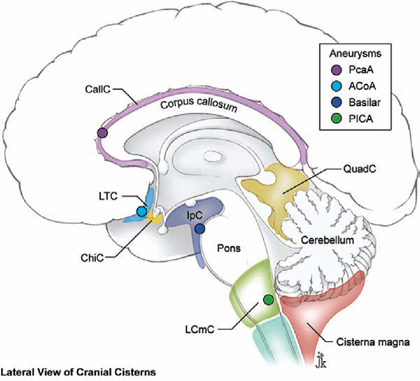
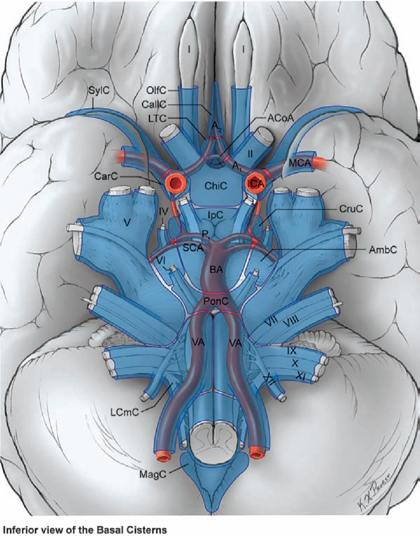
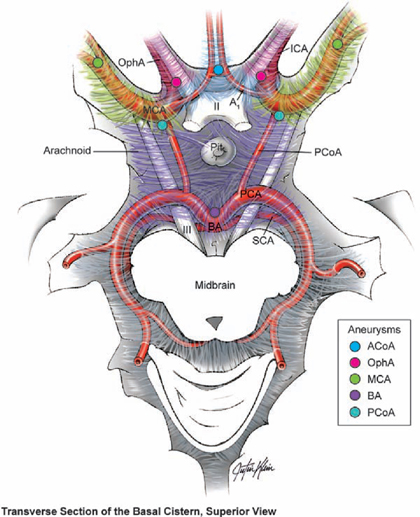
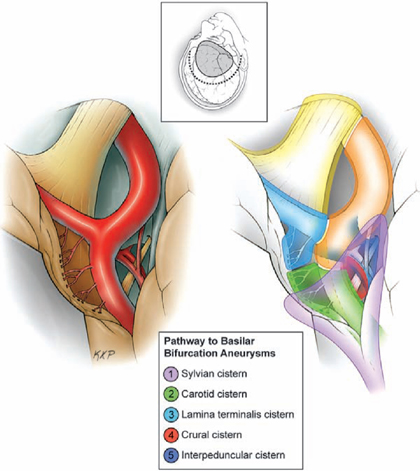
2 Subarachnoid Dissection The subarachnoid space is the arena of aneurysm surgery because it houses the brain’s arteries and provides a navigable labyrinth to deep targets that can be dissected without violating or harming the brain. Subarachnoid dissection, therefore, is a foundation of vascular neurosurgery. Fig. 2.1 Basal subarachnoid cisterns, as viewed from beneath the brain. Middle cerebral artery (MCA) aneurysms reside in the sylvian cistern; posterior communicating artery (PCoA) and ophthalmic artery (OphA) aneurysms reside in the carotid cistern; anterior communicating artery (ACoA) aneurysms reside in the lamina terminalis cistern; pericallosal artery (PcaA) aneurysms reside in the callosal cistern; basilar bifurcation aneurysms reside in the interpeduncular cistern; and posterior inferior cerebellar artery (PICA) aneurysms reside in the lateral cerebellomedullary cistern. AmbC, ambient cistern; BA, basilar artery; CallC, collosal cistern; CarC, carotid cistern; ChiC, chiasmatic cistern; CruC, crural cistern; LCmC, lateral cerebellomedullary cistern; LTC, lamina terminalis cistern; MagC, cisterna magna; OlfC, olfactory cistern; PonC, prepontine cistern; SylC, Sylvian cistern. The subarachnoid space is compartmentalized into cisterns built with sheets of arachnoid tissue, bridged by internal arachnoid trabeculations, and filled with cerebrospinal fluid (CSF) (Fig. 2.1). Subarachnoid dissection opens and interconnects these cisterns en route to an aneurysm. Intercommunication between cisterns also drains CSF and untethers lobes and lobules of brain, thereby relaxing the brain, facilitating retraction, and widening surgical corridors. Every aneurysm is associated with a cistern. Middle cerebral artery (MCA) aneurysms reside in the sylvian cistern; posterior communicating artery (PCoA) and ophthalmic artery (OphA) aneurysms reside in the carotid cistern; anterior communicating artery (ACoA) aneurysms reside in the lamina terminalis cistern; pericallosal artery (PcaA) aneurysms reside in the callosal cistern (Fig. 2.2); basilar bifurcation aneurysms reside in the interpeduncular cistern (Fig. 2.3); and posterior inferior cerebellar artery (PICA) aneurysms reside in the lateral cerebellomedullary cistern and sometimes in the cisterna magna. The pathway to some aneurysms traverses several cisterns. For example, the pathway to ACoA aneurysms progresses from carotid to chias-matic to lamina terminalis cisterns, and the pathway to basilar bifurcation aneurysms progresses from sylvian to carotid to lamina terminalis to crural to interpeduncular cisterns (Fig. 2.4). Most of an aneurysm’s initial dissection has nothing to do with the aneurysm, and instead deconstructs cisternal architecture to open fissures, separate brain surfaces, and expose normal arterial anatomy. Fig. 2.2 Midline subarachnoid cisterns, as viewed in the sagittal plane of the brain. The relationship between midline and paramedian aneurysms and their associated cisterns is shown. QuadC, quadrigeminal cistern. Fig. 2.3 Subarachnoid cisterns around the circle of Willis, as viewed from above the brain, which has been sliced axially. The relationship between aneurysms in the circle of Willis and their associated cisterns is shown. Arteries define a trail through the center of the subarachnoid space that can be dissected continuously from the cortical surface to the circle of Willis. A single cortical artery invariably guides the dissection inward to larger branches and deeper trunks. Arteries are obvious in patients with unruptured aneurysms, untainted CSF, and clear cisterns. However, arteries in patients with subarachnoid hemorrhage (SAH) are buried in dense clot and require some excavation. Clot can be evacuated safely by suctioning outward from an arterial landmark, rather than suctioning inward toward an unidentified artery. Arteries lie centrally in subarachnoid spaces and therefore define the plane of separation between pial surfaces. Larger caliber arteries are identified as the dissection deepens. The angiogram is like a trail map, and angiographic information is translated constantly to the operative field. Every artery has a safe surface to follow during subarachnoid dissection. Safe surfaces have smooth contours and few branches, whereas dangerous surfaces have perforating arteries, the aneurysm neck, or are poorly visualized (Fig. 2.5). For example, the superior surface of the M1 MCA segment gives off lenticulostriate arteries, and dissection along this surface can injure them. In contrast, the inferior surface of the M1 segment gives rise to the anterior temporal artery (ATA), which is easily seen and less vulnerable. Similarly, the superior surface of the P1 posterior cerebral artery (PCA) segment has thalamoperforators and leads directly to the neck of a basilar bifurcation aneurysm, whereas the inferior surface has no perforators. In addition, multiple perforating arteries close the dissection plane between artery and brain. Therefore, an artery’s safe surface is dissected preferentially.
 The Subarachnoid Cisterns
The Subarachnoid Cisterns
 Arterial Landmarks
Arterial Landmarks
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree