18 Spine and Spinal Cord
 Low Back Pain and Radiculopathy
Low Back Pain and Radiculopathy
1. Complete the following about low back pain and radiculopathy: |
| G7 p.428:70mm |
a. True or False. Bed rest beyond 4 days may be more harmful than helpful for patients with low back pain. | true |
|
b. True or False. 60% of patients with low back pain will improve clinically within 1 month even without treatment. | false (89 to 90% will improve in 1 month even without treatment) |
|
c. Pure radicular symptoms will include upper motor neuron (UMN) signs or lower motor neuron (LMN) signs? | LMN signs (Radiculopathy will/may show associated decreased reflexes, weakness, and atrophy.) |
|
2. True or False. The percentage of low-risk back pain patients who will improve without treatment in 1 month’s time is |
| G7 p.428:78mm |
a. 10% | false |
|
b. 20% | false |
|
c. 90% | true (Most low back patients will resolve and no specific diagnosis can be made in 85% despite aggressive workup.) |
|
d. none | false |
|
3. The nucleus pulposus is a remnant of the embryonic _____. | notocord | G7 p.428:160mm |
4. True or False. The following may be considered a nonpathological condition: |
| G7 p.429:37mm |
a. degenerated disc | false |
|
b. protruded disc | false |
|
c. bulging disc generalized > 50% | true (Bulging disc is circumferential symmetrical extension of the disc beyond the end plates. Incidence increases with age.) |
|
d. herniated disc | false |
|
e. focal bulging disc | false | |
5. True of False. Gas in the disc usually is a sign of |
| G7 p.429:37mm |
a. disc infection | false |
|
b. disc generation | true |
|
c. aka v_____ d_____ | vacuum disc |
|
6. An extruded disc where the free fragment is contained by the posterior longitudinal ligament is called a _____ disc. | sequestered | G7 p.429:95mm |
7. Give the definition of a sequestered disc. |
| G7 p.429:95mm |
a. _____disc | extruded |
|
b. that has lost _____ | continuity |
|
c. with its disc of _____ | origin |
|
d. also known as a _____ _____ | free fragment |
|
8. Provide the Modic classification. |
| G7 p.430:20mm |
a. Type 1 T1W1_____ T2W1_____ | ↓ ↑ |
|
b. Type 2 T1W1_____ T2W1_____ | ↓ ↑ |
|
c. Type 3 T1W1_____ T2W1_____ | ↓ ↑ |
|
9. Kyphosis |
| G7 p.430:35mm |
a. is measured by the _____ angle. | Cobb |
|
b. Drawn with a line parallel to the |
|
|
i. superior end plate of the body _____ and the | above |
|
ii. inferior end plate of the body _____. | below |
|
10. Scoliosis |
|
|
a. is a measure of _____ of the curvature. | convexity | G7 p.430:60mm |
b. Drawn with a line parallel to the superior end plate of the _____ body and the | uppermost |
|
c. inferior end plate of the _____ body involved. | lowermost |
|
d. Draw _____ to these lines | perpendicular |
|
e. and measure the _____. | angle |
|
11. Oswestry disability index |
| G7 p.430:105mm |
a. is a scale used for _____ _____. | back pain |
|
b. A score of _____% is essentially totally disabled. | 45% |
|
c. A functional score is in the _____. | teens |
|
12. Signs of cauda equina syndrome include |
| G7 p.431:110mm |
a. a_____ | anesthesia (saddle) |
|
b. b_____ | bladder incontinence |
|
c. c_____ | continence of stool impaired | |
d. d_____ | dolor leg pain (unilateral/bilateral) |
|
e. l_____ | leg weakness (unilateral/bilateral) |
|
13. True or False. Cauda equina syndrome may include the following: |
| G7 p.431:110mm |
a. bladder dysfunction (incontinence or retention) | true |
|
b. Faber sign or Patrick-Faber sign (flexion abduction external rotation) | false (Positive in hip joint disease and does not exacerbate true nerve root compression.) |
|
c. saddle anesthesia | true |
|
d. unilateral/bilateral leg weakness/pain | true |
|
e. fecal incontinence | true |
|
14. Name the associated nerve root for each of the following: |
| G7 p.432:28mm |
a. great toe strength | L5 and some L4 |
|
b. dorsal foot sensation | L5 |
|
c. lateral foot sensation | S1 |
|
d. medial foot sensation | L4 |
|
e. plantar foot sensation | S1 |
|
f. Achilles reflex | S1 |
|
15. For patients with low back pain, red flags for a serious underlying pathology would include signs consistent with what conditions? |
| G7 p.432:65mm |
Hint: cisc |
|
|
a. c_____ | cauda equina syndrome |
|
b. i_____ | infection |
|
c. s_____ | spinal fracture |
|
d. c_____ | cancer |
|
16. Electromyography (EMG) is not helpful to evaluate for myelopathy, myopathy, or nerve root dysfunction unless the symptoms have been present for at least _____ weeks. | 3 to 4 (Results are variable before this time.) | G7 p.432:65mm |
17. True or False. Regarding plain lumbosacral spine x-rays: |
| G7 p.434:70mm |
a. Are recommended for routine evaluation of back pain | false |
|
b. When indicated AP and lateral views are usually adequate | true |
|
c. Unexpected findings occur frequently | false |
|
d. Gonadal radiation is insignificant | false |
|
e. Appropriate in patients who have “red flags” | true | |
18. True or False. Red flags include |
| G7 p.434:105mm |
a. patients underage 20 | true |
|
b. patients over age 50 | false (> 70) |
|
c. drug users | true |
|
d. diabetics | true |
|
e. postop urinary tract patients | true |
|
f. persistent pain for more than 1 week | false (> 4 weeks) |
|
19. Complete the following about low back pain and radiculopathy: |
| G7 p.435:60mm |
a. Signs on MRI that indicate disc degeneration include |
|
|
i. increase or decrease of signal intensity on T2-weighted imaging (T2WI)? | decrease |
|
ii. increase or decrease of disc height? | decrease |
|
b. Signs on computed tomography (CT) that indicate disc herniation include |
|
|
i. increase or decrease of the normal epidural fat? | decrease |
|
ii. _____ of the thecal sac | indentation |
|
c. Will CT show loss of concavity, or convexity, of the thecal sac? | convexity | G7 p.435:96mm |
20. Other useful tests include the following: |
| G7 p.435:155mm |
a. myelogram-CT. Identifies contribution to cause of pressure by _____. | bone |
|
b. discography |
|
|
i. reliability_____ | controversial |
|
ii. interpretation_____ | equivocal |
|
iii. false positives_____ | high |
|
iv. may help in cases of_____ _____if one | multiple discs |
|
v. produces | pain |
|
21. List five signs of psychosocial distress in back pain, remembering that inappropriate response to any three suggests distress is present. |
| G7 p.436:138mm |
Hint: ppaim |
|
|
a. p_____ | physical exam over reaction |
|
b. p_____ | pain on superficial palpation |
|
c. a_____ | axial loading produces pain |
|
d. i_____ | inconsistent SLR |
|
e. m_____ | motor or sensory exam inconsistent |
|
22. Clear indications for urgent lumbar surgery include |
| G7 p.436:175mm |
a. c_____ e_____ s_____ | cauda equina syndrome |
|
b. p_____ n_____ d_____ | progressive neurological deficit |
|
c. p_____ w_____ | profound weakness (motor) | |
23. True or False. The following conservative therapy treatments have shown proven benefit for patients with back pain: |
| G7 p.437:40mm |
a. epidural steroids | false |
|
b. transcutaneous electrical nerve stimulation (TENS) | false |
|
c. traction | false |
|
d. oral steroids | false |
|
e. spinal manipulation | false |
|
f. muscle relaxants | false | G7 p.438:50mm |
24. Is there a risk to the use of Parafon Forte? If so what is the risk? | yes; fatal hepatotoxicity | G7 p.438:62mm |
25. True or False. Standard discectomy and microdiscectomy are of similar efficacy. | true | G7 p.440:25mm |
26. Injection of chymopapain into herniated discs for treatment carries a significant risk of_____. | anaphylaxis | G7 p.440:40mm |
27. The patient’s chances of returning to work if off for |
| G7 p.440:145mm |
a. 6 months is_____% | 50% |
|
b. 1 year is_____% | 20% |
|
c. 2 years is_____% | <5% |
|
 Intervertebral Disc Herniation
Intervertebral Disc Herniation
28. Enumerate the changes that occur in the intervertebral disc with increasing age. |
| G6 p.323:80mm |
|
| G5 p.295:120mm |
Hint: ddddisc |
|
|
a. d_____ | decrease disc height |
|
b. d_____ | decrease in proteoglycan content |
|
c. d_____ | desiccation (loss of hydration) |
|
d. d_____ | degeneration of mucoid |
|
e. i_____ | ingrowth of fibrous tissue |
|
f. s_____ | susceptibility to injury |
|
g. c_____ | circumferential tears of the annulus |
|
29. Complete the following concerning the aging of a disc: |
| G5 p.295:121mm |
a. What decreases? |
|
|
i. _____ | proteoglycan content |
|
ii. _____ | water |
|
b. What increases? |
|
|
i. _____ | mucoid degeneration |
|
ii. _____ | fibrous tissue ingrowth |
|
c. This results in |
|
|
i. _____ | annular tears |
|
ii. _____ | nucleus herniation | |
30. Complete the following about sagittal balance: |
| G7 p.441:130mm |
a. Assessment requires a |
|
|
i. s_____ | standing |
|
ii. l_____ and | lateral |
|
iii. f_____ spine x-ray. | full |
|
b. A plumb line is drawn |
|
|
i. from the center of_____ | C7 |
|
ii. to the disc space of_____. | L5S1 |
|
iii. Within_____ | 3.2 cm ± |
|
iv. behind the s_____ p_____ is | sacral promontory normal. |
|
31. Typical disc herniation compresses the nerve existing_____. | below | G7 p.442:100mm |
32. True or False. Surgical indications include |
| G7 p.442:115mm |
a. cauda equina syndrome | true |
|
b. numbness of foot | false |
|
c. progressive symptoms | true |
|
d. abnormal MRI | false |
|
e. neurologic deficits | true |
|
f. abnormal discogram | false |
|
g. failed conservative treatment | true |
|
h. pain when coughing | false |
|
i. severe radicular pain for 2 weeks | false (6 weeks) |
|
j. severe back pain | false |
|
33. The posterior longitudinal ligament |
| G7 p.442:160mm |
a. is strongest in the_____. | midline |
|
b. Therefore, most disc herniations occur off to _____. | one side |
|
34. Complete the following regarding lumbar disc herniation: |
| G7 p.443:35mm |
a. The occurrence of voiding dysfunction in lumbar disc herniation varies from_____to_____%. | 1 to 18% |
|
b. Concerning bladder symptoms, what is the sequence from the earliest findings? |
|
|
i. d_____ b_____ s_____ | decreased bladder sensation |
|
ii. u_____ u_____ | urinary urgency |
|
iii. i_____ f_____ | increased frequency due to increased postvoiding residual |
|
iv. e_____ and i_____ | enuresis (bed wetting) and incontinence are rare |
|
c. Urinary retention with overflow incontinence is suggestive of what diagnosis? | cauda equina compression |
|
35. What is the most sensitive sign of herniated lumbar disc? | the Lasègue sign | |
36. The significance of a positive crossed straight-leg raising sign is |
| G7 p.443:132mm |
a. specificity for nerve root compression of _____% | 90% |
|
b. It suggests a more_____HNP. | central |
|
c. It may correlate with a disc_____ _____ _____ _____ of the contralateral root. | fragment within the axilla |
|
d. Lasègue specificity for root compression is_____%. | 83% |
|
e. For crossed Lasègue it is_____%. | 90% |
|
37. Describe a positive Lasègue sign. |
| G7 p.443:155mm |
a. Patient’s position is_____. | supine |
|
b. Raise leg by the ankle until_____ _____. | pain elicited |
|
c. Pain occurs below_____degrees. | 60 |
|
d. It is positive in_____% herniated nucleus pulposus (HNP). | 83% |
|
38. Describe the following techniques to elicit indications of nerve root tension: |
| G7 p.443:155mm |
a. Lasègue sign_____ _____ _____ | straight leg raising (SLR) |
|
b. Cram test_____ _____ with _____ _____ | extend knee with leg raised |
|
c. Fajersztajn sign _____ _____ | crossed SLR (central disc)= 97% HNP (crossed Lasègue test) |
|
d. femoral stretch test_____ | prone, knee maximally flexed = L2, L3, L4 root lesions |
|
e. bowstring sign_____ _____ _____ _____ | flex knee after SLR, hip pain persists but sciatic pain ceases |
|
f. sitting knee extension_____ _____ | sitting SLR |
|
39. Describe the Faber test. |
| G7 p.444:90mm |
a. another name? | Patrick sign |
|
b. perform by? | flexion abduction external rotation |
|
c. positive in? | hip pathology |
|
40. Complete the following regarding the Trendelenburg sign: |
| G7 p.444:110mm |
a. The affected hip_____ when the patient is walking, | dips |
|
b. which indicates the contralateral thigh adductors are _____. | weak | |
c. This causes the contralateral pelvis to _____, | tilt |
|
d. which is caused by a lesion of the_____root. | L5 (Affected hip dips when walking to indicate weakness of contralateral thigh adductors, or while standing on leg with weak adductors causes pelvis to tilt contralateral to weakness [L5 lesion].) |
|
41. Complete the following about crossed adductors sign: |
| G7 p.444:120mm |
a. Crossed adductors sign is positive when knee jerk is elicited and the contralateral thigh_____ _____. | adductors contract |
|
b. If knee jerk is |
|
|
i. hyperactive it suggests_____. | UMN lesion |
|
ii. hypoactive it suggests_____. | pathological spread due to nerve root irritation |
|
42. Complete the following about Hoover’s sign: |
| G7 p.444:133mm |
a. It is a test to learn if patient’s leg weakness is_____. | functional |
|
b. Examiner places hands under patients_____. | heels |
|
c. Patient is asked to lift each leg from the_____. | bed |
|
d. If when lifting the normal leg the weak heel pushes_____. | down |
|
e. we know the leg has_____ | strength |
|
f. and the alleged weakness is_____. | functional |
|
43. For the listed lumbar disc level, what is the frequency of herniated disc syndrome? |
| G7 p.444:133mm |
a. L5-S1_____% | 45 to 50% |
|
b. L4-5_____% | 40 to 45% |
|
c. L3-4_____% | 3 to 10% |
|
44. Name physical findings associated with an L5-S1 disc herniation and where pain radiates. |
| G7 p.445:50mm |
a. reflex, a_____A_____ | absent Achilles tendon reflexes |
|
b. motor, g_____w_____ | gastrocnemius weakness (plantar flexion) |
|
c. sensory, decreased at l_____m_____and l_____f_____ | foot |
|
d. pain, p_____c_____ | posterior aspect of calf to the ankle |
|
45. How many vertebrae (presacral) are there in the typical human? | 24 | |
46. Name three indicators for emergency lumbar surgery. |
| G7 p.445:160mm |
Hint: ces, pmd, ip |
|
|
a. ces_____ | cauda equina syndrome—urinary retention or overflow incontinence, saddle anesthesia |
|
b. pmd_____ | progressive motor deficit—“foot drop” |
|
c. ip_____ | intolerable pain (urgent) |
|
47. List potential findings for cauda equina syndrome. |
| G7 p.446:30mm |
Hint: cauda s |
|
|
a. c_____ | can’t function sexually—sexual dysfunction |
|
b. a_____ | ankle jerks absent |
|
c. u_____ | urinary retention/incontinence |
|
d. d_____ | diminished sphincter tone |
|
e. a_____ | anesthesia of saddle area |
|
f. s_____ | strength is decreased |
|
48. True or False. The following is classically recognized as a cause of the cauda equina syndrome: |
| G7 p.446:90mm |
a. tumor | true |
|
b. epidural spinal hematoma | true |
|
c. free fat graft following discectomy | true |
|
d. trauma/fracture | true |
|
e. lumbar stenosis | false (Lumbar stenosis is a more chronic process and therefore would not classically give an acute/subacute presentation of cauda equina syndrome.) |
|
49. True or False. In cauda equina syndrome, surgery should be performed |
| G7 p.447:35mm |
a. stat | false |
|
b. within 24 hours | false |
|
c. within 48 hours | true |
|
d. within 72 hours | false |
|
e. within a week | false | |
50. True or False. Comparing microdiscectomy to standard discectomy for lumbar disc herniation, which of the following are true? |
| G7 p.447:114mm |
a. shorter incision | true |
|
b. shorter hospital stay | true |
|
c. less blood loss | true |
|
d. better efficacy | false (Efficacy has been shown to be equivalent between the two techniques.) |
|
e. may be more difficult to retrieve large fragments | true |
|
51. Success rate at 1 year for surgical discectomy is_____%. | 85% | G7 p.447:143mm |
52. Success rate at 1 year for chemonucleolysis (CNL) is_____%. | 44 to 63% | G7 p.447:146mm |
53. The percentage of patients of chemonucleolysis who eventually undergo surgery for unresolved symptoms is_____%. | approximately 56% at 6 months | G7 p.447:152mm |
54. Complete the following about intradiscal procedures: |
| G7 p.448:23mm |
a. What percent of lumbar disc patients considered for surgery could be candidates for intradiscal procedures? | 10 to 15% |
|
b. What is the success rate of intradiscal procedures? | 37 to 75% | G7 p.448:60mm |
55. True or False. Following discectomy: |
| G7 p.448:140mm |
a. epidural steroids prior to closure have no benefit. | true |
|
b. systemic steroids and bupivacaine may reduce hospital stay and postop narcotic requirements. | true |
|
56. True or False. Regarding epidural free fat graft: |
| G7 p.448:168mm |
a. It can cause nerve root compression. | true |
|
b. It is believed to reduce epidural scar formation. | Opinions on whether it reduces scar formation are mixed. |
|
c. Some believe it may increase epidural scar. | true |
|
d. It increases the incidence of postoperative infection. | false |
|
e. It may cause cauda equina syndrome. | true, rarely | |
57. Characterize complications of lumbar disc surgery. |
| G7 p.449:25mm |
a. mortality_____% | 0.06% (1/1800 pts) |
|
b. superficial infection_____% usual organism_____% | 1 to 5%; Staphylococcus aureus |
|
c. deep infection_____% | < 1% |
|
d. discitis_____% | 0.5% |
|
e. motor deficit_____% | 1 to 8% |
|
f. durotomy_____% | 0.3 to 13% |
|
g. after redo_____% | 18% |
|
h. surgical repair_____ | 1/1000 pts |
|
i. pseudomeningocele_____% | 0.7 to 2% |
|
j. recurrent disc_____% | 4% (1.5% first year) 10-year follow-up |
|
58. Complete the following about durotomy: |
| G7 p.449:60mm |
a. What is the incidence of incidental durotomy in lumbar laminectomy? | incidence is 0.3 to 13% (increases up to 18% in reoperations) |
|
b. Give four possible complications related to incidental durotomies |
|
|
i. C_____ | CSF fistula-requiring repair in ˜10 per 10,000 |
|
ii. p_____ | pseudomeningocele 0.7 to 2% |
|
iii. h_____ | herniation of nerve roots |
|
iv. i_____ | increased epidural bleeding |
|
59. What is the incidence of recurrent herniated lumbar disc? |
| G7 p.449:80mm |
a. same level either side in first 10 years _____% | ˜4% |
|
b. any level over 10 years_____% | 3 to 19% |
|
c. first year same level either side |
| |
d. any different incidence depending on level | two times more common at L4-5 |
|
e. same level recurrence_____% | 74% |
|
f. different level recurrence_____% | 26% had herniated disc at another level |
|
60. Complete the following regarding the anterior longitudinal ligament: |
| G7 p.449:103mm |
a. Asymptomatic perforations occur in _____% of discectomies. | 12% |
|
b. Depth of disc space is_____. | 3.3 cm |
|
c. Vascular injury produces bleeding into operative field only_____% of the time. | 50% |
|
d. Great vessel injury mortality is_____%. | 37 to 67% | |
61. Enumerate five complications related to positioning for lumbar discectomies. |
| G7 p.450:90mm |
Hint: tecup |
|
|
a. t_____ | tibialis anterior compartment syndrome |
|
b. e_____ | eyes pressure |
|
c. c_____ | cervical spine injury |
|
d. u_____ | ulnar nerve compression |
|
e. p_____ | peroneal nerve compression |
|
62. True or False. Regarding unintended durotomy: |
|
|
a. Normal ambulation is not considered a cause for failure of dural repair. | true | G7 p.451:135mm |
b. Risk of a cerebrospinal fluid (CSF) leak is increased in |
|
|
i. revision surgery | true |
|
ii. removal of ossification of the posterior longitudinal ligament (OPLL) | true |
|
iii. high-speed drills | true |
|
c. It is not considered an act of malpractice. | true |
|
d. The use of fibrin glue to close is advantageous. | true |
|
e. It can be due to thinned dura by longstanding stenosis. | true |
|
63. Enumerate four signs of postoperative cauda equina syndrome (i.e., from epidural hematoma). |
| G7 p.452:78mm |
Hint: pain |
|
|
a. p_____ | pain out of the ordinary |
|
b. a_____ | anesthesia of saddle area |
|
c. i_____ | inability to void |
|
d. n_____ | numerous muscle groups weak |
|
64. True or False. Regarding the outcome of surgical treatment of lumbar herniated disc: |
| G7 p.452:127mm |
a. 5% will be classified as having failed back syndrome. | true |
|
b. At 1 year the surgical group had a better outcome than with conservative treatment. | true | |
c. The benefit persisted at 10 years. | false (Surgery group had better outcome at 1 year but benefit was no longer statistically significant at 4-year follow-up. At 10 years neither surgical nor conservative treatment group complained of sciatica or back pain.) |
|
d. 63% had complete relief of back pain at 1 year postop. | true |
|
e. At 5- to 10-year follow-up 86% felt improved. | true |
|
65. True or False. The percentage of patients with L3-4 disc herniation having a past history of L4-5 or L5-S1 disc herniation is |
| G7 p.453:28mm |
a. < 10% | false |
|
b. approximately 25% | true |
|
c. approximately 50% | false |
|
d. 60 to 80% | false |
|
e. almost 90% | false |
|
66. Characterize a herniated upper lumbar disc. |
| G7 p.453:33mm |
a. What is the incidence? |
|
|
i. L1-2_____% | 0.28% |
|
ii. L2-3_____% | 1.3% |
|
iii. L3-4%_____ | 3.6% |
|
b. Most common muscle involved? | quadriceps femoris |
|
c. Femoral stretch test_____ | may be positive |
|
d. Knee jerk_____ | reduced in 50% |
|
67. Characterize extreme lateral lumbar disc herniations. |
| G7 p.453:105mm |
a. What is the incidence? | 3 to 10% |
|
b. What level is most commonly involved? |
|
|
i. L4-5_____% | 60% |
|
ii. L3-4_____% | 24% |
|
iii. L5-S1_____% | 7% |
|
c. Enumerate four differences compared with other common disc herniations |
|
|
i. Straight leg raising (SLR) is negative in_____%. | 85 to 90% |
|
ii. Pain is increased by lateral bending in_____%. | 75% |
|
iii. Pain is more_____. | severe |
|
iv. Extruded fragments are_____. | more frequent | |
68. Distinguishing features concerning far lateral disc herniation include the following: |
| G7 p.453:118mm |
a. The root involved is the root_____ _____ _____ _____ | exiting at that level negative |
|
b. SLR is_____. | negative |
|
c. Lateral bending is_____. | likely to produce pain |
|
d. Severity of pain is_____ because _____ _____ _____ is compressed. | greater; dorsal root ganglion |
|
e. Most common levels are_____and_____. | L4-5 and L3-4 |
|
f. Best surgical approach is_____ _____. | standard hemilaminectomy (and follow nerve laterally; perform medial facetectomy) |
|
69. Zones in which disc herniation can occur are |
| G7 p.453:128mm |
a. c_____ | central |
|
b. s_____ | subarticular |
|
c. f_____ | foraminal |
|
d. e_____ | extraforaminal |
|
70. True or False. One third of extreme lateral lumbar disc herniations are missed on initial radiologic exams. | true | G7 p.454:70mm |
71. To test for far lateral disc what is the value of postdiscography CT scan? | may be a most sensitive test— 94% | G7 p.454:94mm |
72. Give the incidence of surgery for herniated discs in pediatric patients. |
| G7 p.455:65mm |
a. under 20 years of age_____% | less than 1% |
|
b. under 17 years of age_____% | less than ½ of 1% |
|
73. Characterize intradural disc herniation. |
| G7 p.455:100mm |
a. What is the incidence? | 0.04 to 1.1% |
|
b. Can it be diagnosed preoperatively? | rarely |
|
c. It is suspected at surgery because of a_____ _____. | negative exploration |
|
d. Does it require a surgical dural opening? | rarely |
|
74. Characterize juxta facet cysts (JFCs). |
| G7 p.456:50mm |
a. What are the types? |
|
|
i. s_____ | synovial |
|
ii. g_____ | ganglion |
|
b. What is the incidence? | rare (1/500 spinal CTs) |
|
c. Key to diagnosis on myelography or post-myelogram cat scan PMCT is a p_____f_____d_____. | posterolateral filling defect |
|
d. Is it uni-or bilateral? | may be bilateral |
|
e. Does juxta facet cysts suggest stability or instability to the spine? | check for stability—may serve as a marker of instability | |
75. Regarding failed back syndrome, the failure rate for lumbar discectomy is_____%. | 8 to 25% | G7 p.457:120mm |
76. True or False. Regarding failed back syndrome, the following is the best test for detecting residual or recurrent disc herniation: |
| G7 p.459:45mm |
a. myelography with postmyelogram CT scan | false |
|
b. CT scan with infusion | false |
|
c. MRI without and with IV gadolinium | true |
|
d. unenhanced MRI | false |
|
77. Answer the following about arachnoiditis: |
| G7 p.459:55mm |
a. What test is used to differentiate residual or recurrent disc herniation from scar tissue and adhesive arachnoiditis? | MRI without and with IV gadolinium |
|
b. Why is it so important to differentiate? Because surgical treatment for scar has_____. | poor results for scar tissue or adhesive arachnoiditis |
|
78. Characterize recurrent herniated disc. |
| G7 p.460:90mm |
a. second herniation_____% | 3 to 19% |
|
b. 10 years same level_____% | 4% |
|
c. 1 year same level_____% | 1.5% |
|
d. second recurrence_____% | 1% |
|
79. Does it take a larger or smaller disc herniation to cause symptoms in recurrent disc? Why? Because_____ _____ prevents the nerve from moving away. | smaller; scar tissue | G7 p.460:110mm |
80. Where does the cervical root exit in relation to the pedicle? | in close relation to the undersurface of the pedicle | G7 p.461:42mm |
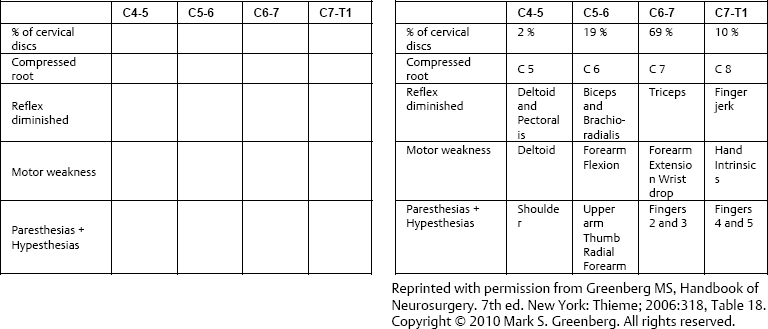
81. Complete the following table concerning cervical disc syndromes: |
| G7 p.461:60mm |
| ||
Table 18.1 |
| |
82. Complete the following about intervertebral disc herniation: |
| G7 p.461:70mm |
a. C6-7 disc causes a C_____ radiculopathy. | C7 |
|
b. C5-6 disc causes a C_____ radiculopathy. | C6 |
|
c. It may simulate a _____. | myocardial infarction | G7 p.461:110mm |
83. A left C6 radiculopathy can simulate an _____ _____ _____. | acute myocardial infarction | G7 p.461:110mm |
84. C8 or T1 nerve root involvement (i.e., a C7-T1 or T1-T2 disc) may produce _____. | a partial Horner syndrome | G7 p.461:115mm |
85. The most common scenario for patients with herniated cervical discs is that the symptoms were first noticed upon _____. | awakening in the morning (without identifiable trauma and stress) | G7 p.461:120mm |
86. Complete the following about intervertebral disc herniation: |
| G7 p.461:60 Table 18.18 |
a. C 4-5 disc compresses C _____ root _____. | C5 root exiting |
|
b. L 4-5 disc compresses L _____ root _____. | L5 root passin |
|
87. Narrowing the cervical foramen mechanically is called _____ _____. | Spurling sign | G7 p.461:180mm |
88. Complete the following about the Spurling sign: |
| G7 p.461:181mm |
a. performed by |
|
|
i. examiner exerting pressure on the _____ | vertex |
|
ii. while patient tilts head toward the _____ _____ | symptomatic side |
|
iii. with neck _____ | extended |
|
b. reproduces _____ _____ | radicular pain |
|
c. analogous to _____ | SLR for lumbar disc— a mechanical sign |
|
89. Give the accuracy of radiological workups. |
| G7 p.462:58mm |
a. MRI is _____%. | 85 to 90% |
|
b. CT myelogram is _____%. | 98% | G7 p.462:83mm |
90. True or False. To fuse or not to fuse. Fusion is beneficial to |
| G7 p.464:15mm |
a. a plate reduces pseudoarthrosis | true |
|
b. a plate reduces graft problems | true |
|
c. a plate maintains lordosis | true |
|
d. improve clinical outcome | false |
|
e. improve arm pain | true |
|
f. provide more rapid relief of arm pain | true | |
g. maintain foraminal height | false |
|
h. maintain disc space height | false |
|
i. reduce post op kyphosis | true |
|
j. improve fusion rate | true |
|
91. What is the incidence of vocal cord paresis due to injury of the recurrent laryngeal nerve (RLN)? |
| G7 p.465:45mm |
a. Temporary _____% | 11% |
|
b. Permanent _____% | 4% |
|
92. True or False. A good way to treat vertebral artery injury is by |
| G7 p.465:70mm |
a. packing | false |
|
b. direct suture | true |
|
c. endovascular trapping | true |
|
93. The rare complication of sleep-induced apnea can occur with anterior cervical discectomy and fusion (ACDF) at the level of_____. | C3-4 | G7 p.465:140mm |
94. Characterize dysphagia following ACDF. |
| G7 p.466:80mm |
a. Incidence early is_____% | 60% |
|
b. At 6 months only_____% | 5% |
|
c. Most serious cause is_____ | hematoma |
|
d. Prmanent recurrent laryngeal nerve injury_____% | 1.3% |
|
95.Characterize pseudoarthrosis following ACDF. On flexion extension cervical spine x-rays |
| G7 p.467:60mm |
a.movement of more than_____ mm | 2 |
|
b.between the_____ _____ | spinous processes |
|
c. lack of _____ across the fusion | trabeculation |
|
d. I _____ around the screws | lucency |
|
e. t_____ of the screws on flexion extension films | toggling |
|
f. n _____uniformly associated with symptoms | not |
|
96. For patients in certain professions we prefer to do posterior cervical surgery instead of anterior. |
| G7 p.468:125mm |
a. Which two professions? | speaker and singer |
|
b. The reason is there is a _____% | 5% |
|
c. incidence of _____ _____ after anterior cervical surgery. | voice change |
|
97. Indications for posterior keyhole laminotomy are |
| G7 p.469:95mm |
a. s_____ l _____d_____ | soft lateral disc |
|
b.occupation of s_____ or s_____ | singer or speaker |
|
c. l _____- or u _____-l _____ d _____ | lower- or upper-level disc | |
98. Matching. Match the recommended sequence of bone removal with the recommended sequence for posterior keyhole laminotomy. |
| G7 p.470:20mm |
Sequence of bone removal recommended: |
|
|
|
|
|
a. 1st area of bone removal |
|
|
b. 2nd area of bone removal |
|
|
c. 3rd area of bone removal |
|
|
99. The success rate of posterior keyhole laminectomy is in the range of _____ to _____%. | 90 to 96 | G7 p.470:150mm |
100. Characterize thoracic disc herniation. |
| G7 p.470:173mm |
a. It usually occurs below the level of | T8 |
|
b. Because many are calcified it is wise to geta _____ _____. | CT scan |
|
101. Characterize thoracic disc herniation. |
| G7 p.471:12mm |
a. The incidence is _____% of all disc herniations. | 0.25 to 0.75% |
|
b. _____% occur between ages 30 and 50. | 80% |
|
c. Historyof trauma is _____%. | 25% |
|
102. Characterize access to the thoracic spine. |
| G7 p.471:130mm |
a. upper _____ | sternal splitting |
|
b. mid _____ | right thoracotomy (heart not in way) |
|
c. lower _____ | left-easier to mobilize aorta than vena cava |
|
d. thoracolumbar _____ | right to avoid liver unless pathology is far on left side |
|
e. lumbar _____ | pathology is far on left side transabdominal |
|
103. Complete the following concerning the thoracic spine and spinal cord anterior access to: |
| G7 p.471:130mm |
a. lower thoracic spine |
|
|
i. use _____ side thoracotomy | left |
|
ii. avoid _____ _____ easier to mobilize | vena cava |
|
iii. _____ | aorta |
|
b. thoracolumbar spine |
|
|
i. use _____ side retroperitoneal approach | right |
|
ii. thereby avoiding _____ | liver |
|
 Degenerative Disc/Spine Disease
Degenerative Disc/Spine Disease
104. For each of the letters listed give the indicated number of terms that collectively describe the pathology of degenerative disc/spine disease. |
| G7 p.474:175mm |
a. D-3 | D dessication disruption disc herniation |
|
b. E-0 | E |
|
c. G-1 | G growth of fibrous tissue/joint laxity |
|
d. E-0 | E |
|
e. N-1 | N narrowing disc space |
|
f. E-0 | E |
|
g. R-1 | R resorption of disc |
|
h. A-1 | A annular tears |
|
i. T-1 | Ttorn annulus |
|
j. I-1 | I isthmic spondylolisthesis |
|
k. V-1 | V vertebral body osteophytes |
|
l. E-0 | E |
|
m. S-1 | S spondylosis |
|
n. P-1 | P proteoglycan |
|
o. I-1 | I interarticular (PARS) defects |
|
p. N-1 | N mucoid degeneration |
|
q. E-0 | E |
|
105. Complete the following about degenerative disc/spine disease: |
| G7 p.475:130mm |
a. Spondylolisthesis or anterior subluxation of one vertebral body on another is graded according to the percent of _____; therefore, it has |
|
|
b. grades |
|
|
i. I _____% | <25% |
|
ii. II _____% | 25 to 50% |
|
iii. III _____% | 50 to 75% |
|
iv. IV _____% | 75% to complete |
|
106. Complete the following about degenerative disc/spine disease: |
| G7 p.475:145mm |
a. True or False. It is common for listhesis to cause root compression. | false |
|
b. If it does do so it compresses the nerve root that _____ at that level | exits |
|
c. below the _____ above | pedicle |
|
d. compressed by the _____ _____ | superior articular facet |
|
e. being displaced _____. | upward | |
107. What is a pseudo disc? |
| G7 p.475:150mm |
a. It is the appearance on _____ | MRI |
|
b. in a patient with _____. | listhesis |
|
c. More correctly considered a _____ of the disc | “roll out” |
|
d. termed _____ by the radiologist. | “uncovered” |
|
108. What congenital condition is associated with spinal stenosis? | achondroplastic dwarfism | G7 p.477:50mm |
109. True or False. Cervical and lumbar stenosis occurs simultaneously in what % of patients? |
| G7 p.477:60mm |
a. 5% | true |
|
b. 10% | false |
|
c. 15% | false |
|
d. 20% | false |
|
110. What level is most commonly the site of lumbar stenosis? | L4-5 and then L3-4 | G7 p.477:110mm |
111. Matching. Match the condition with the appropriate clinical feature(s). |
| G7 p.477:165mm |
Clinical feature: |
|
|
|
|
|
a. neurogenic claudication |
|
|
b. vascular claudication |
|
|
c. trochanteric bursitis |
|
|
112. What posture may elicit pain in lumbar stenosis? | hyperextension | G7 p.478:100mm |
113. Give the normal lumbar spine CT measurements for each of the following: |
| G7 p.479:160mm |
a. anteroposterior (AP) diameter _____ | < 11.5 mm |
|
b. ligamentum flavum thickness _____ | < 4 to 5 mm |
|
c. height of lateral recess _____ | >3 mm |
|
114. State the AP diameter of the spine on plain films. |
| G7 p.479:160mm |
a. normal lumbar spine, lower limits of normal _____ | 15mm |
|
b. cervical spine, lower limits of normal _____ | 12 mm or less | G7 p.136:133mm |
c. lumbar severe stenosis | less than 11 mm |
|
d. cervical severe stenosis | less than 10 mm | |
115. Is treatment for asymptomatic moderate stenosis at adjacent levels appropriate? | yes (They have a likelihood of progressing to become symptomatic.) | G7 p.481:153mm |
116. What percent of patients who undergo decompressive lumbar laminectomies develop instability? | 1% | G7 p.483:40mm |
117. Spinal stability is influenced by Hint: fads |
| G7 p.483:52mm |
a. amount of remaining _____ | facet: unstable if more than one third or one half facet is removed |
|
b. patient’s _____ | age: more unstable in younger patient after decompression |
|
c. violation of _____ space | disc: intact disc space more stable |
|
d. decompression _____ | surgery: produces instability in 1 % of patients |
|
118. Matching. Following decompression in a patient, which procedures are appropriate? |
| G7 p.483:103mm |
|
|
|
|
|
|
|
|
|
a. no instability preop |
|
|
b. instability preop |
|
|
c. spondylolisthesis preop |
|
|
119. Give the lumbar spinal stenosis outcomes. |
| G7 p.484:48mm |
a. mortality _____% | 0.32% |
|
b. superficial infection _____% | 2.3% |
|
c. deep infection _____% | 5.9% |
|
d. deep vein thrombosis (DVT) _____% | 2.8% |
|
e. postural pain relief _____% | 96% |
|
f. recurrence after 5 years_____ % | 27% |
|
g. long-term success at 1 year and 5 years _____% | 70% |
|
120. Non-union risk factors include |
| G7 p.484:60mm |
a. s _____ | smoking |
|
b. number of _____ fused | levels |
|
c. use of _____type medications | NSAIDs |
|
121. Characterize lateral recess stenosis. |
| G7 p.485:17mm |
a. Is the pain unilateral or bilateral? | can be either |
|
b. It is due to _____ of the | hypertrophy |
|
c. _____ _____ facet. | superior articular |
|
d. The most common level is at _____ | L4-5 | |
122. Give the dimensions of lateral recess onCT. |
| G7 p.485:92 mm |
a. lateral recess height_____ mm | 3 to 4 mm |
|
b. suggestive of lateral recess narrowing _____ mm | <3 mm |
|
c. diagnostic of lateral recess syndrome _____ mm | <2 mm |
|
123. Complete the following about degenerative disc/spine disease: | G7 p.488:100mm | |
a. What reflex test is said to be pathognomonic of cervical spinal myelopathy? | inverted radial reflex |
|
b. Elicited by performing the _____ _____ | brachioradialis reflex |
|
c. and obtaining a response of _____ | flexion of the fingers |
|
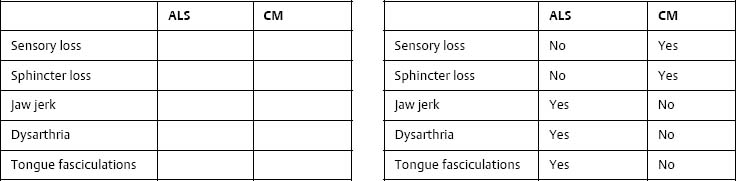
124. Complete the following regarding hyperactive jaw jerk: |
| G7 p.488:118mm |
a. significance is that it indicates an |
|
|
i. u_____ m _____ n _____ l_____ | upper motor neuron lesion |
|
ii. located a_____ t _____ p _____ | above the pons (It distinguishes this from UMN lesions due to lower-level causes, i.e., cervical myelopathy.) |
|
b. helps differentiate what diseases? |
|
|
i. _____ from | ALS from |
|
ii. _____ _____ | cervical myelopathy |
|
125. Complete the following table to differentiate amyotrophic lateral sclerosis (ALS) from cervical myelopathy: |
| G7 p.489:75 mm |
| ||
126. True or False. Concerning ALS: |
| G7 p.489:75mm |
a. Jaw jerk is present. | true (may be first clue) |
|
b. Tongue fasciculations are present. | true (as seen on EMG or visible fasciculations) | |
127. Complete the following about degenerative disc/spine disease: |
| G7 p.489:145mm |
a. cervical spine myelopathy spinal canal diameter |
|
|
i. myelopathic at_____ mm | 10 mm or less |
|
ii. symptomatic at_____ mm | 11.8 mm |
|
iii. increased risk at_____ mm | 14.0 mm |
|
b. not symptomatic at_____ mm or more | 14 mm |
|
128. True or False. Regarding MRI abnormalities that correlate with poor prognosis in cervical spondylitic myelopathy: |
| G7 p.490:15mm |
a. T2W1 hyperintensity within the cord | true |
|
b. Spinal cord transverse area less than 60mm2 | false |
|
c. Spinal cord transverse area less than 45 mm2 | true |
|
d. “Snake eyes” on axial T2W1 | true |
|
129. True or False. Preop SSEP testing can aid in decision making. | true | G7 p.490:120mm |
130. Contraindications to posterior decompression are |
| G7 p.492:23mm |
a. kyphotic angulation, also known as | swan neck |
|
b. subluxation of greater than_____ mm | 3.5 mm |
|
c. or rotation in the sagittal plane of more than_____ degrees. | 20 degrees | G7 p.492:65mm |
131. Characterize cervical sprodylitic myelopathy. |
| G7 p.493:100mm |
a. Postop palsy sfter anterior or posterior | 3 to 5% |
|
b. It involves the d_____ or b_____ muscles | deltoid, biceps |
|
c. and C5 region; that is_____ area sensory symptoms. | shoulder |
|
d. It usually occurs within_____ of surgery. | 1 week |
|
e. Prognosis for recovery is_____. | good |
|
 Craniovertebral Junction and Upper Cervical Spine Abnormalities
Craniovertebral Junction and Upper Cervical Spine Abnormalities
132. Name 13 causes of craniovertebral abnormalities. |
| G7 p.494:40mm |
Hint: attaCK roMinDs |
|
|
a. a_____ | ankylosing spondylitis |
|
b. t_____ | trauma |
|
c. t_____ | tumor |
|
d. a_____ | atlantoaxial dislocation |
|
e. C_____ | Chiari malformation |
|
f. K_____ | Klippel-Feil |
|
g. r_____ | rheumatoid arthritis |
|
h. o_____ | occipitalization of the atlas |
|
i. M_____ | Morquio syndrome (a mucopolysaccharidosis) |
|
j. i_____ | infection |
|
k. n_____ | neoplasm |
|
l. D_____ | Down syndrome |
|
m. s_____ | surgery (transoral odontoidectomy) |
|
133. What are some of the abnormalities at the craniocervical junction? |
| G7 p.494:90mm |
Hint: baaoa |
|
|
a. b_____ i_____ | basilar impression |
|
b. a_____ -o_____ d_____ | atlanto-occipital dislocation |
|
c. a_____ d_____ | atlantoaxial dislocation |
|
d. o_____ of the a_____ | occipitalization of the atlas |
|
e. a_____ p_____ a_____ of CI | absent posterior arch |
|
 Rheumatoid Arthritis
Rheumatoid Arthritis
134. Name four upper cervical spine abnormalities associated with rheumatoid arthritis. |
| G7 p.494:170mm |
a. b_____ i_____ | basilar impression |
|
b. a_____ s_____ | atlantoaxial subluxation |
|
c. s_____ s_____ | subaxial subluxation (less common) |
|
d. v_____ a_____ i_____ | vertebral artery insufficiencydue to changes at the craniocervical junction (less common) | |
135. What are the three stages in pathophysiology that lead to atlantoaxial subluxation in rheumatoid arthritis? |
| G5 p.495:50mm |
Hint: iel |
|
|
a. infl_____ at a_____ s_____ j_____ | inflammation at atlantoaxial synovial joints |
|
b. ero_____ c_____ in o_____ | erosive changes in odontoid |
|
c. loo_____ of the t_____ | loosening of the transverse |
|
I_____ | ligament |
|
136. What percentage of rheumatoid arthritis patients develop subluxation? | Atlantoaxial subluxation occurs in 25% of patients with rheumatoid arthritis. | G5 p.495:60mm |
137. Complete the following regarding atlantoaxial subluxation in rheumatoid arthritis: |
| G7 p.495:125mm |
a. The odontoid C1 interval is normal when less than_____ mm. | 4 mm |
|
b. The asymptomatic patient needs surgery if distance is greater than_____ mm. | 8 mm |
|
c. To do transoral odontoidectomy the mouth needs to open at least_____ mm. | 25 mm |
|
d. Mortality of C1-C2 wiring is_____%. | 5 to 15% |
|
138. Characterize posterior atlantodental interval (PADI). |
| G7 p.495:135mm |
a. Correlates with the presence of _____ | paralysis |
|
b. Predicts neurologic recovery following _____ | surgery |
|
c. No recovery occurs if the PADI is less than_____ mm | 10 |
|
d. An indication for surgery is a PADI less than_____ mm | 14 |
|
139. What degree of atlantodental interval is a generally accepted surgical indication in asymptomatic patients? | 8 mm (6 to 10 mm is the range) | G7 p.496:60mm |
140. What is the percentage of nonfusion for C1-C2 fusions in rheumatoid arthritis? | 18 to 50% | G7 p.496:160mm |
141. Characterize basilar impression in rheumatoid arthritis. |
| G7 p.497:30mm |
a. Changes in lateral masses are called e_____ | erosive |
|
b. Permitting relationship of C1-C2 to change is called t_____. | telescoping |
|
c. Position of dens moves u_____ | upward |
|
i. causes compression of p_____ and m_____ | pons and medulla |
|
ii. compression contributed to by p_____ | pannus |
|
iii. located_____ to dens | posterior | |
142. Matching. List the most common symptoms and signs of basilar impression of patients with rheumatoid arthritis and match with their order of frequency. |
| G7 p.497:65mm |
|
|
|
a. limb paresthesias_____% |
|
|
b. Babinski, hyperreflexia_____% |
|
|
c. bladder incontinence/retention_____% |
|
|
d. cranial nerve dysfunction_____% |
|
|
e. headache_____% |
|
|
f. ambulatory problems_____% |
|
|
143. Characterize basilar impression in rheumatoid arthritis. |
| G7 p.797:65mm |
a. Pain may be a result of_____of C1 and C2 nerves. | compression |
|
b. Cranial nerve dysfunction results from compression of the_____. | medulla |
|
144. What is the treatment for basilar impression? |
| G7 p.497:175mm |
a. if reducible with_____ | traction |
|
i. C1 d_____l_____ followed by | decompressive laminectomy |
|
ii. o_____-c_____f_____ | occipital-cervical fusion |
|
b. in nonreducible patients |
| |
i. t_____o_____r_____followed by | transoral odontoid resection followed by |
|
ii. o_____-c_____f_____ | occipital-cervical fusion |
|
 Paget Disease
Paget Disease
145. Characterize Paget disease. |
| G7 p.498:130mm |
a. Also known as o_____d_____ | osteitis deformans |
|
b. Disorder of o_____ | osteoclasts |
|
c. Results in r_____of bone | resorption |
|
d. Reactive osteoblasts o_____produce | over |
|
e. Sclerotic, radiodense, brittle bone called i_____ b_____ | ivory bone |
|
146. Recommended laboratory tests include |
| G7 p.499:100mm |
a. a_____ ph_____ | alkaline phosphatase |
|
b. ur_____ hy_____ | urinary hydroxyproline |
|
c. bone scan _____ _____ areas of abnormality | lights up |
|
d. and treatment with c_____ | calcitonin | |
147. What are the neurosurgical indications in Paget disease of the spine? |
| G7 p.501:95mm |
a. spinal _____ | instability |
|
b. uncertain _____ | diagnosis |
|
c. failure of _____ _____ | medical management |
|
 Ankylosing Spondylosis
Ankylosing Spondylosis
148. Characterize ankylosing spondylosis. |
| G7 p.502:45mm |
a. It is also known as M_____S_____d_____. | Marie Strümpell disease |
|
b. Locus of involvement is the _____ | entheses |
|
c. replacement of _____ with _____. | ligaments with bone |
|
d. Bone is very_____. | osteoporotic |
|
e. On x-ray it is called_____ _____. | bamboo spine |
|
f. To differentiate from rheumatoid arthritis (RA) serum is _____for _____ _____. | negative for rheumatoid factor |
|
g. Fracture may occur with _____ _____. | minimal trauma |
|
h. Screws for fusion may _____ _____. | not hold |
|
i. Enthesis |
| G7 p.502:60mm |
i. is the _____ _____ | attachment point |
|
ii. of ligaments, tendons or capsules on_____ | bones |
|
149. What are radiologic considerations in ankylosing spondylosis? |
| G7 p.503:15mm |
a. Rotary_____may occur in high cervical area. | subluxation |
|
b. Last area to stay mobile is the o_____-a_____ | occipito-atlanto |
|
c. and a_____joints. | atlantoaxial |
|
d. Minor trauma may result in spine_____. | fracture |
|
e. Vertebral fractures occur through the _____ _____. | ossified disc |
|
f. An early site of involvement is the_____ _____. | Sl joint |
|
g. If suspicious, x-ray the_____ _____. | entire spine |
|
 Ossification of the Posterior Longitudinal Ligament
Ossification of the Posterior Longitudinal Ligament
150. Insert a term starting with the indicated letter to characterize the pathologic process of ossification of the posterior longitudinal ligament (OPLL). |
| G7 p.504:77mm |
a. c_____ | calcification |
|
b. d_____ | dura |
|
c. e_____ | evolves from C34 |
|
d. f_____ | fibrosis |
|
e. g_____ | grows 0.6 mm and 4.1 mm/year |
|
f. h_____ | hypervascular |
|
g. p_____ | periosteal |
|
h. o_____ | ossification |
|
151. True or False. OPLL progresses in the following order: |
| G7 p.504:78mm |
1. ossification |
|
|
2. fibrosis |
|
|
3. calcification |
|
|
a. 1,3,2 | false |
|
b. 2,1,3 | false |
|
c. 3,1,2 | false |
|
d. 2,3,1 | true |
|
152. OPLL grows at a rate of |
| G7 p.504:90mm |
a. _____mm in the anterior posterior (AP)direction and | 0.6 mm |
|
b. _____mm longitudinally per year | 4.1 mm |
|
153. Provide the pathologic classification. |
| G7 p.504:125mm |
a. Confined to space behind vertebral body. | segmental |
|
b. Extends from body to body spanning disc is called_____. | continuous |
|
c. Combines both of the above and has skip areas is called_____. | mixed |
|
154. Describe the evaluation of OPLL. |
| G7 p.504:175mm |
a. Plain x-rays_____ _____ to demonstrate OPLL. | often fail |
|
b. |
|
|
i. MRI: OPLL is difficult to appreciate until it is_____ mm thick. | 5mm |
|
ii. T2W1 may be very_____. | helpful |
|
c. CT, especially with 3D reconstruction, is the_____ method. | best | |
155. List the clinical grading of OPLL. |
| G7 p.505:30mm |
a. class 1 | x-ray only—radiographically evident; no symptoms or signs |
|
b. class 2 | minimal—myelopathy A/O radiculopathy minimal or stable deficit |
|
c. class 3A | myelopathy—moderate to severe myelopathy |
|
d. class 3B | quadriplegia—moderate to severe quadriplegia |
|
156. Complete the following regarding Nurick grades of cervical spondylosis: |
| G7 p.505:82mm |
a. Assess the extent of_____. | disability |
|
b. Surgery showed no benefit for Nurick grades_____and_____. | 1 and 2 |
|
c. Surgery was valuable for Nurick grades_____and_____. | 3 and 4 |
|
d. Surgery was ineffective for Nurick grade_____. | 5 |
|
 Diffuse Idiopathic Skeletal Hyperostosis
Diffuse Idiopathic Skeletal Hyperostosis
157. Characterize diffuse idiopathic skeletal hyperostosis (DISH). |
| G7 p.506:83mm |
a. Areas of spine affected by % |
|
|
i. thoracic_____% | 97% |
|
ii. lumbar_____% | 90% |
|
iii. cervical_____% | 78% |
|
iv. all three segments_____% | 70% |
|
b. Area spared | sacroiliac joints |
|
c. Is the area spared in ankylosing spondylitis? | no |
|
 Scheuermann’s Kyphosis
Scheuermann’s Kyphosis
158. Complete the following regarding Scheuermann’s Kyphosis: |
| G7 p.506:158mm |
a. Which age group does it affect? | adolescents |
|
b. It is defined as |
|
|
i. _____wedging | anterior |
|
ii. of at least_____degrees | 5 |
|
iii. of_____or more_____ | 3; adjacent |
|
iv. _____vertebral bodies. | thoracic |
|
 Spinal Arteriovenous Malformation
Spinal Arteriovenous Malformation
159. Characterize spinal AVM classification. |
| G7 p.507:65mm |
a. Type 1 |
|
|
i. known as_____ _____ | dural AVM |
|
ii. IA: has_____ _____ arterial feeder | a single |
|
iii. IB: has_____or_____ arterial feeders | 2 or more |
|
iv. Formed at the_____ _____sleeve | dural root |
|
b. Intradural AVMs |
| |
i. Flow is_____ | high |
|
ii. _____% with acute symptoms | 75% |
|
c. Type II |
|
|
i. aka spinal_____ AVM | glomus |
|
ii. located_____ | intramedullary |
|
iii. true_____of the cord | AVM |
|
iv. has a_____ _____ | compact nidus |
|
v. prognosis is_____than dural AVM | worse |
|
d. Type III |
|
|
i. aka_____ spinal AVM | juvenile |
|
ii. essentially on enlarged_____ | glomus |
|
iii. occupies_____ _____ cross section | the entire |
|
e. Type IV |
|
|
i. aka_____ spinal AVM | perimedullary |
|
ii. aka_____ fistula | arteriovenous |
|
iii. presents with_____hemorrhage | catastrophic |
|
160. What is the most common type of spinal AVM? |
| G7 p.507:70mm |
a. type_____ | type 1 |
|
b. dural_____ | AVM |
|
c. fed by a_____ | dural artery |
|
d. and draining into a_____ | spinal vein |
|
e. on the_____ aspect of the cord | posterior |
|
f. _____% are males | 90 |
|
161. What is the most common presentation of a spinal AVM? |
| G7 p.508:80mm |
a. onset of_____ | back pain |
|
b. progressive lower extremity_____ and_____ | weakness and sensory loss—acute onset of back pain associated with progressive LE weakness and sensory loss (may be over months to years) | |
162. Spinal AVM with pain may have this syndrome. |
| G7 p.508:90mm |
a. Patient with onset of subarachnoid hemorrhage (SAH), and sudden excruciating back pain is also called c_____ d_____ p_____ of Michon. | coup de poignard |
|
b. This is considered clinical evidence of_____ _____. | spinal AVM |
|
163. What is Foix-Alajouanine syndrome? |
| G7 p.508:95mm |
a. acute or subacute_____ _____ | neurologic deterioration |
|
b. in a patient with a_____ _____ | spinal AVM |
|
c. without evidence of_____ | hemorrhage |
|
d. caused by_____ _____ | venous hypertension |
|
e. with secondary_____ | ischemia |
|
 Spinal Meningeal Cyst
Spinal Meningeal Cyst
164. What is a Tarlov cyst? | spinal meningeal cyst | G7 p.509:97mm |
165. What are the different types of spinal meningeal cyst, and which compartment are they located in? |
| G7 p.509:110mm |
a. type I | superficial compartment extradural without root fibers |
|
b. type II | middle compartment extradural with spinal root fibers—diverticulum |
|
c. type III | central compartment intradural arachnoid cyst |
|
166. Complete the following statements about spinal meningeal cyst: |
| G7 p.509:120mm |
a. Type II spinal meningeal cyst is also known as_____ _____. | Tarlov cyst |
|
b. It occurs on the_____ roots. | dorsal |
|
167. What are the treatment options for spinal meningeal cyst? |
| G7 p.510:40 mm |
a. e_____ | excise the cyst |
|
b. o_____ | obliterate the ostium between cyst and subarachnoid space |
|
c. m_____ | marsupialize if excision is not possible |
|
 Syringomyelia
Syringomyelia
168. Complete the following about syringomyelia: |
| G7 p.510:75mm |
a. _____cavitation of the spinal cord | cystic |
|
b. associated with Chiari I in_____% | 70% |
|
c. affects upper or lower extremities first? | upper |
|
d. More rapid neurologic progression is predicted by a cavity more than _____mm in diameter and with associated cord_____. | 5 mm; edema |
|
169. Rostral extension into brainstem is called_____. | syringobulbia | G7 p.510:105mm |
170. Distinguish from similar entities. |
| G7 p.510:115mm |
a. Tumor cyst |
|
|
i. Most_____ | enhance |
|
ii. Fluid is_____ | proteinaceous |
|
iii. Syrinx fluid has MRI characteristics of_____ | CSF |
|
b. Residual spinal canal |
|
|
i. Central canal usually_____ | involutes |
|
ii. No more than_____ to_____mm wide | 2; 4 |
|
iii. Perfectly_____ on cross section | round |
|
iv. Perfectly in the_____ on axial MRI | center |
|
171. Dilatation of central canal with ependymal lining is called_____. | hydromyelia | G7 p.510:160mm |
172. Communicating syringomyelia is commonly associated with what congenital conditions? |
| G7 p.511:75mm |
Hint: bCDe |
|
|
a. b_____ | basilar impression |
|
b. C_____ | Chiari malformation |
|
c. D_____ | Dandy-Walker syndrome |
|
d. e_____ | ectopia of cerebellum |
|
173. What are the main presenting symptoms and signs of a syrinx? |
| G7 p.511:175mm |
Hint: accC |
|
|
a. a_____w_____ | arm/hand weakness |
|
b. c_____ s_____l_____ | sensory loss with suspended “cape” dissociated sensory loss (loss of pain and temperature with preserved joint position sense) |
|
c. c_____o_____p_____ | cervical/occipital pain |
|
d. C_____j_____p_____a_____ | Charcot joints—painless arthropathies | |
174. True or False. The level of spinal injury that has the highest incidence of posttraumatic syringomyelia is |
| G7 p.513:125mm |
a. cervical | false | G7 p.513:155mm |
b. thoracic | true | G7 p.513:163mm |
c. lumbar | false |
|
175. Characterize posttraumatic syringomyelia. |
| G7 p.514:28mm |
a. Most common symptom is_____. | pain, not relieved by analgesics |
|
b. Most common sign is_____ _____ _____. | ascending sensory level | G7 p.514:55mm |
176. What may be the only feature of descending syringomyelia in patients with complete cord lesions? | hyperhidrosis | G7 p.513:163mm |
177. Complete the following statements about syringomyelia: |
| G7 p.513:155mm |
a. What should raise the index of suspicion for a syrinx in a patient who is paraplegic from trauma? |
| |
i. The_____ development | late |
|
ii. in a_____ patient | paraplegic |
|
iii. of_____ _____ weakness. | upper extremity |
|
b. Incidence is_____. | 0.3 to 3.0% |
|
c. Latency is_____. | 3 months to 30 years |
|
178. Complete the following statements about syringobulbia: |
| G7 p.510:106mm |
a. What is a common symptom in syringobulbia? |
| |
i. p_____p_____ | perioral paresthesias |
|
ii. located_____ | bilaterally (bilateral perioral tingling and numbness) |
|
b. due to compression of_____ _____ _____ | spinal trigeminal tracts |
|
 Spinal Epidural Hematoma
Spinal Epidural Hematoma
179. What is the most common cause of spinal epidural hematoma? |
| G7 p.515:38mm |
a. _____plus | trauma (almost exclusively in patients with) |
|
b. _____ | higher bleeding tendency (anticoagulated, bleeding diathesis, etc.) | |
180. Complete the following about spinal epidural hematoma: |
| G7 p.515:15mm |
a. The most common area of occurrence is_____. | thoracic |
|
b. Is it anterior or posterior? | often posterior (which facilitates removal) |
|
c. The most common category of patient is_____. | anticoagulated |
|
181. What is the usual presentation of spinal epidural hematoma? | severe back pain (with radicular component) | G7 p.515:83mm |
 Spinal Subdural Hematoma
Spinal Subdural Hematoma
182. Complete the following regarding spinal subdural hematoma: |
| G7 p.515:150mm |
a. They occur_____. | rarely |
|
b. They are often related to_____. | trauma |
|
c. Patients are usually on_____medication. | anticoagulant |
|
d. It may sometimes be treatable_____. | conservatively |
|
 Spinal Epidural Lipomatosis SEL)
Spinal Epidural Lipomatosis SEL)
183. Characterize spinal epidural lipomatosis (SEL) |
| G7 p.516:30mm |
a. Due to_____ of epidural fat | hypertrophy |
|
b. Due to |
|
|
i. _____and/or | obesity |
|
ii. exogenous_____ | steroids |
|
c. Symptoms |
| |
i. first is_____ _____. | back pain |
|
ii. progressive_____ _____ | lower extremity |
|
iii. and_____ weakness. | sensory |
|
d. Most occur in the_____ spine. | thoracic |
|
e. Diagnose by use of_____ _____. or | CT or MRI |
|
f. Should be at least_____ mm thick to be SEL. | 7 |
|
g. Treat by |
| |
i. Reduce the use of_____ or_____. | steroids |
|
ii Lose_____. | weight |
|
iii. Remove_____. | surgically |
|
h. Complication rate is_____. | high |
|
 Coccydynia
Coccydynia
184. Answer the following about coccydynia: |
| G7 p.516:130mm |
a. True or False. It is more common in males. | false (It is more common in females.) |
|
b. Due to_____. | a more prominent coccyx (In fact, if found in males in absence of trauma, search for underlying cause should be performed.) |
|
185. What are some causes of coccydynia? |
| G7 p.516:140mm |
a. t_____ | trauma |
|
b. n_____ | neoplasm |
|
c. r_____p_____ | referred pain |
|
186. What is the primary treatment for typical coccydynia? | conservative comfort measures: nonsteroidal antiinflammatory drugs, analgesics, sitting cushion, and lumbar support for 3 months | G7 p.517:87mm |
187. What percentage of conservatively treated coccydynia will recur? | 20%; usually within first year | G7 p.517:100mm |
188. What ganglion will be targeted for blockade or neurolysis in treatment of refractory coccydynia? |
| G7 p.517:132mm |
Hint: Wilps | ||
a. Ganglion of_____, | Walther |
|
b. also known as the ganglion_____, | impar |
|
c. is the_____ganglion of the | lowest |
|
d. _____ _____, | parasympathetic chain |
|
e. just anterior to the_____ _____. | sacrococcygeal joint |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 superior facet of the vertebra below,
superior facet of the vertebra below,  inferior facet of the vertebra above,
inferior facet of the vertebra above,  lateral aspect of lamina above Recommended sequence:
lateral aspect of lamina above Recommended sequence:


 pain is dermatomal;
pain is dermatomal;  sensory loss stocking;
sensory loss stocking;  sensory loss is dermatomal;
sensory loss is dermatomal;  pain with exercise;
pain with exercise;  pain with standing;
pain with standing;  rest relieves pain promptly;
rest relieves pain promptly;  rest relieves pain slowly;
rest relieves pain slowly;  relief with standing;
relief with standing;  relief only with stooping or sitting;
relief only with stooping or sitting;  achiness over thigh; %%11 pain on pressure over hip; 8ocir12; Faber sign positive Condition:
achiness over thigh; %%11 pain on pressure over hip; 8ocir12; Faber sign positive Condition: ,
,  ,
,  ,
,  , %%7,
, %%7, 
 ,
,  ,
,  ,
, 
 , 8ocir11;, 8ocir12;
, 8ocir11;, 8ocir12; no fusion
no fusion posterolateral fusion
posterolateral fusion adding pedicle screw instrumentation
adding pedicle screw instrumentation

 ,
, 
 _____,100%;
_____,100%;  _____,80%;
_____,80%;  _____,80%;
_____,80%;  _____,71%;
_____,71%;  _____,30%;
_____,30%;  _____,22%
_____,22% 71%
71% 80%
80% 30%
30% 22%
22% 100%
100% 80%
80%
