in the lumbar spine?
• Emergent: Cauda equina syndrome, progressive motor deficit
• Elective: Incapacitating leg pain in the distribution of a specific nerve root
• Nerve root tension signs with or without neurologic signs
• Failure to respond to conservative treatment for 4 to 8 weeks
62. What are the indications for surgery in the cervical spine?
• Significant radicular pain (persistent or recurrent)
• Progressive neurologic deficit
• Progressive myelopathy or radiculopathy
63. When is the surgical intervention needed for spinal infection?
• Open biopsy to obtain tissue when closed biopsy has failed
• Failure of medical management with persistent pain and increased erythrocyte sedimentation rate (ESR) and/or C-reactive protein (CRP)
• Drainage of abscess
• Decompression of spinal cord or nerve root with neurologic deficit
• Correction of progressive or unacceptable spine deformity or instability
64. What are the surgical indications for primary spine tumor?
• Open biopsy for diagnosis
• Failure of chemotherapy or radiation
• Decompression of spinal cord or nerve roots with neurologic deficit
• Tumors resistant to medical treatment
• Correction of progressive or unacceptable spine deformity or instability
65. What are the surgical indications for metastatic spine tumor?
• Open biopsy for diagnosis
• Failure of chemotherapy or radiation
• Tumors resistant to medical treatment
• Correction of progressive or unacceptable spine deformity or instability
• Decompression of spinal cord or nerve roots with neurologic deficit
• Intractable pain or neurologic deficit during radiation therapy despite steroids
66. What are the indications of surgery for adult spine scoliosis?
Progressive deformity, intractable pain, cardiopulmonary symptoms, neurologic dysfunction, and cosmesis
67. When is revision surgery indicated?
The pathology should be correctable and the symptoms should be explained by this pathology. There is usually small correlation between the imaging findings and patient’s symptoms.
Surgery is recommended in the following situations: recurrent or persistent disk herniation or spinal stenosis, postlaminectomy instability, lumbar disk space infection following lumbar diskectomy, symptomatic lumbar pseudoarthrosis, and flatback syndrome
68. What areas of bone does a C1–C2 transarticular screw pass through if properly placed?
The inferior C2 facet (3 mm from the medial edge), the C2 pars interarticularis, and the C1 lateral mass. In 30% of patients, the position of the vertebral artery will preclude this type of surgery.
69. What are the landmarks for a C1–C2 puncture?
1 cm caudal and 1 cm posterior to the tip of the mastoid (aiming for the posterior third of the bony spinal canal under fluoroscopy)
70. What is another name for the dorsal ramus of the C1 nerve root?
The suboccipital nerve
71. Successful odontoid screw placement requires preservation of which ligament?
The transverse ligament7
72. In an anterior cervical diskectomy, what structures must be verified and retracted?
1. The platysma is the first muscle incised to gain access to the structures in the anterior neck area.
2. The carotid artery should be palpated and the pulse appreciated. The carotid artery should be carefully displaced laterally.
3. The esophagus needs to be identified and carefully placed medially. The esophagus can be confirmed by having anesthesia move the nasogastric tube if one is available.
4. The anterior spine can be exposed with blunt dissection and the first disk space encountered should be radiographed.
73. In which groove is the recurrent laryngeal nerve located?
The tracheoesophageal groove
74. On what side of the neck does the recurrent laryngeal nerve have a more variable course?
The recurrent laryngeal nerve has a more variable course on the right side of the neck and theoretically has an increased risk of injury on the right side.
75. What is the upper limit of traction that should be used in cervical spine injuries?
Ten pounds per level is the upper limit
76. What are some possible complications that can happen from an anterior cervical diskectomy and fusion (ACDF)?
The most common complication is the development of isolated postoperative dysphagia, postoperative hematoma sometimes requiring surgical intervention, symptomatic recurrent laryngeal nerve palsy, dural penetration, esophageal perforation, worsening of preexisting myelopathy, Horner syndrome, instrumentation failure/backout, and superficial wound infection.8
77. How can a patient develop Horner syndrome after a routine ACDF?
Disruption of the sympathetic plexus due to dissection too far lateral on the longus colli muscles—best to dissect laterally within 1 cm of the medial edge of the muscle
78. In an occipitocervical fusion, where is a safe area to drill a hole and place a screw in the occiput?
Halfway between the foramen magnum and the transverse sinus, and ~3 cm off the midline
79. What are some drugs that inhibit bony fusion?
Steroids, nonsteroidal antiinflammatory drugs (NSAIDs), immunosuppressive drugs, and nicotine. It is important that a patient stop or decrease smoking before and after undergoing a spinal fusion.
80. What devices and maneuvers postoperatively can increase the chances of a quality fusion?
• Use of a bone stimulator in the postoperative period
• Use of bracing intermittently (using a brace constantly will promote muscle atrophy)
• Cessation of smoking
• Maintaining a proper diet with adequate protein intake
• Maintaining proper glucose control in diabetic patients
81. Because a laminectomy cannot access the spaces lateral and anterior in the thoracic spine, what other options does the surgeon have for thoracic stenosis, tumor, or disk herniation?
Transthoracic, transpedicular, and costotransversectomy are potential approaches in the thoracic spine. Unlike the lumbar spine, the thoracic neural elements should not be manipulated or retracted as severe neurologic injury can result.
82. What does “ligamentotaxis” refer to in the setting of spinal stabilization?
Using posterior instrumentation to distract burst fractures to indirectly decompress the spinal canal. Intact ligaments can reimpact the bone fragments into the vertebral body following distraction.
83. What do SSEPs measure? TcMEPs? Pedicle screw stimulation?
The SSEP (somatosensory evoked potential) gives direct feedback on the integrity of the posterior columns by stimulating the posterior tibial nerve at the ankle and recording the responses from the popliteal fossa, cervical spine, and somatosensory cortex. In general, manipulations of the spinal cord and ischemic events will usually affect dorsal column function; thus, SSEPs correlate well with overall spinal cord function, but they do not indicate changes in motor pathways. The TcMEPs (transcranial motor evoked potentials) are determined by stimulating the scalp over the motor cortex; this gives direct feedback on the integrity of the corticospinal tracts of the spinal cord. Pedicle screw stimulation evaluates the integrity of the pedicle. Because bone is an insulator, an intact pedicle requires a threshold of 8 mA to activate the nerve. Anything less than this means that there is a possibility of a pedicle breach.
84. What spinous process of the cervical spine is the lowest bifid spine?
Usually C6
85. What is the average distance between the transverse foramina containing the vertebral arteries?
Three centimeters. Thus, it is imperative during an anterior diskectomy to ensure one is aware where midline is at all times. Complications of anterior cervical diskectomy of operating too lateral result in vertebral artery injury; likewise, operating too far laterally on the longus colli muscles can result in injury to the cervical sympathetic chain resulting in Horner syndrome.
86. Unilateral ligation of the vertebral artery usually has what consequences?
None. Unilateral ligation of the vertebral artery (if absolutely necessary) is usually well tolerated.
87. Where is the proper entry point and trajectory for lateral mass screws?
The entry point for lateral mass screws is 1 mm medial to the exact center of the lateral mass. The appropriate trajectory for lateral mass screws is 10 to 30 degrees in the cephalad direction (use the spinous process as a guide) and 10 to 30 degrees lateral, which facilitates the avoidance of the anterior neurovascular structures. There are different techniques and trajectories. It is recommended to study the preoperative films and determine the best trajectory for each patient. This is best done with an axial computed tomography (CT) scan.
88. What is BMP?
Bone morphogenetic protein (BMP) is a bone growth factor with osteoinductive properties to help promote bone formation. Target cells for BMP are primarily undifferentiated mesenchymal stem cells. Recombinant BMP2 is currently the only FDA-approved BMP product for spinal fusion.
89. What is the definition of pseudoarthrosis?
Pseudoarthrosis is the persistence of a motion segment resulting from the incomplete development of a rigid osseous construct after attempted bony fusion.
90. When is an intertransverse (Jane) procedure utilized?
A Jane intertransverse procedure through a Wiltse intermuscular approach is used to resect far lateral disk herniations. It involves removal of the most superolateral aspect of the facet joint while carefully preserving the pars interarticularis. A far lateral disk herniation often results in compression of the more cephalad (or exiting) nerve root rather than the traversing nerve root as in a posterolateral disk herniation.
91. How is a far lateral disk herniation identified and where is the most common location?
A far lateral disk herniation is located lateral to a line drawn between two adjacent pedicles. The most common level is L4–L5. Due to its location, the far lateral disk can compress the ganglion and the exiting and the traversing nerve root. The terrible pain that patients experience is from this ganglion irritation.
92. Where is the best place to insert an intrathecal baclofen pump?
The tip of the catheter is placed at the level corresponding with the therapeutic indication: T10–T12 for spastic diplegia, C5–T2 for spastic tetraplegia, and C1–C4 for generalized secondary dystonia.
93. Compare the fusion potential in anterior and posterior spinal fusions.
Because 80% of the body’s weight passes through the anterior spinal column, and only 20% passes through the posterior column, the bone graft placed in the anterior column is subject to compression, which promotes fusion. Additionally, the wide bony surface area and high vascularity of the vertebral endplates promote anterior interbody fusion. The bone graft placed in the posterior column is subject to tensile forces; therefore, fusion is more dependent on biologic factors such as osteogenic cells and the quality of the soft tissue bed into which the graft is inserted posteriorly.
94. What types of bone graft are recommended for posterior spinal fusion?
Autologous, cancellous iliac crest bone graft is considered the gold standard in posterior spinal fusion. Although allograft alone does not achieve a high fusion rate in adults, it is used frequently in pediatric patients with good success for scoliosis fusion. If enough autogenous graft is not available, then autograft extenders such as β-tricalcium phosphate, allograft, and biologics such as BMP and demineralized bone matrix can be used with good success if a meticulous decortication and a bone grafting technique are employed.
95. What is the difference between nonstructural and structural bone grafts?
Nonstructural bone grafts typically consist of particulate corticocancellous bone that can be used to promote arthrodesis between adjacent vertebral bodies, but the graft itself does not provide any stability to the anterior column. Structural grafts such as a femoral allograft ring with cortical bone provide mechanical support anteriorly during the process of fusion through the disk space.
96. How do you diagnose a pseudoarthrosis?
Localized pain over the fusion site after 6 to 12 months postoperatively should prompt imaging studies such as flexion and extension radiographs, technetium bone scan, or CT scan (the gold standard for imaging). Pseudoarthrosis is suggested by radiographic findings such as progressive spinal deformity, displacement in flexion and extension, broken screws, screws with halo effect, and discontinuity in the fusion mass. Surgical exploration of the fusion bed is the most accurate method to determine if a pseudoarthrosis is present.
97. What is the difference between a laminotomy, laminectomy, and laminoplasty?
A posterior approach is utilized for all three procedures with the surgical goal to decompress the neural elements. A laminotomy is usually unilateral and partial removal of the lamina or facet joint to decompress the ipsilateral nerve root or dural sac is performed. In a laminectomy, the spinous process and the entire lamina are removed. In a laminoplasty, the area for the neural elements is widened through the lamina but without removal of the posterior spinal elements.
98. When is the posterior surgical approach employed for cervical decompression?
If three or more levels require surgical decompression, a posterior surgical approach is frequently recommended. To perform a posterior laminectomy or laminoplasty for decompression, a neutral to lordotic sagittal alignment of the cervical spine should be present, which permits dorsal migration of spinal cord away from the anterior pathology. Multilevel posterior laminectomy for decompression is often combined with instrumented fusion to avoid postlaminectomy kyphosis. A cervical laminoplasty can provide central decompression without fusion with the caveat that the patient does not have significant preoperative neck pain because postoperative neck pain can occur. A unilateral cervical keyhole laminoforaminotomy is utilized to decompress for unilateral arm pain caused by a soft posterolateral disk herniation or foraminal stenosis from facet hypertrophy.
99. When is an anterior surgical approach indicated for decompression of the cervical spine?
In patients with cervical spinal stenosis who have three or fewer involved levels. In this approach—regardless of the lordotic, neutral, or kyphotic sagittal plane alignment—the decompression can be successful. If neural compression is localized to the level of disk space, multilateral diskectomy and interbody fusion might be used. When cord compression extends beyond the disk level or when a significant kyphotic deformity is present, an anterior corpectomy and a strut graft are performed.
100. When should anterior and posterior approaches be combined in the cervical spine?
In multilevel conditions, such as cervical stenosis, which requires three or more levels of anterior surgical approach decompression; two or more levels of corpectomies when associated with kyphotic deformity; and in rigid posttraumatic or postlaminectomy kyphosis (Fig. 6.4)
101. What nerve root injury is the most common after cervical laminectomy or laminoplasty?
C5 nerve root. Dysfunction may appear immediately following surgery, but can appear in a delayed fashion several days after the surgery. It is believed that because the C5 nerve is short in length, tension is produced as the spine is decompressed in this area. This tension deprives the nerve of oxygen and nutrients and may be a cause of the dysfunction.

Fig. 6.4 An example of postlaminectomy kyphosis. This patient eventually needed posterior fixation via lateral mass screws.
102. Should a laminectomy be performed for the treatment of a thoracic disk herniation?
In the thoracic spine a midline laminectomy and midline approaches should be avoided because they are associated with a high rate of complications such as paraplegia. This approach provides poor access to the central lateral aspect of this space; due to the risk of paraplegia, retraction of the spinal cord is not advised.
103. What are the indications for performing a corpectomy in the thoracic or lumbar spine?
Burst fractures with retropulsed bone causing anterior cord compression, tumor extending from the posterior part of the vertebral body into the spinal canal, osteomyelitis, and in cases with collapsed vertebral body with retropulsed material in the canal. It is also indicated for drainage of a vertebral abscess.
104. What are some intraoperative maneuvers that can decrease the postoperative pain of a lumbar laminectomy?
• Injecting bupivacaine in the paraspinal musculature at the end of the case
• Placing an epidural pain catheter
• Minimizing the muscle dissection during exposure
• Releasing the retractors periodically to prevent venous congestion and skin necrosis
105. What are the proper ways to deal with an inadvertent dural breach?
1. Place a cottonoid on the dural breach and remove some CSF to allow the nerves to descend in the thecal sac.
2. Under magnified vision, place a 4–0 suture starting at the beginning of the breach and continue to the end. This can be done in a running or interrupted fashion depending on the nature of the tear. A patch of muscle may be used to augment the closure. If no dural edges are available, then using a dural substitute is an option. More bone may have to be removed in order to expose the edges of the dural breach and facilitate its primary closure.
3. Ask the anesthetist to perform a Valsalva maneuver to verify the quality of the sutured area.
4. Use a fibrin sealant over the sutured area. Apply the sealant in layers alternating with surgical patches rather than placing the entire amount at one time.
5. During closure of the incision, perform a watertight closure of the fascial layer and a thorough closure of the skin edges using a 2–0 or 3–0 nylon suture (running or interrupted). If a JP drain is necessary it is best to place this under the fascia.
6. Place the patient on at least 3 days of antibiotics and remove the drains promptly.
106. If a wound continues to leak CSF even though all the above maneuvers were employed at surgery, what is the accepted next step?
Insertion of a lumbar drain at a site away from the incision can help the wound to seal by creating a path of least resistance. Ten to 15 mL per hour can be drained for up to 5 days. At that time, the drain can be clamped for 12 to 24 hours and discontinued thereafter. If this drainage maneuver fails, it is prudent to reexplore and close the leak.
107. What is accepted antibiotic usage preoperatively, intraoperatively, and postoperatively?
• Preoperative: 30 minutes before skin incision
• Intraoperatively: Every 6 hours of operating time antibiotics should be repeated
• Postoperatively: 3 to 6 doses of antibiotics (24–48 hours) or antibiotics for as long as a drain is in place



