Fig. 1.1
All structures show differences in mechanical behaviour during loading versus loading with different stress–strain curves. A part of energy which deforms the VB is not quickly available for it to return to original shape, so under repetitive loads the VB becomes unable to recover each deformation undergone, weakening until fracture. This phenomenon is referred to as hysteresis and constitutes the basis of fatigue fractures occurring under repetitive loads. Based on Bogduk [3]
It was calculated that as few as 100 cyclic loads ranging from 50 to 80 % of ultimate compression strength are sufficient to provoke endplate and subchondral bone fractures. These stresses can occur during certain normal daily activities of some individuals [4].
Endplate fractures reproduce the same physical effect as the internal disc disruption (IDD) by inducing sudden depressurization of the nucleus pulposus, overcharge of annulus and irregular distribution of loads within the disc and between adjacent endplates [5]. The concentration of load stresses within the interbody space can cause activation of peripheral nociceptors and mechanical sensitization to physiological stresses becoming painful, giving rise to discogenic pain [6].
Fatigue endplate fractures can also elicit an inflammatory repair response, which eventually extends to the matrix of underlying disc. The inflammation can be aspecific or autoimmune, primed by the exposition of disc antigens to the blood stream of vertebral vessels [7–9]. But, out from any inflammatory process, an endplate trauma could also simply alter the disc metabolism by modifying its pH and proteinases’ activity [10]. Whatever the mechanisms, it can once again abut in IDD and cause discogenic pain (Fig. 1.2).
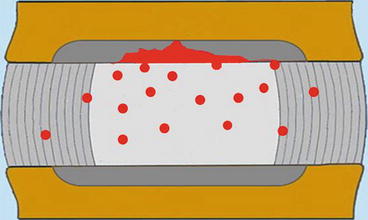
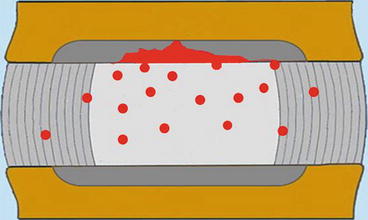
Fig. 1.2
Apart from sudden depressurization on the nucleus pulposus, endplate fractures elicit an aspecific or autoimmune-based inflammatory reaction diffusing from bone to disc matrix. Alternatively, the endplate failure can disturb the delicate homeostasis of disc metabolism creating an increased activity of metalloproteinases
Vertebral endplates present a density of innervation similar to that of a disc and, when injured, can be per se painful.
In one clinical study on a cohort of 21 patients complaining of endplate-related chronic lumbar pain diagnosed by discography, 20 reported a good outcome after fusion surgery [11].
It was calculated that endplate disruption-induced low back pain accounts for 16.7 % of all cases of chronic lumbar discogenic pain [12].
1.2 The Intervertebral Disc
Within interbody joints, the disc accepts and transmits compressive loads and is the main shock absorber of forces directed to the head and brain during walking and jumping.
Both the nucleus and inner annulus are engaged in weight bearing. The external annulus, normally subject to tensile stress, gets compressed in case of disc degeneration and nucleus dehydration, when axial loads are shifted from central endplates upon the stronger ring apophysis. Being formed by densely packed lamellae, the annulus has an intrinsic compression stiffness, but the radial pressure exerted by a compressed and expanding nucleus offers an internal bracing effect which prevents the annulus from buckling inwards, collapsing and eventually tearing, even in case of high and prolonged loads [13].
The load-bearing capacity of the disc is enhanced from the interplay between the nucleus and annulus. A young well-hydrated nucleus behaves like an uncompressible fluid body which, flattening under compression, stretches radially annulus fibres. Through annulus stretching, part of compressive forces are temporarily converted in tensile stresses for being released once load is removed, and the elastic recoil of the annulus brings back the nucleus to its original shape. The annulus distension lessens the speed of transmission of compressive forces and the risk of overcharge and damage of adjacent endplate [13].
A well-hydrated nucleus is a highly isotropic structure where the pressures are homogeneous and transmitted uniformly towards the annulus and opposite endplates. A stress profile obtained from a normal disc exhibits a very homogeneous distribution of internal hydrostatic pressure throughout the nucleus and inner annulus. With ageing, it occurs a restriction of hydrostatic nucleus occurs while it begins some concentration of compression on the posterior annulus. The disc becomes globally stiffer. A disrupted disc shows a completely depressurized nucleus and shift of compressive loads upon the annulus and facet joints [14] (Fig. 1.3).
Fig. 1.3
(a, b) Within a normally pressurized intervertebral disc, load pressures are evenly distributed on the adjacent endplates. Either the nucleus pulposus or inner annulus participate to load bearing (a). The external annulus is normally subject only to tensile stresses. With disc ageing and degeneration, compressive loads are shifted onto the external annulus corresponding to stronger apophysial rings (b)
An abnormally compressed posterior annulus can become painful, being densely innervated. Low back surgery performed on patients under local anaesthesia found it to be an important source of lumbar pain [15].
Concentration of stresses and mechanical pain can also be generated around incomplete radial annular fissures where a few residual lamellae have to resist over-increased tensile stresses [16].
Over time, the overcharge of external annulus induces the formation of marginal claw osteophytes and radial expansion of the vertebral body, as a tentative of distributing loads onto as large an area as possible, what renders spondylosis a simple age compensatory change rather than a true pathological process.
Disc anulus acts as the first ligament to restrain tridimensional motion. Differently from the nucleus, the annulus is a highly anisotropic structure.
The collagen fibres within each one of the 10–20 concentric lamellae forming the annulus run parallel at an angle of 30–35° with respect to vertebral endplates and with an alternating direction between adjacent lamellae [16, 17] (Fig. 1.4).
Fig. 1.4
The collagen fibres within each one of the 10–20 concentric lamellae forming the annulus run parallel at an angle of 30–35° with respect to vertebral endplates and with an alternating direction between adjacent lamellae
Either of the alternating arrangement of collagen fibres between adjacent lamellae and the obliquity degree in each lamella concurs to optimize the capacity of the annulus to control movements in all directions: a steeper orientation would better oppose the distraction, but reducing the resistance to sliding and twisting; a flatter direction would improve the resistance to twisting, but at detriment of that to distraction and bending.
The annulus fibres do not only surround the nucleus circumferentially but spherically, by entering and traversing superiorly and inferiorly vertebral endplates. Only the outermost fibres of the annulus insert onto the bone of the ring apophysis which replaces the peripheral endplates during development.
Both functionally and anatomically, vertebral endplates are an integrant part of a disc, while they are more loosely anchored to the VB, from which they can be fully detached in some types of traumas [18] (Fig. 1.5).
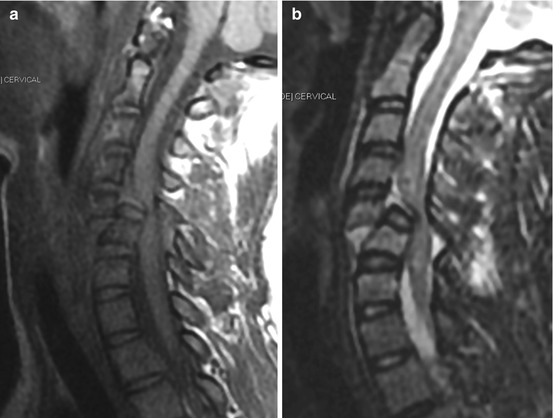
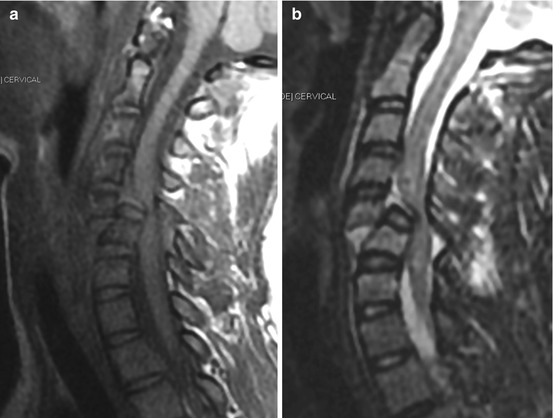
Fig. 1.5
(a, b) Translation–rotation of C5 on C6 with bilateral dislocation and fracture of facets. Sagittal FSE T1 (a) and FSE T2 (b) midline images. The inferior endplate of C5 remains quite completely attached to the subjacent intervertebral disc. Notice also the detachment of longitudinal ligaments and the sprain with oedema, of posterior complex ligaments. The spinal cord is compressed and shows large oedema, with non-evident haemorrhage
1.3 The Facet Joints
The facet joints also participate in load bearing.
According to Louis, from C2 to S1, axial loads are distributed on three columns formed by interbody and facets joints, whose contribution varies depending on the spatial orientation of the spine. In case of hyperlordosis, high and prolonged weight load and disc degeneration, the shift of loads upon the facets increases significantly [19, 20] (Fig. 1.6).
Fig. 1.6
According to the three-column concept by Louis, from C2 to S1 the vertical loads are distributed on the interbody and facet joints forming a triangle with the anterior vertex. The contribution of every column varies with spinal posture. The horizontal black lines indicate the limits of the vertical columns by the Denis concept
While the VB bears essentially compressive loads, the components of the neural arc are subject to different forces. The pedicles, in particular, form a pivot between the VB and other posterior elements which receive tensile and bending forces, the former being generated during forward vertebral sliding blocked by facets, the latter by muscle contraction which globally pulls downwards the neural arc. In both cases the forces are delivered on the thick cortical shell provoking opposite movements of distension and compression [21].
Within each MS any vertebra may perform three translations and three rotations in relation to each one of the x, y, z Cartesian axes of the space and complex movements including principal and coupled movements [22] (Fig. 1.7). The disc acts as an intervertebral spacer which allows bending movements to occur. Despite the annulus design, it being mainly designed to bear axial loads, the interbody joint lacks stability, especially for movements occurring within the horizontal plane.
Fig. 1.7
Within each MS any vertebra may perform three translations and three rotations in relation to each one of the x, y, z Cartesian axes of the space and complex movements including principal and coupled movements
The zygapophysial joints guide and restrain the movements of interbody joints. The symmetry and correct orientation of facets are the fundament for correct function and protection of disc from abnormal stress, namely, during twisting.
The intervertebral disc suffers twisting because it resists it with only half of the annulus lamellae and fibres; those having the same orientation as the torsion direction are the only ones to be stretched, while the remaining will get relaxed.
At lumbar level, facet joint angles over 45° relative to the coronal plane have been found to have a 25 times greater likelihood of developing degenerative spondylolisthesis [23].
Like for the vertebral body, in case of abnormal motion the facets also undergo a remodelling in order to increase their surface, in the form of hypertrophy and marginal osteophytes which in more extreme cases present as “wraparound bumper” osteophytes [24] (Fig. 1.8).
Fig. 1.8
CT axial scan of L5–S1 facet joints. “Wraparound bumper” osteophytes develop along the capsular insertions of facet joints and like claw osteophytes of marginal endplate represent an essay of self-stabilization
1.4 The Ligaments and Muscles
Interbody and facet joints are stabilized by a series of extrinsic ligaments.
Ligaments are the passive stabilizers of MSs and are engaged principally within the EZ, at the end points of joint excursion.
The resistance of ligament and joint capsules is expressed by a stress–strain curve which largely reflects the behaviour of the collagen fibres they contain.
During an initial phase (referred to as “toe”), the ligament undergoes relative greater elongation for the removal of its macroscopic slacking and the straightening of waved and buckled collagen fibres (crimp) it contains [25].
During the second, linear segment of the curve, the chemical bonds between collagen fibres are put in tension and begin to fail, so more energy is needed to pursue the ligament elongation.
The linear segment abut in a peak where the rupture of a great number of fibres occurs, over which elongation pursues under a lower force [25].
However, the biomechanical efficacy of a ligament depends not only on its intrinsic strength but also on the length of lever arms through which it operates, the distance between the bony insertion, the point of application of forces and the instantaneous axis of rotation (IAR), the centre of arc around which a vertebra moves in a given moment.
Ligaments located far apart from the IAR, being located within the posterior part of the vertebral body, such as the supraspinous and interspinous ligaments, stabilize forward flexion more efficaciously than the ligamenta flava and posterior longitudinal ligament.
The muscles superimpose their stabilizing action on the facets, discs, ligaments and facets.
The muscles are the active stabilizers of the spine and operate principally within the NZ where the intrinsic resistance to motion is lowest. Their action is double. A lesser mechanism consists in a direct traction on the abnormally displacing segment, but the longitudinal orientation does not consent an optimal control of horizontal movements. Indirectly, by exerting a compressive action on the spinal joints, the muscles reduce either the ROM or the NZ [26].
1.5 Stability and Instability of the Spine
Whatever the movement a vertebra performs, it has a physiological range within which the resistance and effort required change significantly.
Within the initial part of the range of motion (ROM), on either sides of neutral posture, the neutral zone (NZ), motion meets scarce resistance owing to the general laxity status of joint capsules, ligaments, fascias and tendons. The NZ is followed by an elastic zone (EZ), where the joint restraints come in tension, and the spinal stiffness, and the effort required for a given movement and the slope of load to the displacement curve increase linearly [27] (Fig. 1.9).
Fig. 1.9
The physiological ROM of any spinal joint includes an initial neutral zone where the stiffness is relatively low. The NZ is followed by an elastic zone (EZ) where for the progressive tension of capsules and ligaments at end points of joint excursion, the resistance to further motion increases very quickly. The heavy nonlinear load to displacement ratio represents the fundament of proper kinematics and stability of the spine
The change of resistance during the ROM meets the opposed necessities of performing initial movements near the neutral posture with as little muscle effort as possible, yet respecting the end points of joint excursion.
The heavy nonlinear load to displacement ratio represents the fundament of proper kinematics and stability of the spine.
The literature lacks a generally accepted definition of spinal stability.
The American Academy of Orthopaedic Surgeons defined spinal stability as the capacity of vertebrae to remain cohesive in all physiological body movements [28].
For White and Panjabi, stability is “the ability of the spine under physiologic loads to limit patterns of displacement to not damage or irritate the spinal cord and nerve roots and to prevent incapacitating deformity or pain caused by structural changes” [29].
Larson defined a stable spine being symmetrical in movement and configuration (normal or abnormal), with no changes over time [30]. This concept underlines that stability can be established or settled again during pathological conditions.
Spinal stability is the basic requirement for the protection of nervous elements and vertebral arteries, the generation of forces in the trunk and their transfer between the upper and lower limbs and the prevention of precocious biomechanical deterioration of its own components.
Panjabi theorized that stability is guaranteed by a stability system consisting of three strictly related subsystems, including the spine or passive subsystem, the muscles or active subsystem and the central nervous system (CNS) functioning as the central control unit [27, 31].
The passive subsystem plays either a structural or a transducer role.
Transducer function is carried by mechanoreceptors located within disc anulus, ligaments and joint capsules which convey proprioceptive information about the position, load status and movement of each MS to the CNS which promotes a coordinated muscle response.
Like stability, instability also lacks a generally accepted definition.
Pope and Panjabi defined instability as a loss of stiffness leading to abnormal and increased movement in the motion segments [32].
The instability, either traumatic or degenerative, is not an all or nothing phenomenon because each soft or bony spinal component contributes to stability, and in fact, the failure of all restraints and complete instability are rare [33, 34].
In many cases instability does not consist in an increase of ROM of spinal joints (terminal instability) but is based on a temporary lapse of motion control, within a normal ROM.
An MS may have most of restraints intact, but for the loss of a single restraining element, it can show a momentary looseness and a partial instability during range, and despite a normal final strength, it exhibits excessive displacement and/or abnormal acceleration during the ROM, more often within the NZ. In fact, in many traumatic injuries and degenerative disorders, the NZ modifies early and more than the ROM constituting a more reliable and sensitive index of instability.
In the light of the relative importance of the NZ, instability was defined as the reduced ability by the stabilizing system of the spine to maintain the NZs of the FSUs within physiological limits so that deformity, neurological deficit or disabling pain do not occur [27].
According to a mechanistic interpretation of spinal pain, in normal individuals there exists a pain-free zone (PFZ), within the ROM, including the NZ. In symptomatic subjects the NZ enlarges until overcoming the PFZ [35].
When an MS undergoes a failure of a restraint controlling a given phase of motion, a mismatch between displacing and restraining forces occurs that leads to an abnormal acceleration and displacement. The sudden mismatch between actual and expected movement cannot be adjusted by a proprioceptive reflex and generates a sensation of instability, felt by the patient as a “getting away”. The unexpected abnormal movement and the altered feedback it provokes elicit a sudden abnormal muscle reflex response felt as a “catch” or jerk, which eventually transforms in persistent guarded spasm in response to an overt instability [26].
It was suggested that damage to spinal ligaments and their receptors can generate abnormal proprioceptive inputs for the CNS which mediates an uncoordinated muscle response and then elicits an altered feedback reflex. With time, it may create a vicious circle leading to chronic dysfunction, muscle and joint overstress and pain [36].
Patients complaining of chronic spinal pain and dysfunction present impaired postural control, as well as repositioning errors [36].
For complex movements such as flexion–extension, formed by alternating translations and rotations, the instability can consist in a modification of the ratio between the amplitude of two components in a given phase of the ROM, a relation which otherwise remains constant during every phase of it [26].
1.6 Degenerative Instability
Spine degeneration is a very common cause of axial and radicular pain and disability.
Instability in a degenerated spine can develop when changes of vector forces in the relations between MSs generate abnormal, imbalanced, paradoxical movements [38].
An initial degenerative change primes biomechanical and motion disorders which first involves all joints of the same level (three articular complex) and then extends to that of adjacent MSs, transforming, with a domino effect, a segment in regional pathology. With time, new changes can worsen initial derangements, favouring a vicious circle by which the disease can become cyclically self-sustaining.
Despite a common statement that localization in the interbody joint of the first changes lead to degenerative instability, studies focusing upon the relation between the internal disc disruption and instability have not been performed, so, to date, there is no evidence relating degenerative instability to disc pathology.
Patients with degenerative disc disease may exhibit abnormal patterns of movement, yet have no pain, while abnormal movements occurring in a degenerated spine are not necessarily the cause of pain.
From the literature, the first descriptions of the term instability refer to a painful degenerated disc having irregular, albeit not increased, movements [39] or address a “back–gluteal–thigh” clinical triad by disc degeneration where an eventual spinal hypermobility is though “not always productive of symptoms” [40]. However, since then, the term instability evolved from being a term describing an abnormal MS due to a degenerate disc to a term denoting a diagnosis of an abnormal, or increased, pattern of motion. The abnormal movement became the cause of the pain and fusion surgery its ideal treatment, even though the unpredictable clinical results of more rigid fusions were increasingly casting doubt on the concept of instability.
Kirkaldy-Willis described three phases of degenerative instability, consisting in an initial dysfunction, an instability time and a final restabilization [41].
Instability begins with a dysfunctional time, marked by intermittent nonspecific pain, associated with initial and slight morphological changes, followed by a frank instability phase where the disc is collapsed, the annulus and ligaments become slack and redundant and subluxation of the vertebral body appears, with eventual spinal canal and foramen stenosis. At this stage pain becomes more persistent [41, 42].
Instability can so consist in a pure motion dysfunctional syndrome with no or minimal anatomical changes (microinstability), or it presents as overt forms, among which spondylolisthesis is included.
The syndromes of microinstability are classified on the basis of clinical observations, the supposed mechanism of injury and the site of lesion as well as on aggravating movements in specific directions including flexion, extension, lateral bending or multidirection. For them the diagnosis remains particularly elusive.
Microinstability lumbar syndromes present with a subjective sensation of instability felt by the patient and an objectively observed impaired muscle control. In the absence of an adequate control by segmental muscles inserting directly on the spine, patients tend to stabilize the dysfunctional MS through muscles which provide a compensatory global trunk stabilization for which high levels of intra-abdominal pressure are generated even during low-load tasks [43].
In flexion microinstability, the most frequent type, signs suggestive of altered movement control within the neutral zone are a good range of spinal mobility, but with a “painful arc” and the inability to return to erect posture from forward bending without assistance. Patients are unable to maintain semiflexed postures. A loss of lumbar lordosis during standing can be observed at the level of the unstable MS along with a greater flexion during forward bending [44].
Also for the “overt” forms of primary degenerative instability, the diagnosis is often challenging.
Patients with putative lumbar spine instability often suffer chronic or recurrent pain localized in the low back or referred to the lower extremities, with a mechanical–postural basis, being worsened by lifting, standing, sitting and bending and relieved by lying supine.
While there are no validated clinical signs for diagnosing degenerative instability, on imaging, there exists a large overlap of motion patterns between symptomatic and normal individuals, which renders difficult to state any cut-off to distinguish normality and instability [26].
For translational instability, Posner proposed a normal limit of 2.3 mm for L1–L4 vertebrae or 8 % of endplate length, and 1.6 mm, or 6 % of endplate length, for L5 [45], but many asymptomatic subjects present static disalignments in this range.
In comparison, dynamic slippages, appearing only in flexion or extension, are thought to be more reliable, but over 3 mm [46] or 4 mm [47], being the limits observed in normal people. The same cut-offs were suggested for lumbar retrolisthesis during extension which at a little extension also occurs in asymptomatic subjects [46, 47].
While retrolisthesis is primarily a disorder of disc space and prevails at L3–L4, anterolisthesis is a pathology of posterior joints and is most common at L4–L5.
Isthmic spondylolisthesis can also occur as a complication of degenerative processes, under the opposite colliding action of vertically slipped facets upon an interposed isthmus, abutting in a stress fracture [42].
Isthmic defects are thought to compromise the ability of the posterior elements to stabilize the MS, generating instability.
Spondylolisthesis is classically considered a form of instability because the degree of forward displacement can change with posture and progress over time, but more recent data mitigate this wisdom.
Some patients present forward vertebral slipping by passing from recumbency to a standing position [48], even though the pathological relevance of this finding has not been defined.
Biplanar radiographic studies detect progression of spondylolisthesis with time only rarely and in many patients revealed reduced ROM rather than instability [49].
In addition, other radiographic studies using tantalum landmarks have found no evidence of instability [50].
A 10-year follow-up study found progression of spondylolisthesis only in 30 % of cases, while 65 % of patients who were initially neurologically normal did not worsen and could be treated conservatively [51].
Open MR systems allow for positional-dynamic studies to detect increased and abnormal intersegmental movements which can worsen or uncover a spinal canal and foramen stenosis or a mobile spondylolisthesis, correlating with increased levels of pain [52, 53].
In occult and mobile forms of spondylolisthesis, static MR studies can find large joint effusions along with facet gapping (Fig. 1.10).
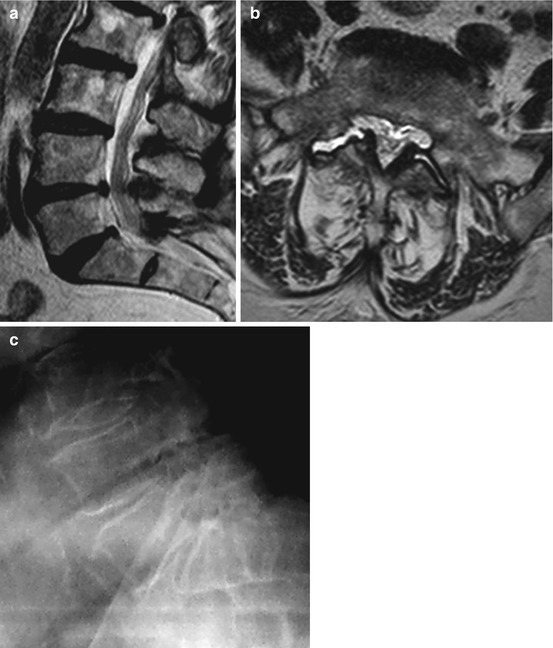
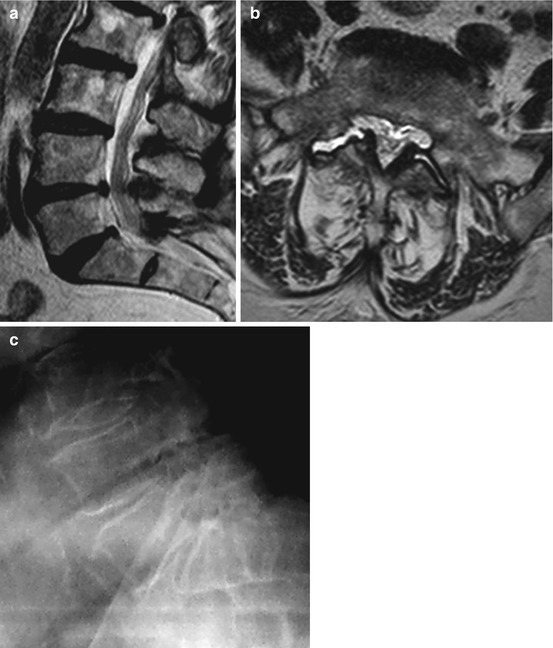
Fig. 1.10
(a–c) Even in the absence of any measurable translation on supine MRI (a FSE T2 sagittal midline image), the largest facet effusions (>1.5 mm) are highly predictive of degenerative spondylolisthesis at L4–L5 (b FSE T2 axial image of L4–L5 MS). A facet effusion >1 mm would still be an indication for dynamic radiographs or MR to diagnose an occult degenerative spondylolisthesis that can be missed with supine positioning. An anterior translation of about 20 % of endplate length appears during flexion in standing position (c)
By using open MRI, McGregor et al. investigated the kinematics of the lumbar spine in 14 symptomatic subjects with degenerative and 15 with isthmic spondylolisthesis without detecting in both cases any significant angular or translational hypermobility compared to subjects with no history of low back pain. The lack of hypermobility was considered a consequence of the increased activity of the erector spinae and multifidus muscles that may stabilize and brace the spine around the level of the defect [54].
Conversely, in a study using positional MR, it was described an instability, defined as posterior, missed by conventional radiographs, due to movements in the spondylolytic cleft and responsible for protrusion in the foramen of bony spurs, ligamenta flava or a cleft cyst, with nerve root compression [55].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








