♦ Preoperative
Operative Planning
- Ensure that lateralization has been clearly determined
- Areas to be covered are discussed with epilepsy team prior to operation
- Neurophysiologist or epileptologist scheduled for electrocorticography (ECoG) recording
- Ensure epilepsy monitoring equipment is available for intraoperative use
- Ensure epilepsy monitoring unit bed available for postoperative care
- Frameless stereotaxy can be used to assist electrode placement, particularly if a neocortical lesion is present, and to facilitate central sulcus localization
- Major set-up
- High-speed drill
- Appropriate array of electrodes for intended coverage
- Electroencephalography machine
- Camera to document grid orientation
- Frameless stereotaxy (optional)
- Microscope, if interhemispheric or intrasylvian placement planned
Anesthetic Issues
- Room should be cool for mild hypothermia
- Intravenous antibiotics with skin flora coverage (cefazolin 2 g) should be given 30 min prior to incision
- Dexamethasone 10 mg intravenously prior to incision
- Mannitol (0.5 to 1 mg/kg) for brain relaxation and protection
- Continue prior anticonvulsants: epileptologist may have tapered anticonvulsants in preparation for epilepsy monitoring unit (EMU)
- Several anesthetic agents will alter ECoG, therefore 30 min prior to recording:
- Isoflurane is kept < 0.2%
- Propofol is discontinued
- Isoflurane is kept < 0.2%
- ± N2O (controversial)
- No barbiturates or benzodiazepines
♦ Intraoperative
Positioning
- Foley catheter
- Patient’s ipsilateral shoulder elevated
- Mayfield head holder
- Leave room with draping for wires to exit through skin
- Alternatively, head may be placed on doughnut
- Leave room with draping for wires to exit through skin
- Head turned 90 degrees to opposite side, parallel to floor (assess neck flexibility before surgery)
- Neck is slightly extended, vertex down
- Pressure points are padded
Planning of Shave and Incision
- “Trauma flap”–“question mark” for left and “reverse question mark” for right (or possible L-shape starting in mastoid region)
- Typically full head shave or “box braids” for long hair (and wide shave at incision)
- Incision started at zygoma, 1 cm in front of tragus
- Curved posteriorly, hugging superior aspect of pinna (closer to floor of middle fossa)
- Posterior margin is extended back to parietal boss
- Medial margin is kept 1 cm off midline (to midline, if interhemispheric placement)
- Anterior extent of incision is brought to limit of hairline at widow’s peak
- Typically full head shave or “box braids” for long hair (and wide shave at incision)
- See Chapter 2, General Craniotomy Techniques
Elevate Scalp and Muscle Flap
- Only scalp is incised
- Major bleeders are controlled with bipolar cautery
- Raney clips are applied
- Major bleeders are controlled with bipolar cautery
- Superficial temporal artery is preserved to promote healing
- Temporalis muscle is elevated with monopolar cautery
- Incision is undercut to palpate zygoma
- Sphenoid depression is visualized
- Anterior exposure is maximized
- Incision is undercut to palpate zygoma
- Flap roll is placed behind flap, which is retracted inferiorly
- Wet sponge is placed over muscle
- Two towel clips are placed at base of muscle and held with rubber bands to Leyla bar
- Remaining muscle is everted over ear with suture to maximize inferior exposure
Bone Flap
- Small drill burr is used to make a bony opening under muscle at inferior margin of bone flap (root of zygoma region)
- B1 foot plate is used to free dura from overlying bone
- Craniotomy is turned, extending as far anterior, posterior, and inferior as possible: medial extent is kept 1.5 cm off midline to avoid superior sagittal sinus and arachnoid granulations (or possibly across midline, if interhemispheric placement planned)
- Bone flap is elevated with flap elevator and Penfield no. 3
- Holes are drilled along superior temporal line to reapproximate temporalis muscle
- Drill is used to shave down sphenoid bone
- Temporal lobe exposure is maximized by removal of temporal-bone squamosa with Kerrison or Leksell rongeurs; air cells are good landmark to indicate adequate inferior exposure (image guidance also useful)
- Bone wax is applied to bone edges, particularly if air cells are visible
- Dural tack-up suture holes (optional) are drilled at bony margins and within bone flap
- Screws and microplates are placed in the bone flap and then handed off to scrub nurse to store in antibiotic solution
- FloSeal and strips of Surgicel are placed under bone edges
- 4–0 silk tenting sutures are placed (optional)
Dural Opening
- Horseshoe-shaped with base over sphenoid
- A 1-cm margin is left to facilitate closure and for electrodes to exit
- Cauterization of dura is avoided
- Quarter-inch Cottonoids are placed around edges to wick blood
- Dura is retracted with sutures
- An area as wide as needed (consulting with epileptologist) is covered
- Grid is fashioned by removing electrodes with scissors
- Grid is placed so as to avoid grid buckling; wires pierce edge of dura; “relaxing” cuts between electrode rows may be helpful
- Strips are inserted under bone flap as needed; brain is depressed with Penfield no. 3 to avoid tearing bridging veins
- Blood under grid can interfere with contact
- Contacts are kept off large blood vessels (if possible)
Electrocorticography
- A 5- to 10-min recording is obtained to ensure adequate coverage (optional; may decide on anatomic coverage preoperatively)
- Significant interictal activity at edge of grid may indicate inadequate coverage
- Grid location is documented with intraoperative photograph and schematic drawings
Closure
- Dura
- A 14-gauge Tuohy needle is used to pull wires through dura (or exit via dural incision)
< div class='tao-gold-member'>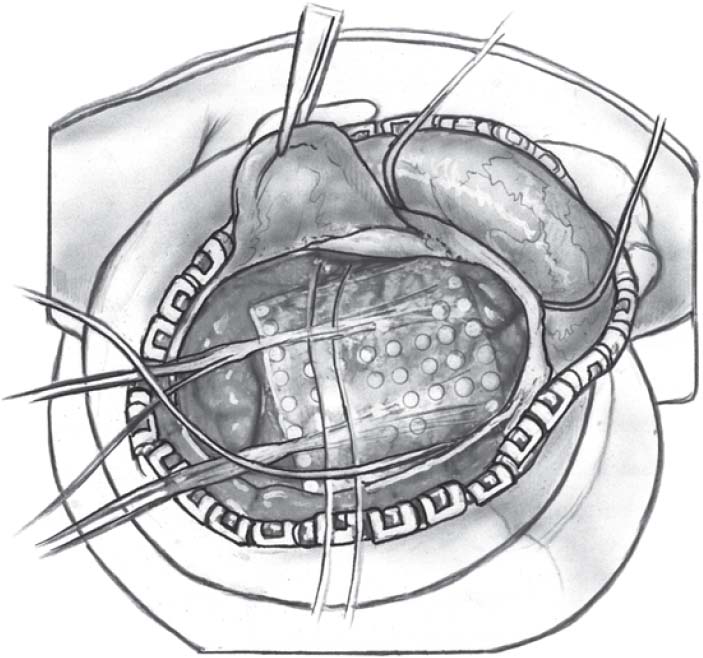 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
- A 14-gauge Tuohy needle is used to pull wires through dura (or exit via dural incision)







