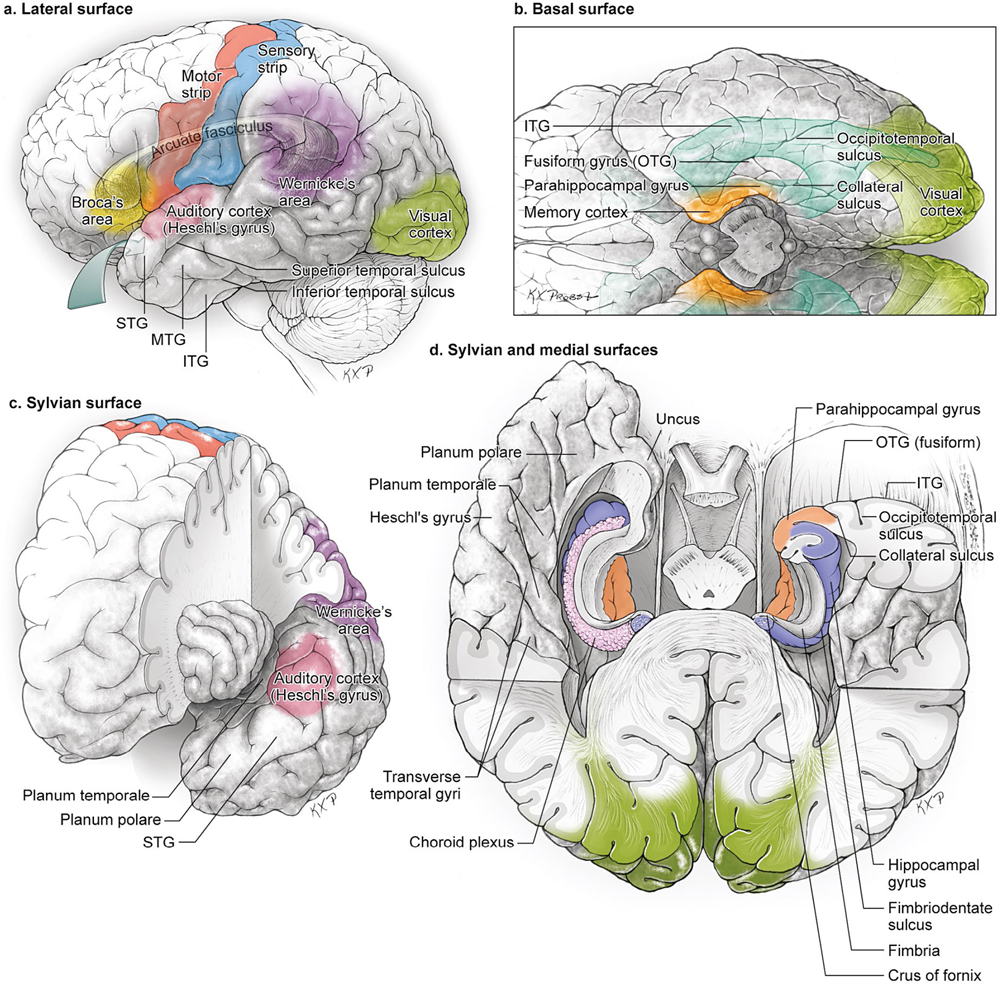
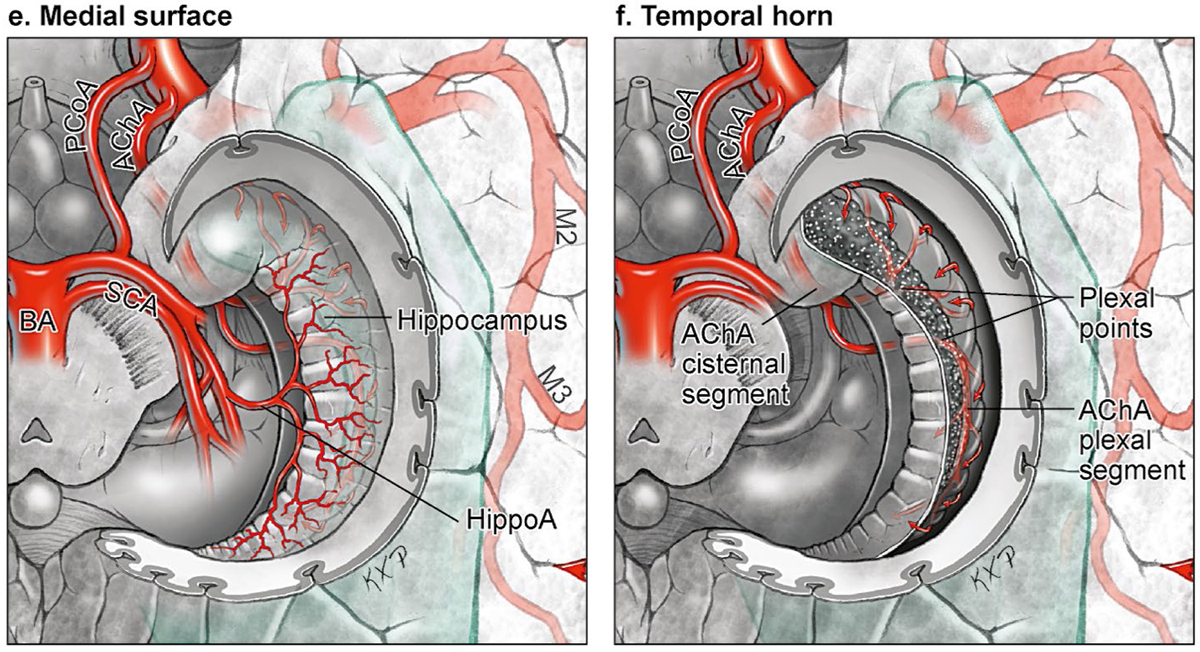
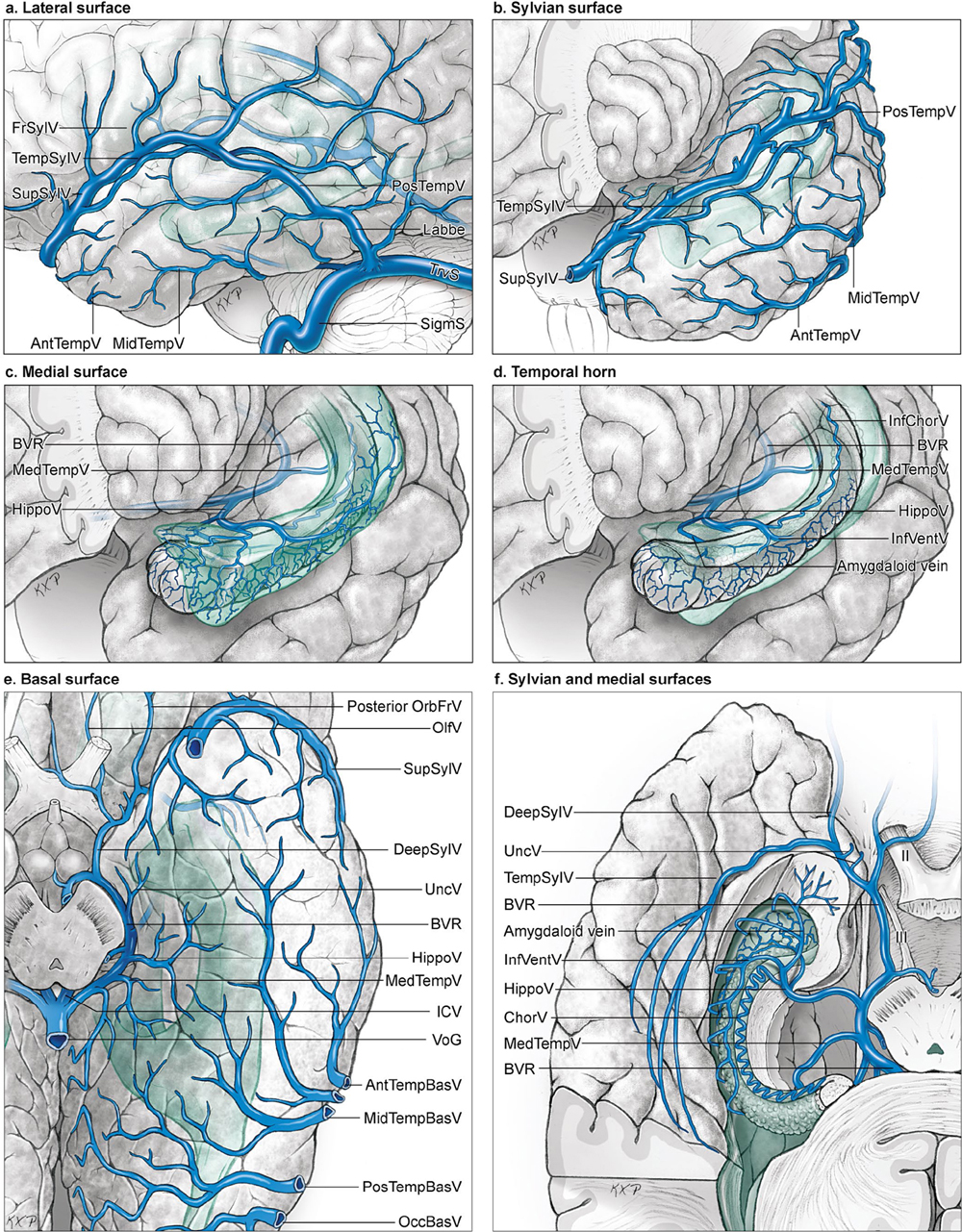
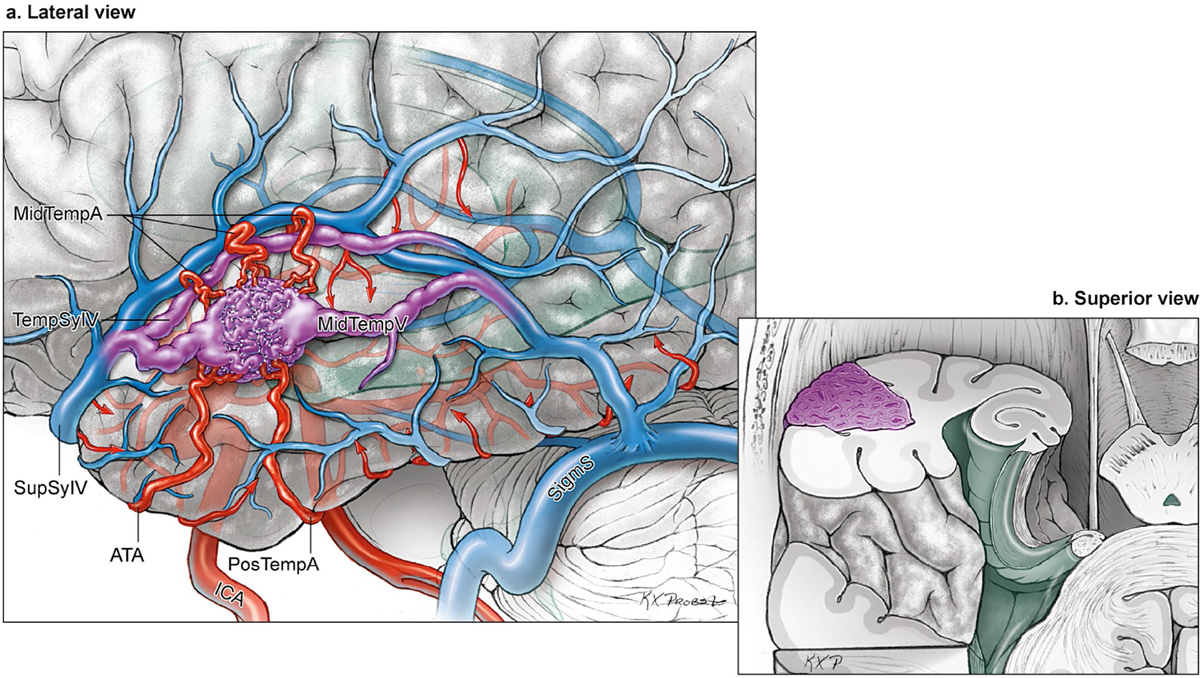
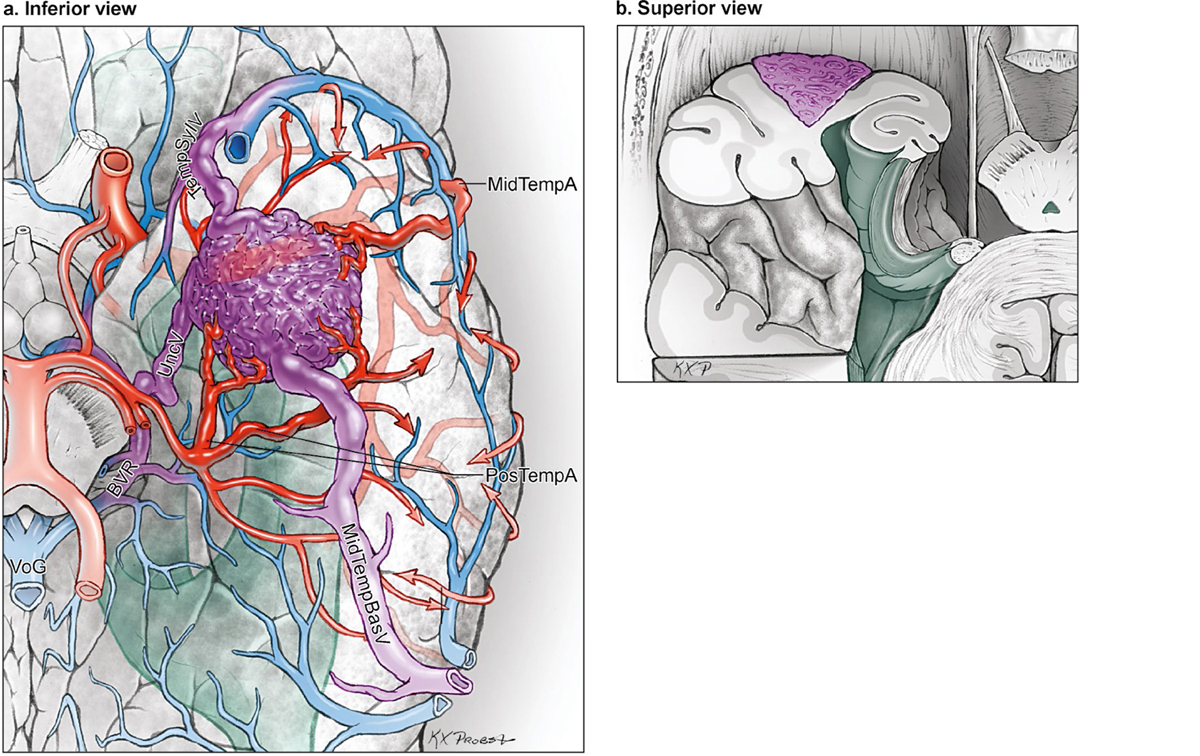
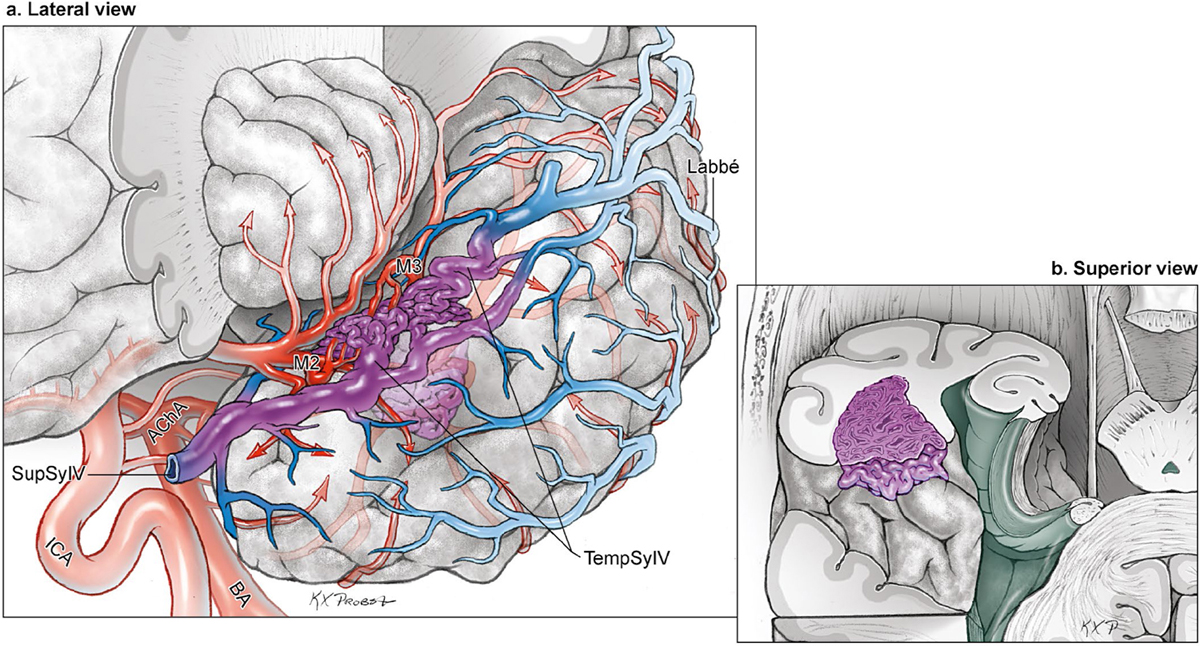
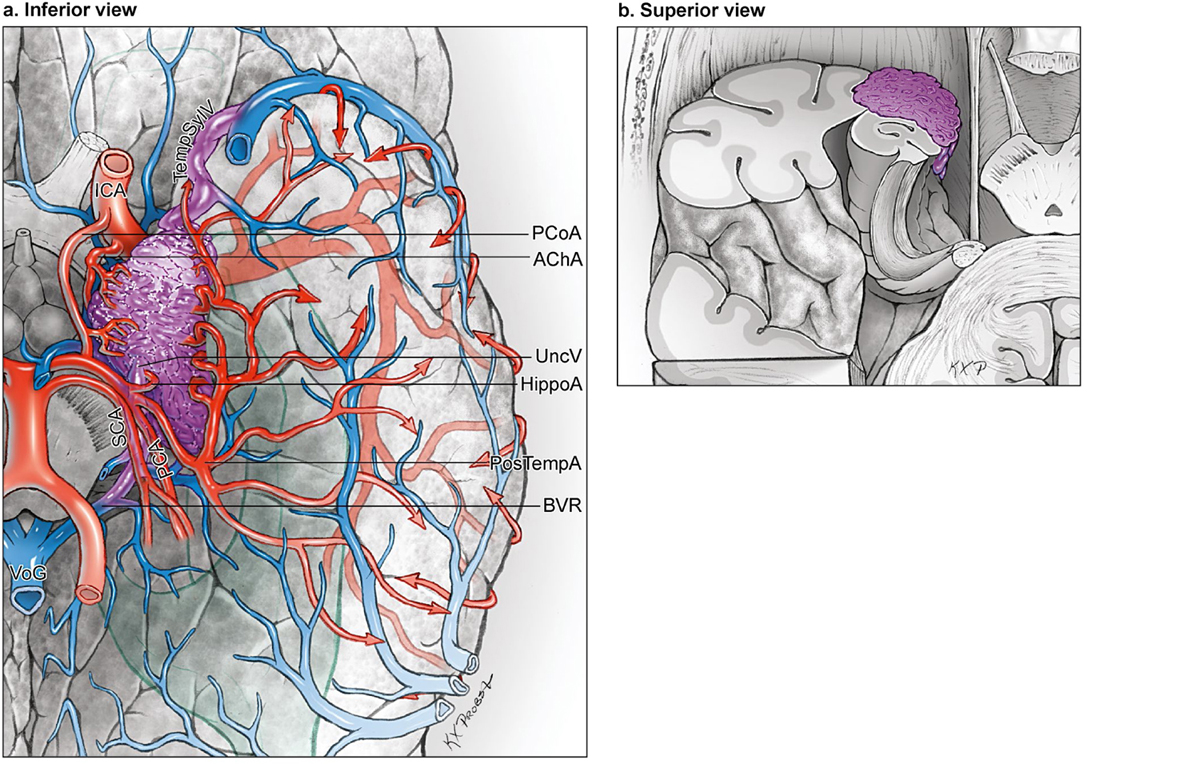
12 Temporal Arteriovenous Malformations The temporal lobe has four surfaces: lateral, basal, sylvian, and medial (Fig. 12.1). The lateral temporal surface consists of three horizontal gyri that lie below and run parallel to the sylvian fissure: superior, middle, and inferior temporal gyri (STG, MTG, and ITG). Superior and inferior temporal sulci separate the three gyri and lie above and below the MTG, respectively. The basal surface also consists of three longitudinal gyri: the lower portion of the ITG, the occipitotemporal (fusiform) gyrus (OTG), and the lower portion of the parahippocampal gyrus. The basal surface is traversed longitudinally by the occipitotemporal sulcus, which separates the fusiform gyrus from the ITG. The collateral sulcus lies between the fusiform and parahippocampal gyri and parallels the occipitotemporal sulcus. The medial temporal surface consists of the parahippocampal gyrus, uncus, and hippocampus (which is composed of the dentate gyrus, Ammon’s horn, and the subiculum). The hippocampal sulcus separates the parahippocampal and dentate gyri. The fimbriodentate sulcus separates the dentate gyrus and the fimbria of the hippocampus, which collects hippocampal efferents as a bundle at the edge of the choroid plexus before leaving the hippocampus to form the crus of the fornix. The amygdala and hippocampal formation lie beneath the medial temporal surface. The sylvian surface forms the superior boundary of the temporal lobe and the lower lip of the opercular cleft. The anterior sylvian surface consists of the planum polare, formed by the upper edge of the STG. The posterior sylvian surface consists of the planum temporale, formed by Heschl’s gyrus and the transverse temporal gyri. The temporal lobe houses important neurologic functions: memory and learning in the hippocampus and parahippocampus; language reception in Wernicke’s area in the dominant STG; auditory reception in Heschl’s gyrus; and transmission of visual signals in the optic radiations. Fig. 12.1 Microsurgical anatomy of the temporal lobe. (a) Lateral temporal surface (lateral view). (b) Basal temporal surface (inferior view). (c) Sylvian surface (anterior view with frontal and parietal lobes partially removed). (d) Sylvian and medial surfaces (superior view with axial sections through the temporal horns and partial removal of the occipital lobes, and on the right side, a coronal section through the temporal pole with choroid plexus removed). The temporal lobe has an intimate relationship with the middle cerebral artery (MCA) coursing through the sylvian fissure, with the posterior cerebral artery (PCA) coursing through the crural and ambient cisterns, and with the anterior choroidal artery (AChA) supplying the choroid plexus of the temporal horn of the lateral ventricle (Fig. 12.2). In contrast to frontal arteriovenous malformations (AVMs) that are supplied by branches from the superior trunk of the MCA, temporal AVMs are supplied by branches from the inferior trunk. The inferior trunk divides into approximately four unnamed stem arteries devoted to the temporal lobe and comprising the M2 insular and M3 opercular segments. These arteries emerge from the sylvian fissure distally to become M4 cortical arteries: middle temporal (MidTempA), poste rior temporal (PosTempA), temporo-occipital (TempOccA), and angular artery (AngA). They course downward from the sylvian fissure in an inferior direction and supply the lateral temporal surface. Collectively, they are referred to as “superior temporal arteries” because of this superior relationship to their territories. Temporopolar (TempPolA) and anterior temporal arteries (ATAs) are “early branches” that do not arise from the inferior trunk or travel the long course of the sylvian fissure, but instead arise from the M1 segment proximal to the MCA bifurcation. TempPolA is a small branch distal to the internal carotid artery (ICA) bifurcation and proximal to the ATA, but it enlarges in the presence of an AVM. Both of these arteries originate from the inferior surface of the M1 segment, course inferiorly, and supply the temporal pole. Fig. 12.2 Microsurgical anatomy of temporal lobe arteries. (a) The lateral surface is supplied by “early branches” arising from the M1 MCA (TempPolA and ATA), “superior temporal arteries” from the inferior trunk of the MCA (MidTempA, PosTempA, TempOccA, and AngA), and “inferior temporal arteries” from the PCA (HippoA and PosTempA) (lateral view). (b) The sylvian surface is supplied by M2 and M3 segments of MCA stem arteries (anterior view frontal and parietal lobes partially removed). (c) The basal surface is supplied by posterior temporal artery, shown here as a common trunk that divides into anterior, middle, and posterior branches. (d) Arteries of the sylvian and medial surfaces (superior view with axial section through the left temporal horn and partial removal of the occipital lobe). (e) The medial surface is supplied by HippoA (inferior view with parahippocampus removed). (f) The temporal horn is supplied by anterior choroidal artery (inferior view with parahippocampus removed). The posterior cerebral artery (PCA) supplies the basal surface of the temporal lobe with branches originating from the P2 segment: hippocampal (HippoA) and posterior temporal arteries (PosTempA). The HippoA is the first PCA cortical branch, arising in the crural or ambient cistern and supplying the uncus, anterior parahippocampal gyrus, hippocampus, and dentate gyrus. The PosTempA can arise as a common trunk that branches into anterior, middle, and posterior branches, or it can originate as individual anterior, middle, and posterior branches. Collectively, these hippocampal and posterior temporal arteries are referred to as “inferior temporal arteries.” They originate from the inferolateral PCA surface and course over the tentorial incisura in the subtemporal plane. They continue past the lateral margin of the basal surface to reach the lateral surface (ITG) and can ascend to the MTG. Venous anatomy of the temporal lobe is a complex collateral network with drainage anteriorly to temporopolar veins and the sphenoparietal sinus, posteriorly to the vein of Labbé and transverse sinus, medially to the basal vein of Rosenthal (BVR) and Galenic system, and superiorly to the sylvian veins and the superior sagittal sinus (SSS) (Fig. 12.3). The lateral temporal convexity is drained by descending veins (AntTempV, MidTempV, and PosTempV) that collect in the vein of Labbé and transverse sinus (TrvS) proximal to the transverse–sigmoid junction. The basal surface is drained by temporobasal veins (TempBasV; anterior, middle, and posterior) that collect laterally in tentorial sinuses and rarely in sphenobasal and sphenopetrosal sinuses, or medially in the BVR. The medial surface of the temporal lobe is drained by the uncal (UncV), anterior hippocampal (HippoV), and medial temporal vein (MedTempV), which collect in the BVR en route to the vein of Galen (VoG). The sylvian surface of the temporal lobe, as well as some of the STG along the sylvian fissure, drain into the temporosylvian veins (TempSylV) that ascend to SupSylV. Anastomotic veins can direct this venous flow anteriorly to SphParS and the cavernous sinus, superiorly to the frontoparietal veins, or deep to DeepSylV and the BVR. Fig. 12.3 (opposite) Microsurgical anatomy of the temporal lobe veins. (a) Veins of the lateral surface (lateral view). (b) Veins of the sylvian surface (anterior view with frontal and parietal lobes partially removed). (c) Veins of the medial surface (anterior view with frontal and parietal lobes partially removed). (d) Veins of the temporal horn (anterior view with frontal and parietal lobes partially removed). (e) Veins of the basal surface (inferior view). (f) Veins of the sylvian and medial surfaces (superior view with axial section through the left temporal horn and partial removal of the occipital lobe). Temporal AVM subtypes include one for each surface: lateral temporal, basal temporal, sylvian temporal, and medial temporal. Lateral temporal lobe AVMs are based on or immediately beneath the lateral convexity (Fig. 12.4). These are the most common of all subtypes, and by far the most common temporal subtype, accounting for over two thirds of temporal AVMs. Superior temporal arteries from the inferior trunk of the MCA are the feeders to these lateral AVMs. The dominant feeding artery varies with the nidus location in the lateral temporal lobe, with the ATA and MidTempA feeding anterior temporal AVMs and PosTempA and TempOccA feeding posterior temporal AVMs. The MCA feeding arteries emanate from the sylvian fissure and intersect the nidus along its superior border. The ATA and TempPolA wrap around the temporal pole and intersect anteriorly. The PosTempA from the P2 PCA contributes to AVMs that are inferiorly located in the ITG. The AChA is involved with larger AVMs with an ependymal plane in the temporal horn. Venous drainage is superficial, with minor deep drainage only with larger AVMs. Drainage usually descends posteriorly through AntTempV, MidTempV, and PosTempV to the vein of Labbé and the TrvS, but may also ascend to TempSylV, SupSylV, and SphParS. Wernicke’s speech area is associated with lateral temporal AVMs in the STG beyond 5 cm from the temporal pole. Arteriovenous malformations on the basal temporal surface reside in the ITG, fusiform, and/or parahippocampal gyri (Fig. 12.5). They are not visible on the lateral temporal surface and become apparent only after subtemporal dissection. Basal temporal AVMs are fed by MCA and PCA branches, but PCA dominates. PosTempA emanates from the crural or ambient cisterns, courses over the tentorial incisura, and supplies the medial AVM border. These feeders are deep to the AVM and may not be accessible until after circumferential dissection around the anterior and posterior sides of the nidus. The MCA branches (AntTempA, MidTempA, and PosTempA) wrap around the ITG to supply the lateral margin. The basal surface is intimate with the dura of the middle fossa and has meningeal feeders in nearly one quarter of patients. The AChA is not involved with these lesions. The TempBasVs (anterior, middle, and posterior) drain basal temporal AVMs and typically remain superficial, but one third will have deep connections to the BVR. Sylvian AVMs in the temporal lobe are based on its superior surface, which is oriented vertically down the fissure (Fig. 12.6). The nidus may be apparent on this cortical surface or it may lie just beneath, in which case an arterialized vein can offer a landmark. Sylvian temporal AVMs respect insular and frontal cortex, and separate from them completely. Sylvian temporal AVMs are deep to and supplied by M3 opercular segments. These stem arteries supply the AVM as feeding trunks or insular branches before they exit the sylvian fissure to become cortical M4 arteries (MidTempA, PosTempA, TempOccA). These arteries supply the medial and superior margins of the AVM. The AChA may supply the medial margin when it extends to the temporal horn. The PCA does not typically feed these AVMs. Venous drainage is superficial via TempSylV, SupSylV, and DeepSylV. These AVMs are only eloquent when they are in Heschl’s gyrus or posterior enough to involve Wernicke’s area in the dominant hemisphere. Fig. 12.4 The lateral temporal AVM subtype: (a) lateral and (b) superior cross-sectional views. This AVM is located on the lateral temporal surface, supplied by early temporal arteries from the M1 segment (ATA and TempPolA) and superior temporal arteries from the inferior MCA trunk, and drained by ascending and descending lateral temporal veins. Fig. 12.5 The basal temporal AVM subtype: (a) inferior and (b) superior cross-sectional views. This AVM is located on the basal temporal surface, supplied by inferior temporal arteries from the PCA (PosTempA), with minor contributions from MCA branches, and drained by temporal basal veins. Fig. 12.6 The sylvian temporal AVM subtype: (a) anterior view with frontal and parietal lobes partially removed, and (b) superior cross-sectional view. This AVM is located on the sylvian temporal surface, supplied by M3 opercular stem arteries, and drained by sylvian veins (TempSylV, SupSylV, and DeepSylV). The medial temporal AVM resides in the block of tissue medial to the temporal horn in the uncus, parahippocampal gyrus, and/or hippocampus (Fig. 12.7). This cortical surface is the inside edge of the temporal lobe. A deep transsylvian dissection that follows the AChA, mobilizes the temporal lobe away from the frontal lobe, opens the crural and ambient cisterns, and traces the tentorial incisura around the midbrain affords the only surgical view of this region, and it is limited at best. Inaccessibility makes medial temporal AVMs challenging. Transsylvian dissection leads to feeders from the AChA and the P2 PCA running along the medial and inferior aspect of the nidus, respectively. The cisternal segment of the AChA is always a transit artery that continues to supply the optic tract and internal capsule. HippoA and PosTempA supply these AVMs, with the parent P2 PCA also continuing to supply the occipital lobe while transmitting normal branches like the peduncular (PedP), circumflex (CirP), and thalamogeniculate perforators (ThGenP). The arterial supply may also come from the anterior thalamoperforators (ThaP) from the posterior communicating artery (PCoA), TempPolA, and ATA, particularly with more anteriorly located (i.e., uncus) medial temporal AVMs. Medial temporal AVMs that are more posteriorly located (i.e., behind the lateral edge of the cerebral peduncle, or parahippocampal gyrus) have increasing supply from PCA branches, including PosTempA and lPChA. Medial temporal AVMs drain deep to the BVR, and may have minor venous drainage posterolaterally through the basal temporal veins or anterolaterally through deep sylvian veins. Involvement of the hippocampus in memory function makes these AVMs eloquent, particularly in the dominant hemisphere. Fig. 12.7 The medial temporal AVM subtype: (a) inferior and (b) superior cross-sectional views. This AVM is located on the medial temporal surface, supplied by medial ICA branches (AChA and PCoA) and medial PCA branches (HippoA and PosTempA), and drained by medial temporal veins collecting in the BVR.
 Microsurgical Anatomy
Microsurgical Anatomy
Brain
Arteries
Veins
 Four Temporal AVM Subtypes
Four Temporal AVM Subtypes
The Lateral Temporal AVM
The Basal Temporal AVM
The Sylvian Temporal AVM
The Medial Temporal AVM
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree