Substance-Related Disorders
Substance disorders are complex psychiatric conditions that govern both internally perceived mental states, such as mood, and externally observable activities, such as behavior. As with most other psychiatric disorders, both biological factors and environmental circumstance govern a person’s involvement in the disorder. Substances can cause neuropsychiatric symptoms indistinguishable from those of common psychiatric disorders with no known causes (e.g., schizophrenia and mood disorders), and thus primary psychiatric disorders and disorders involving the use of substances are possibly related. It is important to understand and appreciate the common features found in these disorders and how they differ from other psychiatric illnesses in order to provide adequate care and treatment for patients with these conditions.
Diagnosing a psychiatric disorder in the context of substance abuse can be complicated. A careful and detailed chronological history of symptom development and its relationship to substance use is critical to clarifying diagnoses. Although a primary diagnosis may be unclear at times, what does seem clear is that substance abuse worsens the course, prognosis, and presentation of any preexisting psychiatric disorder. A patient with schizophrenia who abuses crack cocaine or a depressed patient abusing cocaine or benzodiazepines will undoubtedly be more impaired than a patient who is not. In fact, most experienced clinicians will agree that effectively treating any psychiatric disorder in the context of ongoing substance abuse is not possible.
Clinicians need to be clear about the definitions of many terms relating to substance use, including addiction, dependence, abuse, tolerance, cross-tolerance, intoxication, and withdrawal. Each substance-related disorder also has its own definition, epidemiology, and clinical features, and skilled clinicians must be knowledgeable about each one.
Students should study the questions and answers below for a useful review of these disorders.
Helpful Hints
Students should know each of the terms below.
AA
abuse
addiction
Al-Anon
alcohol delirium
alcohol psychotic disorder
alcohol withdrawal
amotivational syndrome
anabolic steroids
arylcyclohexylamines
belladonna alkaloids
binge drinking
blackouts
caffeine
cocaine delirium
cocaine-induced psychotic disorder
cocaine intoxication and withdrawal
codependence
cross-tolerance
DEA
dispositional tolerance
disulfiram
DSM-IV-TR course modifiers
DTS
dual diagnosis
fetal alcohol syndrome
flashback
freebase
hallucinogen
hallucinogen persisting perception disorder
idiosyncratic alcohol intoxication
illicit drug use
inhalant intoxication
ketamine
Korsakoff’s and Wernicke’s syndromes
LAMM
LSD
MDMA
methadone withdrawal
misuse
MPTP-induced parkinsonism
nicotine receptor
NIDA
nitrous oxide
opiate
opioid antagonists
opioid intoxication and withdrawal
PCP
persisting amnestic disorder
persisting dementia
physical dependence
psychedelics
psychoactive
psychological dependence
RFLP
“roid” rage
sedative-hypnotic anxiolytic
STP alcohol intoxication; blood levels
substance dependence and abuse
THC
tolerance
type I and II alcoholism
volatile hydrocarbons
withdrawal
Questions
Directions
Each of the questions or incomplete statements below is followed by five suggested responses or completions. Select the one that is best in each case.
12.1. The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) states specifically that the diagnosis of dependence can be applied to every class of substances except
A. anabolic steroids
B. caffeine
C. nicotine
D. nitrous oxide
E. none of the above
View Answer
12.1. The answer is B
The DSM-IV-TR section dealing with substance dependence and substance abuse presents descriptions of the clinical phenomena associated with the use of 11 designated classes of pharmacological agents: alcohol; amphetamines or similarly acting agents; caffeine; cannabis; cocaine; hallucinogens; inhalants; nicotine; opioids; PCP or similar agents; and sedatives, hypnotics, and anxiolytics. A residual twelfth category includes a variety of agents, such as anabolic steroids and nitrous oxide, that are not in the 11 designated classes.
In addition to requiring the clustering of three criteria in a 12-month period, the DSM-IV-TR includes a few other qualifications. It states specifically that the diagnosis of dependence can be applied to every class of substances except caffeine. That point is admittedly controversial, and some researchers believe, on the basis of the same DSM-IV-TR generic criteria, that caffeine produces a distinct form of dependence, although it is relatively benign for most persons.
12.2. FT is a 73-year old successful emeritus professor at a small liberal arts college in the Midwest. He was in relative good health when he entered the hospital for an elective hernia repair. The brief history contained no detailed notes of his drinking pattern and made no mention of his γ-glutamyltransferase value of 55 U/L along with the mean corpuscular volume (MCV) of 93.5 μ m3. Eight hours postsurgery, the nursing staff noted an acute increase in the pulse rate to 110 beats/min, an increased in blood pressure to 150/100 mm Hg, prominent diaphoresis, and a tremor to both hands, after which the patient demonstrated a brief but intense grand mal convulsion. He awoke agitated and disoriented to time, place, and person. A reevaluation of the history and an interview with the patient’s wife documented his alcohol dependence with a consumption of approximately six standard drinks per night. Over the following 4 days, the patient’s autonomic nervous system dysfunction decreased as his cognitive impairment disappeared. Which condition is the best classification for Mr. FT in the above case?
A. Alcohol withdrawal delirium
B. Wernicke’s encephalopathy
C. Korsakoff’s syndrome
D. Alcohol-induced anxiety disorder
E. Alcohol-induced persisting dementia
View Answer
12.2. The answer is A
FT experienced alcohol withdrawal delirium postsurgery. Alcohol intoxication delirium and alcohol withdrawal delirium occur when intoxication or withdrawal is accompanied by severe cognitive symptoms and occur in fewer than 5 percent of intoxications or withdrawals. When this agitated confusion is associated with tactile or visual hallucinations, the diagnosis of alcohol withdrawal delirium (also called delirium tremens) can be made. During withdrawal, some alcoholic people show one or several grand mal convulsions, sometimes called rum fits.
Wernicke’s encephalopathy and Korsakoff’s syndrome are both subdivisions of alcohol-induced persisting amnestic disorder, which is the result of a relatively severe deficiency of vitamin B1, thiamine. Wernicke’s encephalopathy, also called alcoholic encephalopathy, is an acute neurological disorder characterized by ataxia (affecting primarily the gait), vestibular dysfunction, confusion, and nystagmus. Wernicke’s encephalopathy may clear spontaneously within a few days or weeks or may progress into Korsakoff’s syndrome. Korsakoff’s syndrome is characterized by impaired mental syndrome (especially recent memory) and anterograde amnesia in an alert and responsive patient. The patient may or may not have the symptom of confabulation. The syndrome is permanent in at least partial form in about 50 to 70 percent of affected patients, and 30 percent of patients may recover fully. Patients appear to respond to 50 to 100 mg of oral thiamine a day, usually administered for many months.
Alcohol-induced persisting dementia is characterized by heterogeneous long-term cognitive problems that develop in the course of alcoholism. Global decreases in intellectual functioning, cognitive abilities, and memory are observed. Brain functioning tends to improve with abstinence, but perhaps half of all affected patients have long-term and even permanent disabilities in memory and thinking.
Anxiety symptoms fulfilling the diagnostic criteria for alcohol-induced anxiety disorder are also common in the context of acute and protracted alcohol withdrawal. Almost 80 percent of alcoholic people report panic attacks during at least one acute withdrawal episode. Similarly, during the first 4 weeks or so of abstinence, people with severe alcohol problems have symptoms resembling social phobia.
12.3. Which of the following statements regarding cancer and alcohol use is correct?
A. Cancer may be caused by the immunosuppressive effects of ethanol.
B. Cancer is the second leading cause of premature death in alcoholics.
C. Increases in breast cancer have been noted with just two drinks per day.
D. Alcohol can be directly linked to cancers of mucous membranes.
E. All of the above
View Answer
12.3. The answer is E (all)
High rates of most cancers are seen in alcoholic people, especially cancers of the head, neck, esophagus, stomach, liver, colon, lungs, and breast tissue. An enhanced risk for breast malignancies might be seen with as few as two drinks per day, especially in women with family histories of this disease. The association with cancer probably reflects alcohol-related immune system suppression and the direct effects of ethanol on mucous membranes. The heightened rates of malignant tumors in alcoholic people remain significant even when the possible effects of smoking and poor nutrition are considered, and this is the second leading cause of premature death in alcohol-dependent men and women.
12.4. Which of the following statements regarding alcohol’s effect on sleep is false?
A. Heavy drinkers often awaken at night and have difficulty going back to sleep.
B. Alcoholics tend to have more dreams later in the night.
C. Alcohol increases rapid eye movement (REM) sleep.
D. Alcohol can significantly impair normal sleep patterns.
E. Alcohol use tends to inhibit stage 4 sleep.
View Answer
12.4. The answer is C
Alcohol intoxication can help a person fall asleep more quickly, but if the intake in an evening is more than one or two drinks, the sleep pattern can be significantly impaired. Most heavy drinkers awaken after several hours and can have problems falling back asleep. Alcohol also tends to depress rapid eye movements (REMs) and inhibit stage 4 sleep and thus is likely to be associated with frequent alternations between sleep stages (sleep fragmentation) and with more dreams late in the night as the blood alcohol level decreases. Exaggerated forms of similar problems are seen in alcoholics in whom sleep stages might not return to normal for 3 or more months after abstinence.
12.5. Acute PCP intoxication is not treated with
A. diazepam (Valium)
B. cranberry juice
C. phentolamine (Regitine)
D. phenothiazines
E. all of the above
View Answer
12.5. The answer is D
Phenothiazines are not used in the treatment of acute PCP intoxication because they have anticholinergic effects that may potentiate the adverse effects of PCP, such as seizures. Diazepam (Valium) is useful in reducing agitation. If agitation is severe, however, the antipsychotic haloperidol (Haldol) may have to be used. Cranberry juice is used to acidify the urine and to promote the elimination of the drug; ammonium chloride or ascorbic acid serves the same purpose. Phentolamine (Regitine) is a hypotensive agent that may be needed to deal with severe hypertensive crises produced by PCP.
12.6. In distinguishing schizophrenia from amphetamine-induced toxic psychosis, the presence of which of the following is most helpful?
A. tactile or visual hallucinations
B. paranoid delusions
C. intact orientation
D. clear consciousness
E. auditory hallucinations
View Answer
12.6. The answer is A
Amphetamine-induced toxic psychosis can be exceedingly difficult to differentiate from schizophrenia and other psychotic disorders characterized by hallucinations or delusions. Paranoid delusions occur in about 80 percent of patients and hallucinations in 60 to 70 percent. Consciousness is clear, and disorientation is uncommon. The presence of vivid visual or tactile hallucinations should raise suspicion of a drug-induced disorder. In areas where and populations in whom amphetamine use is common, it may be necessary to provide only a provisional diagnosis until the patient can be observed and drug test results are obtained. Even then, there may be difficulties because in some urban areas, a high percentage of persons with established diagnoses of schizophrenia also use amphetamines or cocaine. Typically, symptoms of amphetamine psychosis remit within 1 week, but in a small proportion of patients, psychosis may last for more than 1 month.
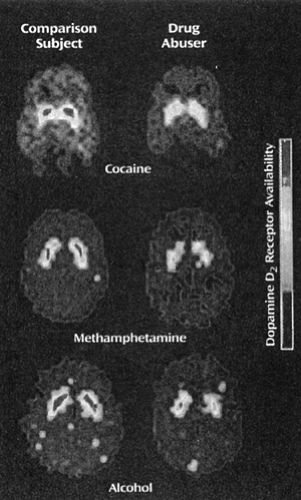
12.7. The image in Figure 12.1 shows decreased dopamine type 2 (D2) receptor binding in the striatum in drug users compared with normal control subjects. Which of the following types of substance withdrawal is this pattern not typical of?
A. Alcohol
B. Cocaine
C. Methamphetamine
D. Opioids
E. All of the above
View Answer
12.7. The answer is D
Opioid withdrawal has not been associated with decreased dopamine binding in the striatum. It has been found repeatedly that there are perfusion deficits in brains of cocaine-dependent subjects recently withdrawn from cocaine. This deficit is probably not related to tolerance or withdrawal, but several other findings probably are. Many (but not all) studies using positron emission tomography and single photon emission computed tomography to examine the brains of cocaine-dependent subjects have found a decreased number of dopamine transporters in the striatum, a finding consistent with postmortem studies. At 1 to 4 weeks and at 3 to 4 months postwithdrawal, cocaine abusers have lower metabolic rates in the frontal cortex that correlate with symptoms of depression and decreased availability of D2 receptors. These findings were similar in studies of patients after alcohol and amphetamine withdrawal.
12.8. Which of the following is not a therapeutic indication for use of anabolic-androgenic steroids?
A. Anemia
B. Hereditary angioedema
C. Hyperthyroidism
D. Male hypogonadism
E. Osteoporosis
View Answer
12.8. The answer is C
Anabolic-androgenic steroids (AAS) have not been used in the treatment of hyperthyroidism. The anabolic steroids are a family of drugs comprising the natural male hormone testosterone and a group of more than 50 synthetic analogs of testosterone, synthesized over the past 60 years. These drugs all exhibit various degrees of anabolic (muscle-building) and androgenic (masculinizing) effects. Thus, they should more correctly be called AAS. Note that it is important not to confuse the AAS (testosterone-like hormones) with corticosteroids (cortisol-like hormones such as hydrocortisone and prednisone). Corticosteroids have no muscle-building properties and hence little abuse potential. AAS, by contrast, have only limited legitimate medical applications. However, AAS are widely used illicitly, especially by boys and young men seeking to gain increased muscle mass and strength either for athletic purposes or simply to improve personal appearance.
AAS are primarily indicated for testosterone deficiency (male hypogonadism), hereditary angioedema (a congenital skin disorder), and some uncommon forms of anemia caused by bone marrow or renal failure. In women, they are given, although not as first-choice agents, for metastatic breast cancer, osteoporosis, endometriosis, and adjunctive treatment of menopausal symptoms. In men, they have also been used experimentally as a male contraceptive and for treating major depressive disorder and sexual disorders in eugonadal men. Recently, they have been used to treat wasting syndromes associated with AIDS. Controlled studies have also suggested that testosterone has antidepressant effects in some HIV-infected men with major depressive disorder, and it is also a supplementary (augmentation) treatment in some depressed men with low endogenous testosterone levels who are refractory to conventional antidepressants.
12.9. Ms. E is a 32-year-old single white woman employed full time at a local factory. She is a smoker and occasionally has flares of asthma. She typically drinks four to five mugs of coffee each day and prefers to drink it without cream, milk, or sugar. Physicians had recommended she cut down or stop her coffee use because of complaints of mild indigestion, and she abruptly stopped her caffeine intake as a result of these recommendations. Which of the following statements regarding caffeine is true?
A. Caffeine is slowly absorbed and metabolized by the kidneys.
B. Caffeine’s effects on the body include bronchoconstriction.
C. Caffeine metabolism is markedly increased at the end of pregnancy.
D. Caffeine increases the metabolism of the antipsychotic clozapine.
E. The rate of caffeine elimination is increased by smoking.
View Answer
12.9. The answer is E
Caffeine is a methylxanthine, as are theobromine (found in chocolate) and theophylline (typically used in the treatment of asthma). Caffeine is well absorbed from the gastrointestinal tract, with peak plasma concentrations typically occurring within 1 hour after ingestion. Caffeine is readily distributed throughout the body and is metabolized by the liver. The half-life of caffeine is approximately 5 hours, with large individual differences. The rate of caffeine elimination is increased by smoking, oral contraceptives, steroids, cimetidine, and fluvoxamine (Luvox). Caffeine inhibits the metabolism of the antipsychotic clozapine (Clozaril) and the bronchodilator theophylline (Theo-Dur) to an extent that might be clinically significant. Caffeine metabolism is markedly slowed at the end of pregnancy.
Caffeine exerts effects throughout the body, including bronchodilation (hence the therapeutic application of caffeine and theophylline in the treatment of asthma); modest increases in blood pressure (which are reduced in caffeine-tolerant individuals); increased production of urine; increases in gastric acid secretion; and increases in plasma epinephrine, norepinephrine, renin, and free fatty acids. Centrally, caffeine affects turnover or levels of various neurotransmitters, and it functions as a central nervous system stimulant.
12.10. The above patient would most likely experience all of the following because of her abruptly stopping caffeine intake except
A. decreased concentration
B. headache
C. insomnia
D. irritability
E. muscle aches
View Answer
12.10. The answer is C
Insomnia is a symptom of caffeine intoxication, not withdrawal. Even though the DSM-IV-TR does not include a diagnosis of caffeine withdrawal, several well-controlled studies indicate that caffeine withdrawal is a real phenomenon. The appearance of withdrawal symptoms reflects the tolerance and physiological dependence that develop with continued caffeine use. Several epidemiological studies have reported symptoms of caffeine withdrawal in 50 to 75 percent of all caffeine users studied. The most common symptoms are headache and fatigue; other symptoms include anxiety, irritability, mild depressive symptoms, impaired psychomotor performance, nausea, vomiting, craving for caffeine, and muscle aches and stiffness. The number and severity of the withdrawal symptoms are correlated with the amount of caffeine ingested and the abruptness of the withdrawal. Caffeine withdrawal symptoms have their onset at 12 to 24 hours after the last dose; the symptoms peak in 24 to 48 hours and resolve within 1 week.
12.11. Which of the following is contraindicated for the treatment of acute disulfiram (Antabuse) overdose?
A. Activated charcoal
B. Decontamination
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree