Chapter 7 Suprascapular Nerve
The Suprascapular Nerve
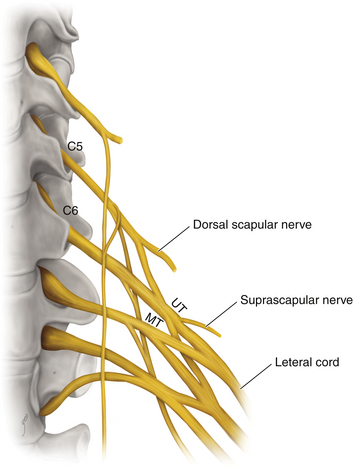
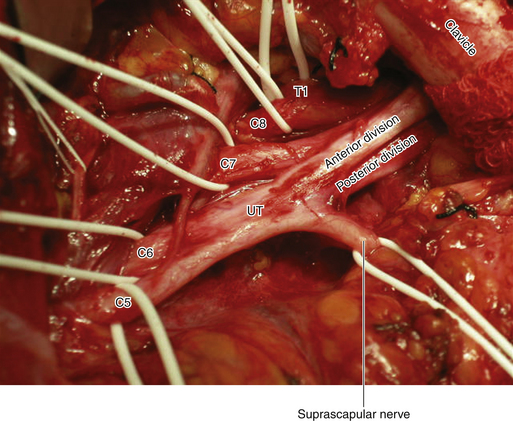
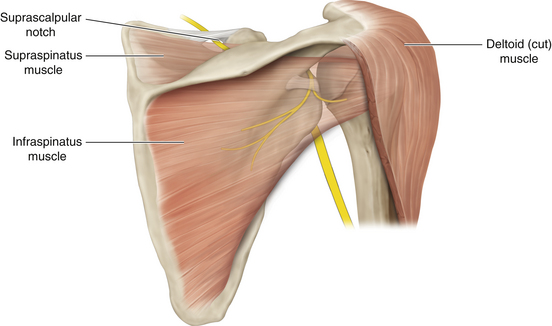
• The suprascapular nerve arises from the upper trunk of the brachial plexus, in close proximity to the anterior and posterior divisions (Figure 7-1). It receives fibers primarily from the C5 and C6 spinal nerves (Figure 7-2). The suprascapular nerve supplies the supraspinatus and infraspinatus muscles and the shoulder joint.
• Both muscles are important to shoulder function, the supraspinatus to initiate abduction and the infraspinatus to initiate external rotation. If elbow flexion is achieved after surgery, the patient will have difficulty in bringing food to the mouth if suprascapular function is not also regained.
• In the posterior triangle of the neck, the suprascapular nerve leaves the brachial plexus close to the lateral border of the scalenus medius.
• The suprascapular nerve passes laterally and downward and across the posterior triangle of the neck. It runs superior to the brachial plexus. The suprascapular nerve passes though the suprascapular notch under the transverse scapular ligament to descend deep to the supraspinatus and infraspinatus muscles (Figure 7-3).
• During an anterior approach, the inferior belly of the omohyoid can be used as a guide to the suprascapular notch, because that is the point of insertion of the inferior belly of the muscle.
Patient Positioning and Skin Incision
• An incision is made parallel to and slightly above the scapular spine. This can be done with the patient either supine or prone (Figures 7-4 and 7-5).
• We favor the supine position and use folded sheets beneath the patient’s shoulder, head, and neck, so that the shoulder area is somewhat elevated off the operating table.
• The incision is deepened to expose the trapezius. This muscle is then split in the direction of its fibers.
• Next, the supraspinatus is split in the direction of its fibers. The muscle can sometimes be mobilized both inferiorly and superiorly away from the spine of the scapula, and then retracted after it has been encircled with a wrung-out, moist 4 x 4 inch sponge.
• It is important to extend the exposure well laterally toward the acromion.
• The suprascapular ligament crossing the notch is then exposed. The nerve runs deep to the ligament (the usual point of entrapment), and the vessels run superficial to the ligament (Figure 7-6). On rare occasions, the artery may accompany the nerve.
• It is important to note a variation of the suprascapular nerve in which the supraspinatus branch passes superior to the ligament. Entrapment under these circumstances might spare supraspinatus function, but can result in dysfunction of the infraspinatus.
• The arterial branch can be retracted by a plastic loop.
• The ligament is then sectioned by a No. 15 scalpel blade on a long-handled knife (Figure 7-7).
• A plastic loop is placed around the suprascapular nerve as it heads toward the scapular notch. If necessary, the nerve can be dissected toward and through the scapular notch.
• If an entrapment involves the distal suprascapular nerve in the region of the scapular notch, this portion of the nerve can be exposed by an incision below the spine of the scapula.
• The infraspinatus is then split in the direction of its fibers, so that the surgeon can dissect down on the branched portion of the nerve on the backside of the scapula.
• The suprascapular nerve operation is much trickier than one would expect. It certainly pays to very carefully examine the scapula on a skeleton before the operation so as to fully appreciate just where the suprascapular notch is.
• The bony shape of the notch varies from patient to patient. Most inexperienced operators attempt to find the nerve too far medially.
• At the crucial part of the operation, the surgeon is operating in quite a deep hole. Illumination and magnification, provided by a microscope, are a great help to both the surgeon and assistant.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree