7 Surgical Anatomy of EC-IC Bypass Procedures
Introduction
The number of cerebral revascularization procedures performed by neurosurgeons has declined after the Cooperative Study of Extracranial-Intracranial Arterial Anastomosis1 failed to demonstrate that this procedure reduced the risk of stroke in patients with cerebral ischemia. However, cerebral revascularization is now well recognized as an important element in the treatment of complex intracranial aneurysms, cranial base tumors, and certain kinds of ischemic diseases.
Results
Arterial Relationships
The diameters of vessels measured, which are frequently used for cerebral revascularization procedures, are shown in Tables 7–1 and 7–2.
Table 7–1 Diameter of Vessels for Cerebral Revascularization in Anterior Circulation (MM).
| ICA |
| Cervical segment: 8.57 ± 1.34 Petrous segment: 5.42 ± 0.68 Supraclinoid segment: 3.95 ± 0.56 |
| ECA |
| Cervical portion: 5.75 ± 0.94 |
| STA |
| At the level of zygoma: 1.93 ± 0.48 |
| MCA |
| M2 (largest branch near the central sulcus): 1.76 ± 0.36 M4 (largest branch in the area) Frontal branch: 1.19 ± 0.32 Temporal branch: 1.22 ± 0.23 Parietal branch: 1.36 ± 0.24 |
| ACA |
| A2: 2.35 ± 0.60 A3: 1.98 ± 0.35 A4: 1.94 ± 0.40 A5: 1.55 ± 0.12 |
Table 7–2 Diameter of Vessels for Cerebral Revascularization in Posterior Circulation (MM).
| PCA |
| P2A: 2.13 ± 0.38 P2P: 1.73 ± 0.33 P3: 1.67 ± 0.16 |
| SCA |
| Anterior pontomesencephalic segment: 1.67 ± 0.16 Lateral pontomesencephalic segment Single trunk: 1.51 ± 0.12 Rostral trunk: 1.25 ± 0.17 Caudal trunk: 1.15 ± 0.30 |
| AICA |
| Anterior pontomesencephalic segment: 1.34 ± 0.28 Cortical segment: 1.07 ± 0.29 |
| PICA |
| Anterior medullary segment: 1.84 ± 0.45 Tonsillomedullary segment (caudal loop): 1.68 ± 0.38 |
| OA |
| At the digastric groove: 2.05 ± 0.48 At the level of the superior nuchal line: 2.01 ± 0.45 |
Internal carotid artery
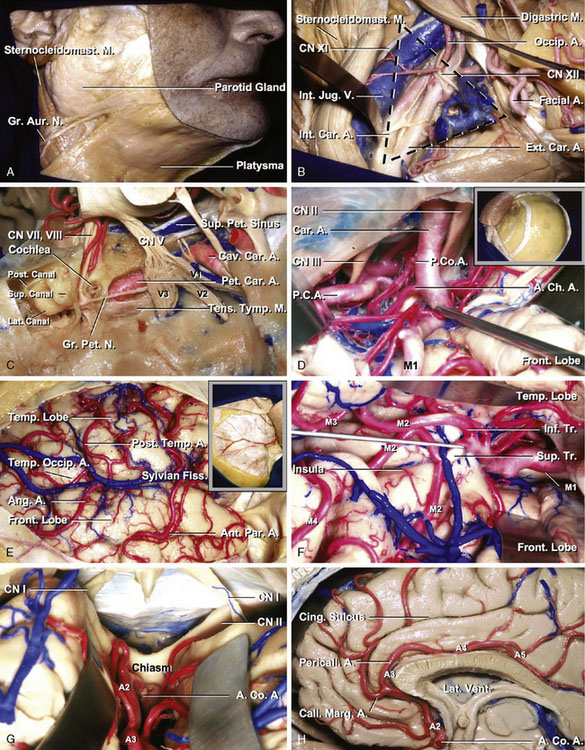
The common carotid artery divides into the internal (ICA) and external carotid artery (ECA) at the level of C2-C3 below the mandibular angle. The cervical, petrous, and supraclinoid ICAs are the sites of cerebral revascularization procedures. The average diameters of the cervical, petrous, and supraclinoid ICAs were 8.57, 5.42, and 3.95 mm, respectively (Table 7–1). The cervical portion of the ICA is covered by the skin, superficial cervical fascia, platysma, deep fascia, anterior margin of the sternocleidomastoid muscle, and internal jugular vein. Dissecting these anatomic structures exposes the carotid triangle, which is formed by the posterior belly of the digastric, omohyoid, and sternocleidomastoid muscles. In the carotid triangle, the ICA begins at the bifurcation of the common carotid, opposite the upper border of the thyroid cartilage, and runs perpendicularly upward, in front of the transverse processes of the upper three cervical vertebrae, to the carotid canal in the petrous portion of the temporal bone (Figures 7–1A and 7–1B).
The petrous portion of the ICA courses within the carotid canal and ends where the artery enters the cavernous sinus. The carotid artery, at the point where it enters the carotid canal, is surrounded by a strong layer of connective tissue that makes it difficult to mobilize the artery. The roof of the carotid canal opens below the trigeminal ganglion near the distal end of the carotid canal. The greater petrosal nerve runs beneath the dura of the middle fossa, immediately superior and anterolateral to the horizontal segment of the petrous carotid. The cochlea lies below the floor of the middle fossa, just posterosuperior to the lateral genu of the petrous carotid artery. The Eustachian tube and the tensor tympani muscle are located parallel to and along the anterior margin of the horizontal segment, where they are separated from the artery by a thin layer of bone (Figure 7–1C).
The supraclinoid segment of the ICA begins where the artery emerges from the dura mater and enters the cranial cavity by passing along the medial side of the anterior clinoid process and below the optic nerve. It reaches the lateral side of the optic chiasm and bifurcates below the anterior perforated substance at the medial end of the sylvian fissure to give rise to the anterior cerebral artery (ACA) and middle cerebral artery (MCA). The supraclinoid segment of the ICA gives rise to three branches: the ophthalmic, posterior communicating, and anterior choroidal arteries. In addition, this segment gives off perforating branches including the superior hypophyseal artery (Figure 7–1D).
External carotid artery
The external carotid artery (ECA) begins at the bifurcation of the common carotid in front of the ICA and ascends backward to the space behind the neck of the mandible, where it divides into the superficial temporal and maxillary arteries. The average diameter of the ECA was 5.75 mm (Table 7–1). The ECA is crossed by the hypoglossal nerve, common facial and superior thyroid veins, and the digastric and stylohyoid muscles. The superior thyroid artery arises from the external carotid artery just below the level of the greater cornu of the hyoid bone and ends in the thyroid gland. The STA, the smaller of the two terminal branches of the ECA, appears, from its direction, to be the continuation of that vessel. The STA plays an important role as a donor vessel in cerebral revascularization. The STA begins in the substance of the parotid gland, behind the neck of the mandible, and crosses over the posterior root of the zygomatic process of the temporal bone. The average diameter of the STA at the level of the zygoma was 1.93 mm (Table 7–1). The STA divides into two branches, frontal and parietal. The frontal branch (anterior temporal) runs tortuously upward and forward to the forehead, supplying the muscles, integument, and pericranium in this region, and anastomosing with the supraorbital and frontal arteries. The parietal branch (posterior temporal), larger than the frontal, curves upward and backward on the side of the head, lying superficial to the temporal fascia and anastomosing with its fellow of the opposite side and with the posterior auricular and occipital arteries (Figure 7–1B).
Middle cerebral artery
M2 and M4 are the sites of cerebral revascularization procedures. The M2 segment includes the trunk that lie on and supply the insula. This segment begins at the genu where the middle cerebral artery (MCA) trunk passes over the limen insulae and terminates at the circular sulcus of the insula. The greatest branching of the MCA occurs distal to the genu as these trunks cross the anterior part of the insula. The M2 branches are used for a bypass procedure, especially for a high-flow bypass. Important factors in selecting an artery for the procedure are its diameter, the length of artery available on the cortical surface, and perforating arteries to the basal ganglia. The average diameter of the largest branch near the central sulcus of the insula was 1.76 mm (Table 7–1).
The M4 is composed of the branches to the lateral convexity. They begin at the surface of the sylvian fissure and extend over the cortical surface of the cerebral hemisphere. The largest cortical artery is the temporo-occipital artery. Nearly two-thirds are 1.5 mm or more in diameter, and 90% are 1 mm or more in diameter. The smallest cortical artery is the orbitofrontal artery; approximately one-quarter are 1 mm or more in diameter. The average diameters of the largest M4 in the parietal, temporal, and frontal area were 1.36, 1.22, and 1.19 mm, respectively (Table 7–1). The central sulcal artery is the largest branch to the frontal lobe, and the angular artery is the largest branch to the parietal lobe. The temporo-occipital and the posterior temporal arteries are the largest branches to the temporal lobe. The minimum length of a cortical artery needed to complete a bypass is 4 mm. The angular, posterior parietal, and temporo-occipital arteries have the longest segments on the cortical surface, and the orbitofrontal and temporopolar arteries have the shortest cortical segment (Figures 7–1E and 7–1F).
Anterior cerebral artery
The anterior cerebral artery (ACA) is divided at the anterior communicating artery (AComA) into two parts, proximal (A1) and distal (A2–5). The A3 segment of the ACA is the dominant site of cerebral revascularization procedures, including side-to-side anastomosis and short arterial and venous interposition grafting. The average diameters of A2, A3, A4, and A5 were 2.35, 1.98, 1.94, and 1.55 mm, respectively (Table 7–1). The pericallosal artery is the portion of the ACA distal to the AComA and is constantly present. The pericallosal artery ascends in front of the lamina terminalis to pass into the interhemispheric fissure (A2). Above the lamina terminalis, the artery makes a smooth curve around the genu of the corpus callosum (A3) and then courses backward above the corpus callosum in the pericallosal cistern (A4 and A5).
The callosomarginal artery is defined as the artery that courses in or near the cingulate sulcus and gives rise to two or more major cortical branches.2 When the callosomarginal artery is well formed, it lies in the cingulate sulcus above the cingulate gyrus and follows a course roughly parallel to that of the pericallosal artery. Its origin varies from just distal to the AComA to the level of the genu of the corpus callosum. Its frequent origin was from the A3 segment, followed by the A2 segment and AComA. The size of the pericallosal artery distal to the callosomarginal origin varies inversely with the size of the callosomarginal artery (Figures 7–1G and 7–1H).
Posterior cerebral artery
The posterior cerebral artery (PCA) arises at the basilar bifurcation, is joined by the posterior communicating artery (PComA) at the lateral margin of the interpeduncular cistern, encircles the brainstem passing through the crural and ambient cisterns to reach the quadrigeminal cistern, and is distributed to the posterior part of the hemisphere. The PCA supplies not only the posterior part of the cerebral hemispheres, but also sends critical branches to the thalamus, midbrain, and other deep structures, including the choroid plexus and walls of the lateral and third ventricles. Each segment of the PCA is classified according to our already proposed system.3 The P1 is the segment proximal to the PComA. The P2 segment extends from the PComA to the point at which the PCA enters the quadrigeminal cistern. The P2 segment is subdivided into equal anterior (P2A) and posterior (P2P) halves. The P2A begins at the PComA and courses between the cerebral peduncle and uncus that forms the medial and lateral walls of the crural cistern, and inferior to the optic tract and basal vein that crosses the roof of the cistern, to enter the proximal portion of the ambient cistern. The P2P begins at the posterior edge of the cerebral peduncle at the junction of the crural and ambient cisterns. It courses between the lateral midbrain and the parahippocampal and dentate gyri, which form the medial and lateral walls of the ambient cistern, below the optic tract, basal vein, and geniculate bodies and the inferolateral part of the pulvinar in the roof of the cistern, and superomedial to the trochlear nerve and tentorial edge. The P3 segment begins at the posterior midbrain, courses within the quadrigeminal cistern, and ends at the anterior limit of the calcarine fissure. The P4 segment is the distal branch of the P3 segment. The average diameters of P2A, P2P, and P3 were 2.13, 1.73, and 1.67 mm, respectively (Table 7–2). The PCA gives rise to three types of branches:1 central perforating branches to the diencephalon and midbrain,2 ventricular branches to the choroid plexus and walls of the lateral and third ventricles and adjacent structures,3 and cerebral branches to the cerebral cortex and splenium of the corpus callosum. The central branches include the direct and circumflex perforating arteries, including the thalamoperforating, peduncular perforating, and thalamogeniculate arteries. The ventricular branches are the lateral and medial posterior choroidal arteries. The cerebral branches include the inferior temporal group of branches, which are divided into hippocampal and the anterior, middle, posterior, and common temporal branches, plus the parieto-occipital, calcarine, and splenial branches. The long and short circumflex, thalamoperforating, and medial posterior choroidal arteries arise predominantly from P1, and the other PCA branches most frequently arise from P2 or P3. The hippocampal, anterior temporal, peduncular perforating, and medial posterior choroidal arteries most frequently arise from P2A. The middle temporal, posterior temporal, common temporal, and lateral posterior choroidal arteries most frequently arise from P2P. The thalamogeniculate arteries arise only slightly more frequently from P2P than from P2A. The calcarine and parieto-occipital arteries most frequently arise from P3 (Figure 7–2A).
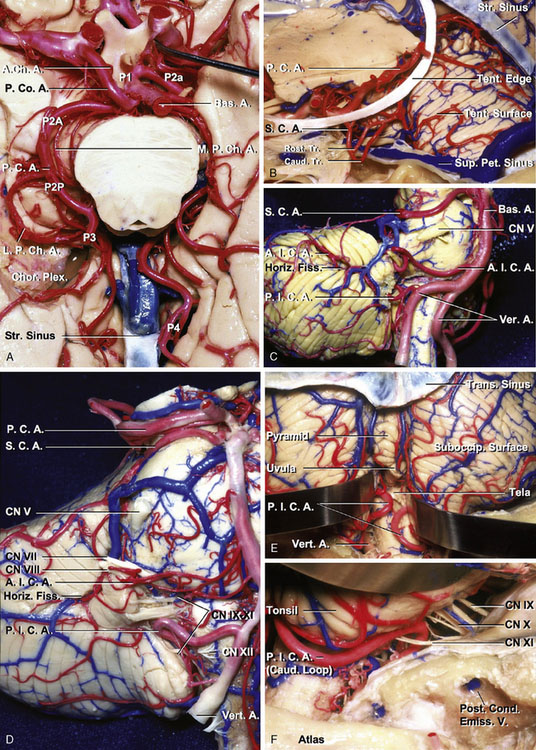
Figure 7–2 Arterial relationships. A and B. Inferior and anterosuperior views, PCA. The PCA arises at the basilar bifurcation, is joined by the PComA at the lateral margin of the interpeduncular cistern, encircles the brainstem passing through the crural and ambient cisterns to reach the quadrigeminal cistern above the edge of the cerebellar tentorium, and is distributed to the posterior part of the hemisphere. The PCA is divided into P1 to P4. The PCA gives rise to three types of branches:1 central perforating branches to the diencephalon and midbrain,2 ventricular branches to the choroid plexus and walls of the lateral and third ventricles and adjacent structures,3 and cerebral branches to the cerebral cortex and splenium of the corpus callosum. C and D. Anterolateral and anterior views of the brainstem and the cerebellum, SCA, AICA, and PICA. The SCA arises in front of the midbrain, usually from the basilar artery near the apex, and passes below the oculomotor nerve. Its proximal portion courses medial to the free edge of the tentorium cerebelli around the brainstem near the pontomesencephalic junction, and its distal part passes below the tentorium, making it the most rostral of the infratentorial arteries. All of the SCAs that arise as a single vessel bifurcate into two major trunks, one rostral and one caudal, most commonly near the point of maximal caudal descent of the artery on the lateral side of the brainstem (B). The AICA originates from the basilar artery, usually as a single trunk, and encircles the pons near the abducent, facial, and vestibulocochlear nerves. After coursing near and sending branches to the nerves entering the acoustic meatus and to the choroid plexus protruding from the foramen Luschka, it passes around the flocculus on the middle cerebellar peduncle to supply the cerebellopontine fissure and the petrosal surface. The PICA arises from the vertebral artery near the inferior olive and passes posteriorly around the medulla. E and F. Posterior and posterolateral views of the brainstem and the cerebellum and PICA. After passing the lateral aspect of the medulla, the PICA courses around the cerebellar tonsil and enters the cerebellomedullary fissure and passes posterior to the lower half of the roof of the fourth ventricle. On exiting the cerebellomedullary fissure, its branches are distributed to the vermis and hemisphere of the suboccipital surface. In the tonsillomedullary segment of the PICA, the loop passing near the lower part of the tonsil, referred to as the caudal loop, forms a caudally convex loop that coincides with the caudal pole of the tonsil, but it may also course superior or inferior to the caudal pole of the tonsil without forming a loop. The telovelotonsillar segment commonly forms a loop with a convex rostral curve, called the cranial loop. The apex of the cranial loop usually overlies the central part of the inferior medullary velum. A., artery; A.Ch.A., anterior choroidal artery; A.I.C.A., anterior inferior cerebellar artery; Bas., basilar; Caud., caudal; Chor. Plex., choroid plexus; CN, cranial nerve; Cond., condylar; Emiss., emissary; Fiss., fissure; Horiz., horizontal; L.P.Ch.A., lateral posterior choroidal artery; M.P.Ch.A., medial posterior choroidal artery; P.C.A., posterior cerebral artery; P.Co.A., posterior communicating artery; Pet., petrosal; P.I.C.A., posterior inferior cerebellar artery; Post., posterior; Rost., rostral; S.C.A., superior cerebellar artery; Str., straight; Suboccip., suboccipital; Sup., superior; Tent., tentorial; Tr., trunk; Trans., transverse; V., vein; Vert., vertebral.
Superior cerebellar artery
The superior cerebellar artery (SCA) arises in front of the midbrain, usually from the basilar artery near the apex, and passes below the oculomotor nerve. Its proximal portion courses medial to the free edge of the tentorium cerebelli around the brainstem near the pontomesencephalic junction, and its distal part passes below the tentorium, making it the most rostral of the infratentorial arteries. All of the SCAs that arise as a single vessel bifurcate into two major trunks, one rostral and one caudal, most commonly near the point of maximal caudal descent of the artery on the lateral side of the brainstem. The SCA is divided into four segments: anterior pontomesencephalic, lateral pontomesencephalic, cerebellomesencephalic, and cortical. The anterior pontomesencephalic segment begins at the origin of the SCA and extends below the oculomotor nerve to the anterolateral margin of the brainstem. The average diameter of the vessel was 1.67 mm in the segment (Table 7–2). The lateral pontomesencephalic segment begins at the anterolateral margin of the brainstem and frequently dips caudally onto the lateral side of the pons. This segment terminates at the anterior margin of the cerebellomesencephalic fissure. The average diameters of rostral and caudal trunks in this segment were 1.25 and 1.15 mm, respectively. If it is a single trunk, the average diameter was 1.51 mm in the segment (Table 7–2). The cerebellomesencephalic segment courses within the cerebellomesencephalic fissure, giving off branches that penetrate fissure’s opposing walls. The cortical segment includes the branches distal to the cerebellomesencephalic fissure that pass under the tentorial edge and are distributed to the tentorial surface (Figures 7–2B through 7–2D).
Anterior inferior cerebellar artery
The anterior inferior cerebellar artery (AICA) originates from the basilar artery, usually as a single trunk, and encircles the pons near the abducent, facial, and vestibulocochlear nerves. After coursing near and sending branches to the nerves entering the acoustic meatus and to the choroid plexus protruding from the foramen Luschka, it passes around the flocculus on the middle cerebellar peduncle to supply the cerebellopontine fissure and the petrosal surface. It commonly bifurcates near the facial-vestibulocochlear nerve complex to form a rostral and a caudal trunk. The AICA is divided into four segments: anterior pontine, lateral pontine, flocculonodular, and cortical. Each segment may include more than one trunk, depending on the level of bifurcation of the artery. The average diameters of the anterior pontine and cortical segments were 1.34 and 1.07 mm, respectively (Table 7–2). The most common pattern is for the AICA to supply the majority of the petrosal surface, but overlap of the SCA onto the upper part of the petrosal surface and the PICA onto the lateral part of the suboccipital surface is not uncommon, depending on the size of the AICA (Figures 7–2C and 7–2D).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree