15 I. Lifetime incidence of low back pain estimated at 80% of general population A. Fourteen percent of new patient visits to physicians are related to lower back pain. B. Second only to respiratory infections as the most common cause of work absence II. One hundred sixty-five lumbar spine operations per 100,000 individuals occur each year in United States A. Lumbar fusion for discogenic pain and lumbar laminectomies for radicular symptoms are the most common spine surgeries performed. III. Risk factors for low back pain A. Previous history of low back pain B. Increasing age C. Smoking D. Medical comorbidities E. Lower socioeconomic status F. Psychological distress G. Heavy occupational demands I. Idiopathic or nonspecific A. Up to 85% without specific diagnosis II. Degenerative disc disease A. Discogenic pain B. Disc herniation III. Developmental A. Isthmic spondylolisthesis B. Idiopathic scoliosis IV. Congenital V. Traumatic VI. Infectious A. Osteomyelitis B. Discitis VII. Inflammatory A. Ankylosing spondylitis VIII. Neoplastic IX. Metabolic A. Osteoporosis X. Referred A. Dissecting aortic aneurysm B. Renal vein thrombosis C. Acute myocardial infarction D. Pancreatitis E. Duodenal ulcer XI. Red flags in clinical presentation that require further investigation A. History of significant trauma B. History of previous malignancy C. Age >50 years D. Systemic symptoms (fever, chills, anorexia, recent weight loss) E. Severe progressive neurological deficit 1. Especially saddle anesthesia or bowel/bladder dysfunction F. Ongoing infection G. History of immunosuppression I. Establishing a pathoanatomic diagnosis is the key to successful surgical outcomes (Table 15–1). II. Arriving at a conclusive diagnosis is not possible in as many as 85% of patients who are categorized as having “idiopathic low back pain.” III. Plain Radiographs A. Flexion-extension films 1. May demonstrate dynamic instability B. Oblique films
Surgical Management of Axial Back Pain
♦ Introduction
♦ Etiologies
♦ Diagnostic Tools
| Intervertebral disks | Primary pain generator in setting of degenerative disk disease. Pain fibers present in the outer third of the anulus fibrosus. Biochemical factors that can mediate painful stimuli:
|
| Facet joints | Extensively innervated with pain fibers. Synovial folds of the joint lining also possess pain fibers. Proprioceptive nerve endings also present, which mediate protective muscular reflexes. |
| Musculoligamentous structures | Both anterior and Posterior Longitudinal Ligaments (PLL) possess sensory innervation. PLL has been found to have substance P-containing fibers. Unencapsulated nerve fibers found in paraspinal musculature respond to metabolites accumulated during prolonged muscle contraction or spasm. |
| Neural structures | Pain from mechanical nerve root compression is thought to require the presence of inflammation. Dorsal root ganglion sensitive to direct pressure and vibratory forces. Increase in genetic expression of neuropeptides (substance P) in response to mechanical nerve root compression. |
1. Helpful in evaluating the integrity of the pars intra-articularis in the setting of a spondylolisthesis
C. Lumbar spine films unnecessary for at least 4 weeks in a patient with new onset of low back pain without any of the previously mentioned red flags
IV. Computed tomography
A. Excellent visualization of the bony anatomy of the vertebral column
B. Not as good as magnetic resonance imaging (MRI) for visualization of soft tissue structures
C. Computed tomographic myelography is an excellent imaging modality for spinal stenosis, but MRI is used because it is less invasive.
V. MRI
A. Excellent axial, coronal, and sagittal visualization of soft tissues and neural structures both surrounding and within the vertebral column
B. Great for evaluation of neural compression within the canal and foramen
C. T2-weighted MRI shows darkening of the discs in disc degeneration due to loss of water, but this finding does not predict development of back pain in an asymptomatic patient.
A. Rationalized by the hypothesis that facet arthrosis contributes to low back pain
B. Not many well-designed studies to evaluate efficacy, and thus the use of injections to predict surgical outcomes for patients with low back pain is not supported.
VII. Discography
A. Highly controversial
B. Performed by the introduction of a needle into the nucleus pulposus and injection of contrast to visualize internal fissures or tears
C. Saline may also be injected into the disc to see if it provokes the pain that the patient has previously experienced.
D. Combination of pain with disc injection and findings of disc degeneration on post CT-Discography increase the likelihood that a particular disc is in volved in patient’s pain.
E. Important findings
1. Re-creation of pain with injection
2. Pain at low pressure
3. Disc accepts greater than 2 mL of dye
4. Dye extravasation from disc space
♦ General Surgical Indications
I. Mechanical instability
II. Neurological deficits
III. Indications for patients with low back pain without radicular symptoms
A. Unremitting pain and disability for more than 1 year
B. Failure of physical therapy and nonoperative treatment modalities
1. Nonsteroidal antiinflammatory drugs (NSAIDs), heat, ice, weight loss, activity modification
C. Absence of psychiatric disorders and compensation or ligation issues
D. Isolated single-level disc degeneration on MRI with concordant pain on discography or single-level static or dynamic instability
♦ Surgical Procedures
I. General principles
A. Low back pain management largely focuses on spinal fusion.
B. Decompression indicated in setting of leg pain and nerve root compression
C. Nucleus pulposus or intervertebral disc degeneration arthroplasty
1. Emerging options that are still being investigated
A. Prevents further segmental motion
1. More appropriate for spinal instability
B. Keys to attaining a solid arthrodesis
1. Meticulous preparation of the graft site (decortication)
2. Supplementation with appropriate type and amount of bone graft
3. Consideration of lumbar spine biomechanics
a. Maintaining or restoring the normal lordosis in the sagittal alignment of the lumbar spine
4. Optimizing systemic conditions that influence bone healing
a. Nicotine, corticosteroids, NSAIDs, nutrition, and infection
b. Concern for degeneration of adjacent levels to the fused segments mandates that minimum numbers of levels be fused, especially in younger individuals.
III. Techniques for achieving fusion in the lumbar spine
A. Summary of fusion techniques (Table 15–2)
B. Posterolateral intertransverse process fusion
1. Involves either posterior or posterolateral muscle-splitting approach
2. Involves decortication of transverse processes and placement of an autogenous bone graft along the transverse processes
3. Pseudarthrosis rate without instrumentation is estimated to be between 5 and 25%.
4. Instrumentation lowers pseudarthrosis rate to 5 to 10% but without accompanied improvement in clinical outcomes.
5. There is still some motion anteriorly that occurs after this procedure because of the intact disc anteriorly. Pain may persist if it is due to movement at the disc joint.
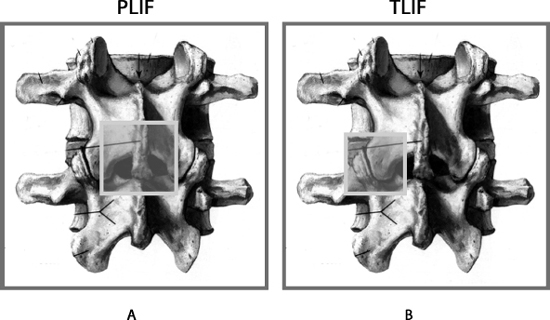
C. Posterior lumbar interbody fusion (Figs. 15–1, 15–2)
1. Extraction of much of the disc through posterior approach and wide laminectomy