17 Stimulation of Amygdala and Hippocampus Despite considerable advances in pharmacological therapy for epilepsy, 25 to 30% of medically treated epileptic patients continue to have seizures and are considered as pharmacoresistant.1 Resective surgery has shown its efficacy in the control of intractable seizures if presurgical evaluation clearly demonstrates a focal epileptogenic zone (EZ) that can be removed without causing unacceptable neurological deficit. Higher success has been achieved with temporal lobe epilepsy (TLE).2 However, up to 30% of TLE cases are unsuitable for surgery either because of the involvement of eloquent areas or the bilateral or multifocal nature of the ictal onset or because they show an unsatisfactory response to previous surgical treatment.3 Moreover, some patients may not have access to surgical therapy because of the limitation of human or technical resources or the high technical complexity and cost. Electrical stimulation of the brain has been proposed as an additional option to resective surgery. The first trial of epilepsy treatment by brain stimulation was made by Cooper et al in 1973,4 who reported reduction of seizure frequency by cerebellar subdural stimulation. Since the 1980s, other preliminary studies have suggested some effect on seizure frequency by stimulation of several targets among deep brain structures including the anterior thalamus,5–7 the centromedian thalamic nucleus,8–17 the caudate nucleus,18,19 the mamillary body,20,21 the subthalmic nucleus,22–24 and more recently, the amygdalohippocampal (AH) complex.25,26 Velasco et al17,25 have observed improvement over time in interictal spike as well as in seizure frequency with subacute AH high-frequency stimulation during invasive recording with depth electrodes or subdural grids. Similar effects have been reported with long-term stimulation using quadripolar electrode and implantable device.26 More recently, a prospective randomized study conducted on four patients has confirmed some long-term benefits and absence of adverse effects of hippocampal electrical stimulation in mesial TLE, although the effects were smaller than those reported earlier.27 Finally, as the mechanisms of AH stimulation have not clearly been elucidated and as this recent therapeutic issue has been proposed to a low number of patients, there are no definitive data concerning either the optimal site of implantation or the optimal implantable device properties, or even the ideal stimulation parameters. Electrical stimulation of the brain needs further, large, controlled and completed clinical trials to be definitely validated as a therapy for intractable epilepsy. However, it is an attractive and promising new treatment modality. Typical candidates for AH electrical stimulation should include intractable epileptic patients presenting with either unilateral or bilateral mesial temporal lobe epilepsy (MTLE) with one predominant side. Noninvasive tools of the presurgical evaluation (history of childhood onset epilepsy, clinical symptoms, scalp and sphenoidal electroencephalogram [EEG], video EEG, positron emission tomography [PET], single photon emission tomography [SPECT]) should clearly identify the EZ in the mesial portion of the temporal lobe.28–30 When bilateral onset is suspected, depth electrodes recording may be needed for identification of the dominant side and to rule out independent co-dominant foci. Neuropsychological testing should typically show normal interictal speech (dominant side) or spatial (nondominant side) memory function associated with severe postictal dysfunction and should be correlated with the absence of clearly identifiable hippocampal sclerosis (HS), atrophy, or hypertrophy on MRI sequences. In these patients, seizure outcome after surgery is known to be less favorable compared with patients with structural lesions such as mesial temporal sclerosis.31 Moreover, resection of mesial temporal lobe structures in these cases may be associated with a higher risk of memory impairment. When HS is visible, selective Wada test should be performed to assess the functional integrity of the hippocampus and predict memory deficits in case of hippocampal removal. Other criteria such as preexisting psychiatric illness, professional and/or psychosocial impact of memory dysfunction on patient life, and operability should be taken in consideration for the selection of the therapeutic strategy (Table 17.1). In our institution, a three-dimensional (3-D) T1-weighted MRI is performed under stereotactic conditions (we use a CRW frame, Integra Radionics, Inc., Burlington, MA) to allow computed 3-D surgical planning (FrameLink stereotactic software, Medtronic Inc., Minneapolis, MN). The approach trajectory is selected along the main axis of the hippocampus to place the contacts of the DBS electrode at the junction between the hippocampus and the parahippocampal gyrus with the distal contact located within the inferior aspect of the amygdala to avoid intraventricular trajectory (Fig. 17.1).
Indications
Operative Technique
| History of the Epilepsy | Adult Onset |
|---|---|
| Noninvasive presurgical evaluation | MTLE |
| Depth electrodes (when needed) | One predominant side with contralateral propagation |
| Absence of bilateral independant EZ | |
| MRI | No hippocampal sclerosis and/or atrophy |
| Neuropsychological evaluation | |
| Interictal | Normal or discrete memory dysfunction |
| Postictal | Severe memory dysfunction |
| Wada test (when needed) | Severe memory dysfunction homolateral to the EZ |
| Psychiatric evaluation | No associated illness |
| Professional and psychosocial impact of memory dysfunction | Severe |
Abbreviations: MTLE, mesial temporal lobe epilepsy; EZ, epileptogenic zone.
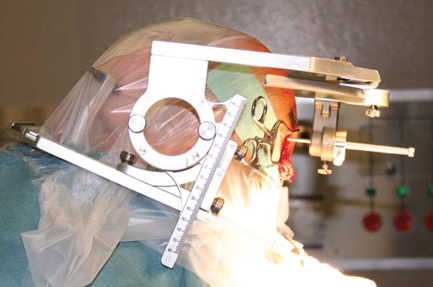
In the operating room, the patient under general anesthesia is placed in a semi-sitting position. A U-shaped skin incision is performed in the occipital region precisely determined by the entry point of the planned trajectory (Fig. 17.2). The skull is opened with a 3-mm twist-drill.
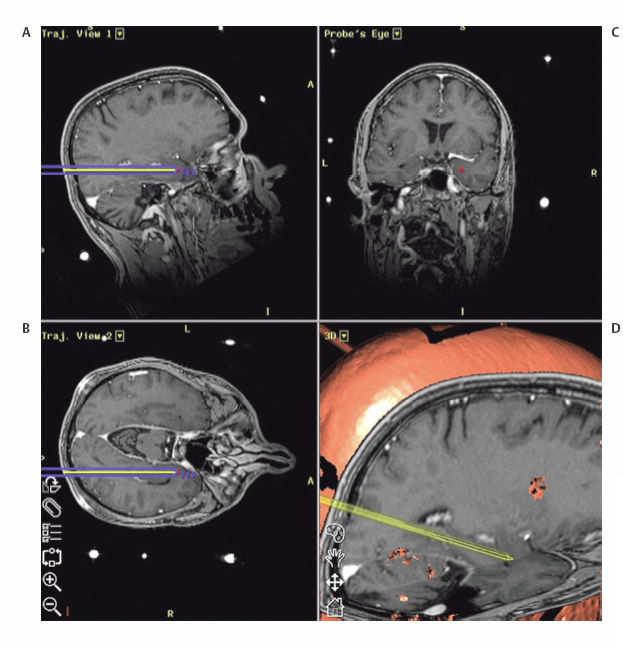
Fig. 17.1 Trajectory views of the surgic al planning (A, vertical plane; B, horizontal plane; C, perpendicular; D, 3-D) along the main axis of the hippocampus at the junction between the hippocampus and the parahippocampal gyrus (C).
The dura is carefully perforated with coagulation to avoid significant cerebrospinal fluid (CSF) leakage and the quadripolar DBS electrode (we have used so far the Pisces-Quad, Medtronic, Inc.) is implanted under lateral fluoroscopic control with the distal end in an upward direction into the amygdala (Fig. 17.3=radio).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








