Substance Abuse
Terry Rustin
Addictive drugs are defined by their capacity to reinforce drug-taking behavior, resulting in compulsive use despite negative consequences. The class is defined not by the drugs’ legal status or by their capacity to give pleasure to some individuals, but by these reinforcing properties (1). Some legal drugs kill more people than illegal ones (tobacco vs. heroin), some drugs are legal in some settings and illegal in others (cocaine, anabolic steroids), and some drugs are legal in one city and illegal in another city 20 miles away (marijuana, alcohol).
The syndrome of drug dependence comprises compulsive use despite consequences, along with inability to control drug use after starting, obsession with obtaining and using drugs, denial of the severity of the problem, and neuroadaptation to the drug (2). By the time addicted individuals present for help, they are no longer enjoying their alcohol or drug use—they are trying to stay as normal as possible.
In addition to reinforcement, addictive drugs alter cognition, mood, concentration, alertness, perception, and behavior; other chemicals that alter these central nervous system (CNS) functions (antidepressants, antipsychotics, antiretrovirals, corticosteroids, etc.) do not have reinforcing or neuroadaptive properties. Research has focused on the effects of addictive drugs on neurotransmitters, especially dopamine, but why they are so reinforcing in some individuals and not others is far from clear.
Addictive drug use is more common among individuals with psychiatric disorders than in the general population. Recent studies report that individuals with bipolar disorder have rates of comorbid addiction approaching 60% percent (3), and those with schizophrenia have rates as high as 34% (4). Thus, the staff of every psychiatric emergency service (PES) should expect many times every day to encounter patients who use addictive chemicals (5). They must deal with at least four situations:
Patients presenting to the PES because of a primary problem with alcohol or other drug use; they are intoxicated, in withdrawal, or seeking help for their addiction.
Patients presenting to the PES with a primary psychiatric problem, which is complicated by their use of alcohol or other drugs.
Patients brought to the PES acutely disorganized, psychotic, or violent, with no clear diagnosis, in whom drug use is suspected.
Staff and professional issues, including transference and countertransference issues, regulatory and reporting requirements and limitations, and the use of addictive substances by staff members.
This chapter seeks to clarify and guide the PES professional staff in the diagnosis and management of these issues.
Author disclosure: The author has received honoraria from Reckitt Benckiser, manufacturer of Suboxone (buprenorphine).
PRESENTING CLINICAL FEATURES
PES staff does not have the time for an in-depth interview with each patient, and PES patients are not always cooperative. Therefore, decisions must frequently be made with incomplete data. This is often the case in the initial assessment of patients with drug use disorders.
The first few seconds of the interview reveal whether a patient has an intact level of consciousness, appears sedated or stimulated, or has some other alteration in mentation. This section describes the most important presenting situations of PES patients caused by alcohol and other addictive drugs: excessive sedation, excessive
stimulation, impairment of cognition, suicidal ideation and intent, complaints of acute or chronic pain, and specific physical manifestations of addiction.
stimulation, impairment of cognition, suicidal ideation and intent, complaints of acute or chronic pain, and specific physical manifestations of addiction.
Depressed Level of Consciousness
Alcohol Intoxication
At low blood levels, alcohol is primarily disinhibiting, not sedating, and is perceived by users as a stimulant because they feel less concern or worry and start to have a good time. Some individuals become aggressive, others depressed, others amorous, others foolish. They feel more relaxed because alcohol sedates inhibitions. As the blood alcohol concentration (BAC) increases, they become progressively sedated, culminating in respiratory depression and death.
Sedative Intoxication Other Than Alcohol
At low blood levels, intoxication by sedatives other than alcohol is perceived by the user as a relaxed, anxiety-free state; observers notice progressive disinhibition and sedation. As blood levels increase (either due to delayed absorption of the drug or repeated doses), alertness is progressively decreased to a point at which users cannot be easily aroused; they will eventually lapse into coma and cease breathing spontaneously. Death ensues.
Opioid Intoxication
Patients intoxicated on opioids are sedated; in addition, they have analgesia to all forms of pain—physical, emotional, or mental—and feel a blissful quietude in which they have no worries at all. This dreamy state between lethargy and light sleep in which users are just barely aware of their surroundings is called nodding; it is different from the sedation of the benzodiazepines, which is more of a generalized slowing of mentation and cognition.
Marijuana Intoxication
Initially, marijuana produces disinhibition, but it is rarely accompanied by aggressive behavior; users are more likely to be silly and find humor in ordinary things. The sedation of marijuana is accompanied by a perception of slowing of time and a contraction or elongation of space. Intoxication is not life threatening, but simultaneous use of marijuana and other sedatives produces additive effects.
Volatile Inhalant Intoxication
The sedation produced by volatile inhalants is more like that of anesthetic agents, and may be accompanied by hallucinations, delusions, paranoid fears, or out-of-body experiences. There is a narrow therapeutic window with these drugs; users inhale them (called “huffing”) and progress quickly from alertness through bizarre thoughts to sleep. When they awaken, paper bag in hand, they dose themselves again. Users continue this up-and-down cycle from sedation to lethargy for hours at a time.
Heightened Level of Consciousness
Amphetamine Intoxication
Amphetamine, methamphetamine, methylenedioxymethamphetamine (MDMA, called Ecstasy), methylenedioxy-N-ethamphetamine (MDEA, called Eve), and other derivatives increase alertness and arousal, raise the heart rate and blood pressure, and increase the basal metabolic rate. Individuals become hypervigilant, seeing potential danger where there is none. Because these drugs have a long half-life, this state of hyperarousal can last many hours, deteriorating into paranoid delusions. Intoxication on psychostimulants results in an increase in heart rate, blood pressure, alertness, motor activity, restlessness, and rate of speech. These patients are in less danger from the drug they have taken than they are from the other patients in the PES—because of their intrusiveness and agitation, they tend to pester other patients and not take no for an answer. They may initiate sexual liaisons and make drug deals. Moderate stimulant intoxication tends to make patients feel self-assured and talkative; at higher levels of stimulant intoxication, they become increasingly hypervigilant, easily startled, fearful, and impatient. They are usually in the PES because of complications with a co-occurring psychiatric disorder (schizophrenia or bipolar disorder) and rarely for help with their addiction.
Cocaine Intoxication
Cocaine crosses the blood–brain barrier quickly and efficiently, leading to an immediate elevation of mood, alertness, and vital signs. Cocaine has a short half-life, so even though the hypervigilance of cocaine is indistinguishable from that of amphetamine, it resolves much more quickly.
Phencyclidine Intoxication
Phencyclidine (PCP, called angel dust, fry, whack, and other names) is a special case. It is an analgesic as well as a CNS stimulant; coupled with its marked disinhibiting effects and the delusions of special powers users have, PCP intoxica-tion presents a particularly dangerous situation. Individuals are hypervigilant, agitated, and extremely irritable.
Impaired Mood Control, Cognitive Functioning, Memory, Concentration, and Orientation
Intoxication by any substance, by definition, impairs mental functioning. Some specific impairments due to chronic toxicity also merit a mention here.
Alcohol toxicity. Many years of alcohol use may lead to thiamine deficiency and subsequent Wernicke encephalopathy. Wernicke encephalopathy consists of a triad of eye movement disorders (abducens nerve palsy), ataxia, and depression of consciousness. The eye movement abnormalities usually improve with parenteral thiamine, and the diagnosis may therefore be missed. If the thiamine deficiency is severe and chronic, Korsakoff psychosis may supervene. It consists of the triad of ataxia, memory deficit, and confabulation, an unusual form of disordered memory in which patients replace their memory loss with invented stories. This is done at an unconscious level, and the patients believe they are telling the truth.
Inhalant and hallucinogen toxicity. These drugs impair concentration, memory registration, and cognitive functioning. The deficits are cumulative, and result in permanent impairment in long-term users.
Anabolic steroid toxicity. Natural, semisynthetic, and synthetic steroid intoxication includes aggressiveness, emotional lability, irritability, and explosiveness. These drugs are used by athletes (and by ordinary people) hoping to improve their athletic performance; use of anabolic steroids results in muscle hypertrophy, improved oxygen-carrying capacity, and temporary improvement in feelings of well-being. In most cases, hormonal feedback loops shut down the body’s production of gonadotropin-releasing factor, luteinizing hormone, and follicle-stimulating hormone, which reduces a man’s intrinsic production of testosterone and sperm; testicular atrophy ensues. In women, menses cease, and masculinizing hormones overwhelm feminizing ones. After stopping the steroids, the body does not return to homeostasis for many months, if ever.
Phencyclidine toxicity. Patients intoxicated on PCP are more labile than others, and can shift from being calm and cooperative to being hostile and aggressive in a few seconds.
Withdrawal states. In general, withdrawal states impair concentration more than memory. Testing concentration independent of memory by using an overlearned task, such as repeating the days of the week in reverse, or serial threes, or spelling one’s name in reverse, helps assess the degree of impairment. Patients in withdrawal are more likely to be emotionally labile and irritable.
Life-Threatening Sedation Caused by Drug Overdosage
Intentional overdosage in a suicide attempt using alcohol or other drugs of addiction is quite common but rarely results in death, due to the high degree of neuroadaptation. More serious are overdoses in drug-naive individuals or an overdose with a drug from a class other than the patient’s usual drug—these patients lack tolerance to the drug and are therefore at greater risk. Even more serious are overdoses with drugs of two or more classes; the effects can be synergistic when the drugs activate different receptor systems. Benzodiazepines, for example, activate the gamma-aminobutyric acid (GABA) receptor, whereas opioids activate the mu-opioid receptor. A patient addicted to alprazolam could take an enormous amount of lorazepam and not be in danger from oversedation, but could be after taking 20 hydrocodone tablets.
Overdosage in relapse after a period of abstinence can cause life-threatening oversedation. This is common when patients previously addicted to heroin are released from prison and start back on heroin at about the same dosage they used prior to going into prison; they go into respiratory arrest and die. This appears to be due to downregulation
of their opioid receptors. The receptor is a strand of protein and will degrade over time; lacking the stimulus of regular opioid use, the cell ceases to produce an excess of mu-receptor protein. The same is true for benzodiazepines.
of their opioid receptors. The receptor is a strand of protein and will degrade over time; lacking the stimulus of regular opioid use, the cell ceases to produce an excess of mu-receptor protein. The same is true for benzodiazepines.
Altered Level of Consciousness Associated with but Not Caused by Alcohol and Drug Use
Altered level of consciousness (LOC) also results from head trauma, which is common in patients who are addicted: They fall and strike their heads, and they are frequently at risk of being assaulted. A lethargic patient smelling of alcohol may be triaged to the PES when the real problem is head trauma. Head trauma patients may initially be agitated and aggressive, and may look as if they are intoxicated on amphetamines or PCP. A careful neurologic examination must be part of the PES assessment in every patient with altered LOC, even if alcohol or other drug use seems to be the primary diagnosis. Alcohol intoxication should be commensurate with the BAC. Intoxication on sedatives is generally accompanied by disinhibition and, in serious cases, will usually respond to flumazenil; opioid intoxication will respond to naloxone.
Ingestion of a toxic substance during a suicide attempt can also produce alterations in the LOC. Because alcohol is part of most suicide attempts, the PES psychiatrist may be tempted to ascribe the sedation or confusion to alcohol, when actually it is caused by a chemical other than alcohol, such as acetaminophen, a neuroleptic, diphenhydramine, or an antidepressant. A BAC too low to explain the level of sedation is helpful in making this diagnosis, but a collateral history is even more helpful.
On occasion, alcohol-dependent individuals may consume industrial products to become intoxicated when alcohol is unavailable. These are not suicide attempts, so suicide precautions and psychiatric hospitalization are not needed; nor are they accidental ingestions, which are unlikely to be repeated. These patients know what they doing, and are repeatedly willing to risk the consequences in order to achieve intoxication. The most commonly used substances are methyl alcohol (wood alcohol), isopropyl alcohol (rubbing alcohol), or ethylene glycol (antifreeze). Methyl alcohol (methanol) is metabolized to formaldehyde and then to formic acid, causing a metabolic acidosis, often blindness, and sometimes death. Isopropyl alcohol ingestion causes confusion and delirium and may cause cardiovascular collapse. Ethylene glycol causes a metabolic acidosis, renal failure, and often death. An unusual odor on the patient’s breath, a BAC too low to explain the degree of sedation, or an unexplained metabolic acidosis help make the diagnosis and redirect treatment.
Portal systemic encephalopathy (PSE), or hepatic coma, results from years of progressive deterioration of the liver, most often as a result of alcohol use or chronic hepatitis, or both. These patients become agitated, confused, and disoriented, and may appear as if intoxicated on alcohol. Giving such a patient a sedating drug will cause further mental impairment; in addition, if the medication given requires hepatic metabolism, it will be there a very long time, because the patient’s confusion is due to impaired liver function. If PSE is suspected (and it should be in any alcohol-dependent patient with jaundice), lab tests (liver function tests, serum bilirubin, serum ammonia) should be done before administering sedatives. In this situation, medications with short half-lives that do not require hepatic metabolism (e.g., oxazepam or lorazepam) are preferred.
Drinking alcohol after taking disulfiram (Antabuse) results in an acute delirium that may resemble PSE or alcohol intoxication. Disulfiram partially antagonizes aldehyde dehydrogenase and therefore impedes the conversion of acetaldehyde to acetate. Any use of alcohol in a patient on disulfiram results in an excess of acetaldehyde. Initially, the patient is agitated and confused, with elevated vital signs, and resembles a patient in early portal systemic encephalopathy. With further alcohol use or further buildup of acetaldehyde, the patient becomes lethargic and then stuporous, with a waning pulse and blood pressure, and may die. These patients may resemble a person intoxicated on alcohol alone. The key to diagnosis is twofold: a level of intoxication much greater than the BAC would justify, and the odor of acetaldehyde (like other aldehydes, it has a somewhat fruity, musky odor).
Chronic Pain
Patients in acute pain will be seen first in the medical-surgical ED, whereas patients with chronic pain may be triaged to the PES, especially if they are only requesting a prescription for
medication. Most of these patients have a physical cause for their pain; all are addicted to opioids, and all they want from the PES is a prescription. Hydrocodone is the most common drug requested; these patients are typically using thirty to fifty 10-mg hydrocodone/acetaminophen tablets daily. Less frequently, they are using extended-release oxycodone, methadone, or fentanyl patches. These drugs are often taken concomitantly with carisoprodol (Soma, which is metabolized to meprobamate) and alprazolam (Xanax). Such patients usually obtain their drugs from “script docs” who provide prescriptions for hundreds of tablets following a cursory evaluation, from dealers on the street, from cancer patients who do not need all the medication they are prescribed, and from the Internet. When their supply runs out, they show up in emergency centers.
medication. Most of these patients have a physical cause for their pain; all are addicted to opioids, and all they want from the PES is a prescription. Hydrocodone is the most common drug requested; these patients are typically using thirty to fifty 10-mg hydrocodone/acetaminophen tablets daily. Less frequently, they are using extended-release oxycodone, methadone, or fentanyl patches. These drugs are often taken concomitantly with carisoprodol (Soma, which is metabolized to meprobamate) and alprazolam (Xanax). Such patients usually obtain their drugs from “script docs” who provide prescriptions for hundreds of tablets following a cursory evaluation, from dealers on the street, from cancer patients who do not need all the medication they are prescribed, and from the Internet. When their supply runs out, they show up in emergency centers.
PES staff must be alert in these situations so as not to be naive accomplices in illegal drug use, and to intervene whenever possible. Patients with a legitimate need for opioid analgesics should be given no more than 1 day’s supply of a schedule III (not a schedule II) medication from the PES, with a referral to a reliable physician. If the PES prescribes a substantial amount of opioids or schedule II opioids, word will get around quickly, and the PES will become a chronic pain clinic.
IMMEDIATE INTERVENTIONS FOR ACUTE PRESENTATIONS
Before the Patient Sees the Psychiatrist
The PES is a unique environment, where highly trained professionals provide compassionate care to patients who often refuse it. Patients are often hostile and may become violent toward staff, other patients, and themselves. The safety of PES staff and their patients must be ensured for good treatment to proceed. A metal scanner and visual inspection by a security officer is a minimum level of search for any PES, with all bags and containers and food left at the door. Of course, a metal scanner will not detect drugs or alcohol, and patients or visitors intent on bringing drugs into the PES will be able to do so by hiding them on their persons. The PES has the right to inspect patients and visitors in order to maintain a safe and therapeutic environment.
Urine Drug Testing
Psychiatrists get little help in making a DSM-IV diagnosis from laboratory testing; this is also true for diagnosing addiction. A positive drug screen reveals some of the drugs a patient has recently used, but it provides little information about the cause of a patient’s behavior or impairment, for multiple reasons.
Many drugs do not show up reliably on a routine drug screen—notably phencyclidine. The patient may be intoxicated on phencyclidine, yet have a negative drug screen for it. Neither methadone nor buprenorphine reacts positively on a routine test for opioids. Alcohol may be present in the urine and react positively on a drug screen, but exist in such low concentrations that it is not affecting the patient’s mental state. Many common medications cause a false-positive drug screen (ibuprofen, bronchodilators), and some interfere with testing, causing a false-negative drug screen (usually intended by the user). Most false negatives are due to urine dilution (copious water drinking several hours before the test) and the passage of time since the last use (especially for drugs with a short half-life).
The patient may be in withdrawal from one drug and intoxicated on a second one, but the drug screen does not distinguish between them (e.g., if the patient is in withdrawal from benzodiazepines and intoxicated on cocaine, the drug screen will be positive for both, but it does not reveal which condition requires immediate intervention). The patient’s signs and symptoms may be from drug toxicity or from an idiosyncratic reaction to a drug rather than drug intoxication.
Drug screens test for cocaine metabolites (benzoylecgonine and ecgonine methyl ester), not cocaine itself, and thus the drug screen does not reveal whether the patient is under the influence of cocaine at the time of evaluation (e.g., a bipolar patient who used cocaine 3 days ago, precipitat-ing a manic episode). With the exception of oxazepam and lorazepam, benzodiazepines have multiple metabolic products that test positive on drug screens; chlordiazepoxide has at least four metabolic products. Thus, a positive drug screen for benzodiazepines does not reveal how recently the patient used these drugs, which drug was used, or whether or not they are responsible for the clinical presentation.
If the patient’s past psychiatric and medical histories are not known, the patient’s presentation may be incorrectly ascribed to the drug showing up on the drug screen, when the patient is actually at baseline (e.g., alcohol intoxication in a patient with dementia). The patient may have used drugs that show up in a drug screen, but the presenting problem may be caused by a medical condition (e.g., positive drug screen for marijuana in a patient with encephalitis) or a psychiatric condition (e.g., positive drug screen for cocaine metabolites in a patient with paranoid schizophrenia) and not the drug.
For all these reasons, urine drug testing has limited usefulness in the PES.
Intoxication and Withdrawal
Table 22.1 shows drug intoxication and withdrawal states requiring immediate intervention.
TABLE 22.1 Drug Intoxication and Withdrawal States Requiring Immediate Intervention | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Intoxication is defined as a measurable change in an individual’s cognition, mood, behavior, perception, or neurologic function as a result of use of a drug. Intoxication is the state individuals seek when using any drug. Addicted individuals have lost the ability to control their level of intoxication. Intoxicated individuals rarely present for treatment at the PES; when they do come, it is usually in the company of law enforcement or because of dysphoria from excessive intoxication, a medical or psychiatric complication, or a suicide attempt. Withdrawal is the set of signs and symptoms that appear in an addicted individual when the blood level of the drug decreases; these findings are drug specific. Detoxification is the process by which the withdrawal from intoxication is medically managed to minimize complications and discomfort.
In clinical settings, detoxification should be seen as the prelude to psychosocial treatment
resulting in abstinence and recovery. Although the majority of patients resume chemical use after completing detoxification, clinicians should not abandon efforts to motivate patients toward recovery. Addiction is a chronic, relapsing psychiatric illness, like bipolar disorder; clinicians do not refuse to treat bipolar patients for a second or third or thirtieth manic episode, and they should not refuse to treat addiction patients for a second or third or thirtieth relapse either.
resulting in abstinence and recovery. Although the majority of patients resume chemical use after completing detoxification, clinicians should not abandon efforts to motivate patients toward recovery. Addiction is a chronic, relapsing psychiatric illness, like bipolar disorder; clinicians do not refuse to treat bipolar patients for a second or third or thirtieth manic episode, and they should not refuse to treat addiction patients for a second or third or thirtieth relapse either.
We can divide addictive drugs into the following six categories, based on their CNS effects:
Alcohol
Sedatives other than alcohol
Cocaine and amphetamines
Hallucinogens
Dissociative drugs
Opioids
For each group, both intoxication and withdrawal present special treatment issues. Of these, alcohol withdrawal, sedative withdrawal, and dissociative drug intoxication are the most critical.
Alcohol Intoxication
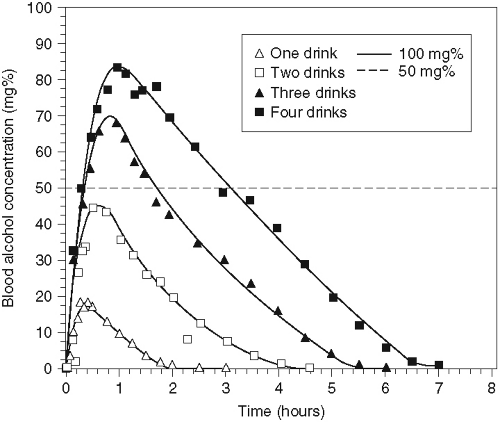
Alcohol intoxication so severe as to threaten the life of the patient is not common, because as individuals become increasingly intoxicated, they usually fall asleep long before respiratory depression occurs (Table 22.2). However, if the individual drinks a great deal very rapidly, the alcohol is temporarily sequestered in the stomach and is not absorbed; 10 or 15 minutes later, it will be, and the individual can lapse into coma (see Fig. 22.1 for BACs attained after one to four drinks). Around
three hundred people die each year from alcohol intoxication (“accidental alcohol poisoning”) in the United States, and alcohol is a contributing factor in about 1,000 additional accidental deaths (6). Contrary to common belief, most of these individuals are not young adults, but men in their 40s and 50s. Situations in which this occurs include the following: drinking heavily to alleviate dysphoric feelings, wagers on one’s drinking capacity, fraternity parties, hazings, initiations, party games, and 21st-birthday celebrations. In the PES, collateral history will help make the diagnosis.
three hundred people die each year from alcohol intoxication (“accidental alcohol poisoning”) in the United States, and alcohol is a contributing factor in about 1,000 additional accidental deaths (6). Contrary to common belief, most of these individuals are not young adults, but men in their 40s and 50s. Situations in which this occurs include the following: drinking heavily to alleviate dysphoric feelings, wagers on one’s drinking capacity, fraternity parties, hazings, initiations, party games, and 21st-birthday celebrations. In the PES, collateral history will help make the diagnosis.
TABLE 22.2 Progression of Sedating Effects of Alcohol | |||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||
A rising BAC over 20 minutes in an already intoxicated patient signals danger; this patient should be transferred to the medical-surgical ED and should not be given any sedative medication, even if combative. Gastric lavage and charcoal are of no value in these cases; the alcohol will be completely absorbed by the time the patient arrives in the PES. Intravenous fructose increases alcohol metabolism, but not sufficiently to reverse respiratory depression. Flumazenil may help, but the best treatment is to admit these patients to the medical intensive care unit (ICU) and support their respirations until their livers metabolize the alcohol. In the case of a patient with hepatic insufficiency, peritoneal dialysis will quickly remove most of the alcohol.
Alcohol is metabolized in the liver (and to a smaller extent in other organs) via zero-order kinetics (a constant amount, not a constant percentage, is metabolized per unit of time). In a healthy individual with moderate alcohol experience, metabolism drops the BAC by about 20 to 25 mg/dL each hour; thus, a man drinking five standard drinks over 2 hours will return to a BAC of 0 in about 4 more hours. However, a person with impaired hepatic function will metabolize the alcohol more slowly (as a result of having fewer functioning hepatocytes), and an alcohol-dependent person with an intact liver will metabolize the alcohol more rapidly (as a result of hypertrophy of the microsomal ethanol oxidizing system). Women tend to lack alcohol dehydrogenase in the lining of the stomach; a woman therefore achieves a higher BAC than a man of the same size after consuming the same number of drinks (7).
Patients with portal systemic encephalopathy do not have to drink very much to become agitated or delirious; they can progress quickly to
coma and death. An agitated patient with PSE may look like a patient in alcohol withdrawal; if the diagnosis of PSE is not made and the patient is given a neuroleptic or a large dose of a sedative, the PSE will quickly worsen. Thus, if PSE is suspected in a patient intoxicated on alcohol, very small doses of medication must be used, with a preference for those with a short half-life and less hepatic conversion.
coma and death. An agitated patient with PSE may look like a patient in alcohol withdrawal; if the diagnosis of PSE is not made and the patient is given a neuroleptic or a large dose of a sedative, the PSE will quickly worsen. Thus, if PSE is suspected in a patient intoxicated on alcohol, very small doses of medication must be used, with a preference for those with a short half-life and less hepatic conversion.