Chapter 10
Surgery
Chapter objectives
- Present an overview of surgical procedures that are commonly used with clients with neurological conditions.
- Present a narrative review and critique of the research evidence for upper limb surgery.
- Discuss indications and aims for surgery for people with different upper limb characteristics.
- Describe the factors to consider when supporting clients and caregivers through the process of surgical consultation, procedures and follow-up.
Abbreviations
| AROM | Active range of motion |
| C1-8 | Cervical nerves, 1 to 8 |
| HGF | House, Gwathmey & Fidler thumb classification |
| HIPM | Hypertonicity Intervention Planning Model |
| HO | Heterotopic ossification |
| L1-5 | Lumbar nerves, 1 to 5 |
| MACS | Manual Ability Classification Scale |
| MASMS | Modified Ashworth Scale of Muscle Spasticity |
| MCP | Metacarpophalangeal (joint) |
| PROM | Passive range of motion |
| ROM | Range of motion |
| S1-5 | Sacral nerves, 1 to 5 |
| Z&Z | Zancolli & Zancolli hand classification |
10.1 Classification of surgical procedures
Surgery for children and adults with neurological disorders can be classified into three categories: dorsal rhizotomies, peripheral neurotomies and orthopaedic procedures, each of which is indicated in different circumstances. While beyond the focus of this chapter, deep brain stimulation techniques, such as stimulation of the globus pallidus internus, have been used successfully to reduce rigidity and tremor associated with Parkinson’s Disease and in recent years have been applied to people with dystonic cerebral palsy with some promising results, although ongoing research is indicated [1].
Dorsal rhizotomies and peripheral neurotomies are both termed “neuroablative procedures” because they involve interruption of the stretch reflex with the aim of reducing spasticity. In contrast, orthopaedic surgery is concerned with the musculoskeletal system and aims to prevent or correct bony and soft tissue deformity [2].
10.1.1 Neuroablative procedures
Dorsal rhizotomy involves permanent sectioning (cutting or dividing) of the sensory component of the dorsal roots of the spinal cord to promote a generalised reduction in spasticity when it is the main factor impacting on a person’s overall care, comfort or function [2, 3]. Dorsal rhizotomy is more commonly used to address spasticity in the lower limbs, although the technique is also reported to be effective in the upper limbs [4]. Neurotomy (cutting of a peripheral nerve) is indicated when spasticity is localised to a group of muscles supplied by one or several peripheral nerves [5]. For example, division of some fascicles (bundles) of the median and ulnar nerves might be used to reduce spasticity in the wrist and finger flexors [5]. However, it is important that such procedures are selective to ensure that sensory functions and muscle strength are preserved and that spasticity does not recur [2, 5, 6].
10.1.2 Orthopaedic procedures
Orthopaedic procedures are the third surgical category used in neurorehabilitation. These types of procedures are appropriate in situations where deformities exist and improvement of joint position or a rebalancing of the forces acting on the joint will lead to improved function, cosmesis or ease of caregiving [7, 8]. Orthopaedic surgery is generally used to address one or more of the following aims:
- Release or lengthening of hypertonic/contracted muscles
- Augmentation of weak or paralysed muscles
- Stabilisation of joints [3].
Depending on the degree to which a person’s upper limb is affected by hypertonicity/spasticity or secondary adaptive changes (see Section 2.4.3), a number of surgical aims may be identified and, therefore, several procedures may be warranted [3, 6]. While there is debate regarding whether these procedures should be performed in incremental steps or simultaneously [9], multilevel orthopaedic surgery is often recommended, provided that the operative plan is carefully developed [7, 10, 11].
Table 10.1 presents the common procedures used to achieve surgical aims in people with brain injury, definition of the procedures used and examples of how each may be used in the upper limb. When making decisions about the type of procedure to undertake, surgeons need to consider a number of factors. For example, when active contraction of antagonists exists, muscle and tendon lengthening alone might be appropriate, but if no active movement is expected and the aim is repositioning of joints to improve hygiene management and comfort, then surgery may be targeted towards contracture release (see Figure 10.1) [3, 12]. Muscle transfers may be used when antagonists (e.g. wrist extensors) are weak, however, the mechanical properties of muscle affected by hypertonia mean that when a muscle is transferred to a new location it can become stiffer over time post-surgery (see Section 2.4.3), leading to over-correction of the deformity and possibly development of the opposite deformity, for example, excess wrist extension after flexor muscle transfer for correction of wrist flexion [8, 13]. The action of some muscle groups across a number of joints also requires consideration; for example, lengthening biceps or wrist flexors may have an impact on pronation as the former muscle group acts as an accessory supinator and the latter acts as an accessory pronator. Similarly, augmenting wrist extensors using tendon transfer may lead to increased finger flexion if hypertonicity or contracture exists in the finger flexors [3, 10]. Stabilisation of joints using arthodesis tends to be reserved for the most severe deformities as it results in a fixed position with active and passive joint movement no longer possible [3]. Considerations and implications for function regarding surgery are described in Box 10.1.
Table 10.1 Common orthopaedic surgical procedures used in neurorehabilitation [3, 8, 10, 12, 22, 23].
| Aim | Procedure | Description | Examples |
| Release or lengthen hypertonic or contracted muscle(s) |
|
| Severe wrist and finger flexion deformity (Type 3 Zancolli &Zancolli [Z&Z] hand classification):
|
|
| Elbow flexion contracture:
| |
|
| Thumb adduction/flexion deformity:
| |
|
| MCP and IP finger flexion contracture:
| |
|
| Less than 20° wrist flexion, active finger extension (Z&Z Type 1):
Swan-neck deformity:
| |
|
| Elbow flexion contracture:
| |
| Augment weak or paralysed muscle(s) |
|
| More than 20° wrist flexion (Z&Z Type 2b):
|
|
| Shoulder internal rotation:
| |
| Stabilise joints |
|
| Wrist flexion deformity:
|
|
| Thumb adduction/MCP hypermobility (HGF Group 4) with/without IP flexion:
|
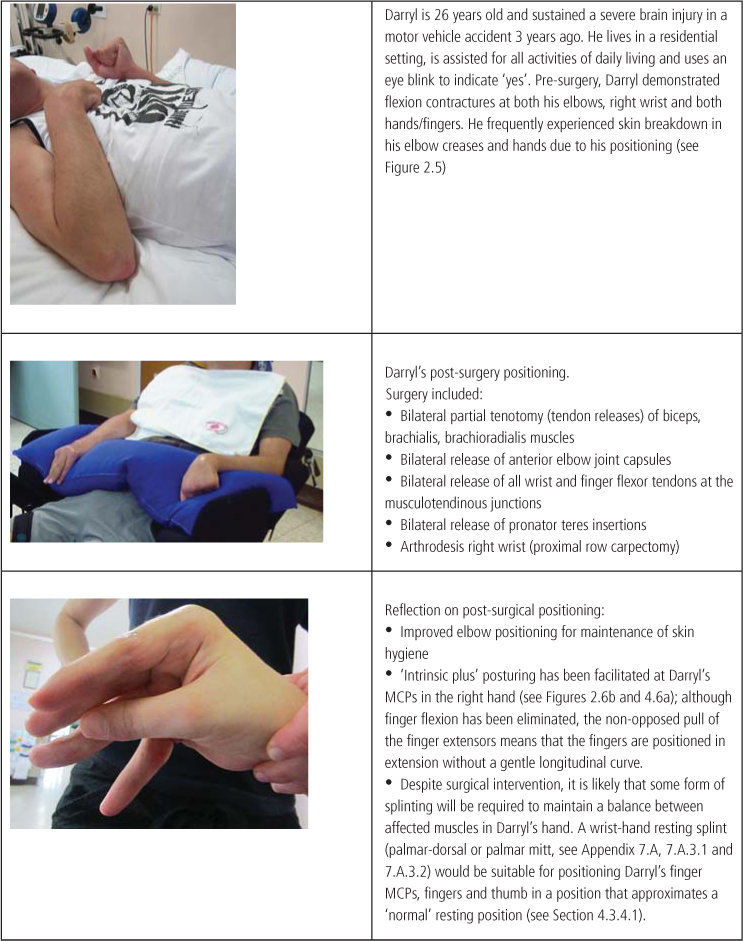
Figure 10.1 Description of, and reflection on, orthopaedic surgery for a person with a severe traumatic brain injury.
10.2 Surgery: A narrative review
The effectiveness of surgery for children and adults with upper limb impairment due to brain injury is considered here by means of a narrative review of the literature (see Section 7.2). A search for Cochrane reviews and systematic reviews was conducted; one Cochrane review focusing on surgery for thumb-in-palm deformity [14], two systematic reviews of surgery for heterotopic ossification [5, 16] and one literature review on functional outcome after surgical management of the hand in cerebral palsy were located [17]. A number of prospective studies were found but most studies were descriptive and involved retrospective analysis of clinical records. In addition, the vast majority of studies were related to children with cerebral palsy. Given the paucity of high quality research available, studies were chosen on the basis that their content provided some guidance to the clinician regarding the potential benefits of different types of surgical procedures and the different expectations of surgery that might be realistic for clients with different upper limb characteristics.
10.2.1 Dorsal rhizotomy
Although dorsal rhizotomy is primarily aimed at reducing lower limb spasticity, a retrospective review of 154 people who had selective posterior rhizotomy of lumbar and sacral nerve roots (partial sectioning of the nerve roots from L1-S1) suggested that upper limb spasticity was also reduced in 65% of cases (it was not clear to what extent this occurred) [18]. Dorsal rhizotomy has been used for reducing spasticity in the upper limbs [19], particularly when cervical nerve roots (C1-3) have been targeted [20, 21]. However, despite this reduction, minimal functional improvement has been described [2]. In contrast, encouraging results have been described for 20 children with hemiplegic cerebral palsy after dorsal rhizotomy at the level of the brachial plexus. Clinical measures indicated a statistically significant reduction of hypertonicity (more than 2 grades on the Modified Ashworth Scale of Muscle Spasticity [MASMS] for most muscle groups in 95% of participants), which was maintained at the 15 month follow-up, as well as improvements to active movement and grasp [19]. Further research into this technique using more rigorous methodology may be worth pursuing.
10.2.2 Neurotomy
A small number of early studies using selective peripheral neurotomy for reduction of spasticity at the elbow and shoulder reported positive results for adults with brain injury [24, 25]. However, a larger cohort of 52 children with cerebral palsy indicated that some degree of persistent spasticity remained in around a third of the study participants after neurotomy of the musculocutaneous nerve to reduce elbow spasticity [26]. A smaller, more recent study investigated the results of neurotomy at the shoulder for five children with cerebral palsy and marked shoulder external rotation patterning. Hypertonicity reduced from moderate or severe (2 or 3 on the MASMS, see Table 4.2) to no increase in muscle tone (MASMS 0), while active shoulder internal rotation was significantly increased [27].
Documented research of the efficacy of below-elbow peripheral neurotomies is similarly sparse, and most papers are descriptions of the surgical procedure rather than outcome studies. A few recent studies investigating selective median, or median and ulnar, neurotomy have demonstrated some degree of reduced hypertonicity and some functional or cosmetic changes. However, pre- and post-surgical measures have generally been performed by the clinical team, without establishing a baseline or reliability and validity of the measures used. For example, a retrospective study was conducted for 22 adults with stroke, traumatic brain injury and cerebral palsy to determine the effects of selective median nerve neurotomy. Participants were an average of eight years post-injury and presented with severe wrist and finger hypertonicity. MASMS scores were taken as part of the usual clinical process and were documented as severe (an average of 3.27) prior to surgery and as mild-moderate (an average of 1.82, 1.73 and 1.77) at 3, 6 and 12 months respectively, post-surgery [28]. In another study, 10 adult participants, also with varied diagnoses, underwent neurotomies of both the median and ulnar nerves. These participants were rated as having severe or very severe hypertonicity (MASMS 3 or 4) and little or no active function. The procedure was more effective for some participants than others, with post-surgery hypertonicity measured as severe (MASMS 3; n = 1, 10%), moderate (MASMS 1+ or 2; n = 5, 50%) and mild (MASMS 0 or 1; n = 4, 40%). Recurrence of hypertonicity was apparent for one participant and transient paresis for another. Hand posture improved for 90% and pain reduced for 50% of the participants [29].
Maarawi et al. [30] performed median and/or ulnar nerve neurotomies for 31 adults who had moderate to severe spasticity (MASMS average of 2.14–3.64 across various muscle groups) and varying levels of functional ability. Participants were divided into two groups according to the surgical goal, with 11 (36.6%) aiming for a movement-related goal and 20 (63.4%) aiming for improved comfort or cosmesis. Follow-up continued for an average of four-and-a-half years, with measures taken as part of usual clinical procedures. Hypertonicity scores on the MASMS reduced significantly across the participant group (average of 0.6–2.28 in the various muscle groups). Of those with a movement goal, most (81.85%) achieved hand opening post-surgery and reported subjective improvements in daily activities. For the remaining participants who aimed for improved comfort or cosmesis, 40% achieved small improvements in hand movement, 90% reported improved cosmesis and hygiene, and 50–75% reported improvements to self-care, dressing or leisure. Five people (15%) had recurrent spasticity requiring another procedure, and five experienced complications including haemotoma, hypesthesia and transient paresis.
While the available research has methodological issues and indicates mixed outcomes, it nevertheless suggests that some clients may benefit from neurotomy. Further methodologically sound research is recommended, with researchers also advising that clients need to be carefully selected for this procedure to determine the relative contribution of spasticity to the person’s functional limitations and deformity [22, 29, 30].
10.2.3 Muscle and tendon releases
Several recent retrospective clinical studies have indicated improvements to shoulder and elbow positioning, PROM, AROM and hypertonicity after muscle and tendon releases alone, with some functional improvements noted anecdotally. Two studies conducted by Namdari et al. [12, 31] tracked cohorts of 29 and 36 adults with hemiplegia due to stroke or brain injury, severe hypertonicity, contractures and no voluntary movement who had undergone elbow and shoulder releases, respectively. Elbow releases, including biceps, brachialis and brachioradialis muscles, led to increased PROM (from an average lack of 78° to 17°), and reduced hypertonicity from severe (MASMS 3.3) to mild (MASMS 1.4) at 1.7 years post-surgery. Only one recurrence of contracture was reported, and occurred due to lack of splint wearing and participation in rehabilitation post-surgery [31]. Full shoulder releases included tenotomies of pectoralis major, latissimus dorsi, teres major and subscapularis muscles. Passive shoulder range in all directions of movement improved by 35–55% of normal PROM and was retained at follow up one year later. However, hypertonicity at the shoulder only reduced slightly [12]. Participants noted improvements to skin hygiene and/or dressing in both studies. These findings echo those of another study conducted with adults with brain injury due to various diagnoses, in which elbow and shoulder releases led to improved ratings for ease of caregiving, even though PROM did not increase quite as much at the elbow (average 28°) [32]. In relation to children with cerebral palsy, a retrospective review of outcomes for 13 children who underwent pectoralis major releases indicated that greater than 90° of shoulder abduction was retained for 10 children (77%) 12 months post-surgery.
Research that has investigated similar surgical procedures with participants who have contractures but retain some voluntary control demonstrate similar changes to PROM, small changes to hypertonicity and moderate to substantial changes in active movement [22, 33]. Carlson et al. [22] compared two different surgical procedures for 86 children and young people with cerebral palsy, depending on their degree of elbow contracture. Those with contracture greater than 45° underwent extensive elbow releases while those with less significant contractures had partial muscle lengthenings. After surgery, the elbow was held in a straighter position when walking for both groups of participants. Those who had full releases gained more active elbow extension but also lost some active flexion. Unlike the majority of research in this area, Carlson’s study used an independent assessor who viewed participant videotapes, thus improving methodological rigour. Another study found that releases at the shoulder and/or elbow led to small improvements in clients’ capacity for bimanual tasks, but these changes did not improve performance in daily-living skills [32].









