♦ Preoperative
Preoperative Work-up
- Extensive evaluation by the epilepsy neurology team usually involving detailed seizure and medication history, inpatient video-electroencephalogram (EEG) monitoring with recording of some seizures, neuropsychologic evaluation, magnetic resonance imaging, and other tests in specific cases (e.g., intracarotid amobarbital [Wada] test, magnetoencephalograph, single photon emission computed tomography, positron emission tomography) to determine both lateralization and intrahemispheric localization of seizure onset.
- In case of discordant or unclear findings, preoperative evaluation will also include invasive intracranial EEG recording (e.g., subdural strips and/or grids ± depth electrodes).
- Concordance of EEG and imaging findings implicating temporal lobe pathology portends better postoperative seizure-free outcome.
- Anticonvulsant medications are often tapered preoperatively to facilitate preoperative evaluation or if intraoperative recording is performed.
Anesthetic Issues
- Standard general anesthesia is most commonly used.
- Some centers employ awake craniotomy (especially for dominant temporal lobectomy) for two reasons:
- The need to perform intraoperative functional cortical mapping
- The desire to minimize drug-induced interference with intraoperative electrocorticography
- The need to perform intraoperative functional cortical mapping
- In such cases, the surgeon will be called upon to perform a scalp block with local anesthetic as well as dural infiltration as needed during the procedure.
♦ Intraoperative
Standard Temporal Lobectomy (Fig. 57.1A)
Overview
- Defined as resection of the anterior temporal lobe including the hippocampus and parahippocampal gyrus at a standardized length, which may be shorter in the dominant hemisphere (e.g., 4.5 cm) than on the nondominant side (e.g., 5.5 cm)–resection lengths may vary between centers
- Originally described as en bloc anterior temporal lobectomy in which neocortical and mesial temporal structures are removed together in one specimen
- Most current temporal lobectomies, however, are performed in a staged procedure with removal of temporal neocortex followed by resection of deep structures.
- For purposes of brevity, the details of intraoperative electrocorticography and tailored resections are not covered in this chapter.
Positioning
- Head is positioned so that the lateral surface of the temporal lobe is approximately horizontal
- Patient is positioned supine with the shoulder elevated and the head turned, or in the full lateral position
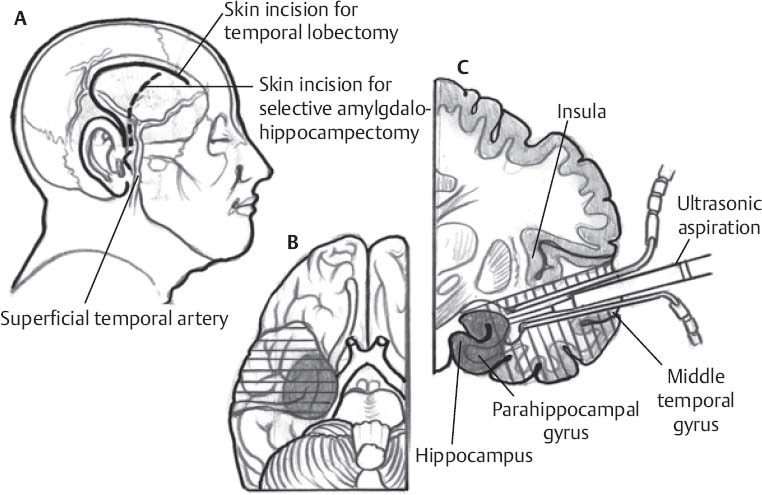
Fig. 57.1 (A) Schematic of exposure for standard temporal lobectomy versus selective amygdalohippocampectomy. (B,C) Comparison of tissue removed with standard temporal lobectomy versus SAH.
Incision, Craniotomy, and Dural Opening
- Standard scalp incision is a curvilinear or “question mark” shape extending from the superior border of the zygomatic arch just in front of the tragus above the auricle then superiorly and anteriorly to the hairline; this spares the frontalis branch of the facial nerve and can also be performed so as to preserve the superficial temporal artery.
- The temporalis muscle is incised and reflected inferiorly leaving an appropriate cuff, or may be elevated together with the skin as a musculocutaneous flap.
- A standard temporal craniotomy is fashioned to expose the superior temporal gyrus (STG) and middle temporal gyrus (MTG), with the superior margin 1 cm above the sylvian fissure (more frontal lobe is exposed if intraoperative electrocorticography will be performed).
- The inferior and anterior margins of the craniotomy are rongeured to reach the floor of the middle fossa and temporal pole.
- The dura is opened and reflected anteriorly.
Lateral Neocortical Removal
- The length of resection from the temporal pole (e.g., ~4.5 cm on the dominant side, ~5.5 cm on the nondominant side) is measured with a Cushing needle or other measuring device.
- The pia of the STG parallel to the sylvian fissure is coagulated, and also perpendicularly at the posterior resection margin down to the floor of the middle fossa
- The plane between the STG and the sylvian fissure is dissected subpially with a Penfield dissector or with the ultrasonic aspirator, protecting the middle cerebral artery (MCA) and its candelabra; this subpial dissection is carried down to the uncus inferomedially.
- Next step is identification of the ventricle, done by incising the temporal stem at the inferior Circular sulcus in the proper trajectory; an incision too medial may result in injury to the optic tract (producing a hemianopsia); an incision too lateral will result in missing the ventricle and arriving at the cortex over the floor of the middle fossa.
- Entry into the ventricle is confirmed by the appearance of bluish ependyma, choroid plexus, CSF, and/or view of the ventricular surface of the hippocampus.
- Disconnection of the neocortical block can be completed: first, a disconnection line is fashioned slightly oblique from the inferior circular sulcus and extended basally just lateral to the ventricle; second, dissection down to the arachnoid deep to the lateral neocortical gyri is accomplished with the ultrasonic aspirator to approximately the level of the collateral sulcus; third, the posterior margin of the neocortical incision can then be extended to join with the prior disconnection to the ventricle; lastly, the remaining arachnoid attachments of the neocortical block are cut, and it can be removed.
Mesial Resection
- Resection of the mesial structures (amygdala, uncus, hippocampus, parahippocampal gyrus [PHG], and entorhinal cortex) is next
- The uncus can be emptied with the ultrasonic aspirator at a low setting extending mesiobasally at the level of the limen insulae (working parallel to the ascending M1 segment)
- Next, the temporal horn is further opened extending to the anterior tip
- The choroid plexus, choroidal fissure, pes hippocampus, head and anterior body of the hippocampus, and amygdala will be in view within the ventricle; the hippocampus lies within the floor of the temporal horn while the amygdala forms the roof of the anterior portion of the temporal horn.
- The choroidal point (anterior limit of the insertion of the choroid plexus in the choroidal fissure) is connected with the limen insulae along the choroid plexus–limen insulae (CP–LI) line.
- The portion of the amygdala inferolateral to the CP–LI line can now be removed with ultrasonic aspiration; during this step, the entorhinal cortex (anterior portion of PHG) will be transected and removed.
- The fimbria hippocampi, which forms the medial border of the hippocampus and the lateral boundary of the choroidal fissure, is next loosened from its attachments (taenia fimbriae) mediolaterally, revealing the hippocampal sulcus (hippocampal fissure), containing a duplicate layer of arachnoid covering the arterial branches (hippocampal arteries) from the P2 segment of the posterior cerebral artery (PCA) and anterior choroidal artery.
- The arachnoid of the PHG (i.e., the deeper of the two layers) is identified and sectioned, allowing the subpial elevation of the PHG out of its arachnoid bed.
- The small perforating vessels entering the hippocampal sulcus are identified and divided close to the substance of the hippocampus, allowing the mobilization of the combined block of PHG and hippocampus.
- This leaves only the posterior disconnection, which is done with the ultrasonic aspirator (to remove ~3 cm of hippocampus); the hippocampus-PHG block can then be removed (en bloc if desired).
- Following adequate hemostasis, the craniotomy is closed in standard fashion.
- The choroidal point (anterior limit of the insertion of the choroid plexus in the choroidal fissure) is connected with the limen insulae along the choroid plexus–limen insulae (CP–LI) line.
Selective Amygdalohippocampectomy (Figs. 57.1B, 57.1C)
Overview
- Selective amygdalohippocampectomy (SAH) refers to a group of procedures aimed at resection of mesial structures only without neocortical resection; it is not really “selective” as the PHG and uncus are also included in the resection.
- Indications include patients with clear evidence of mesial temporal lobe seizure foci or lesions and lack of involvement of lateral temporal neocortex (e.g., typical cases of mesial temporal sclerosis).
Positioning
- Patient is positioned either in a lateral decubitus position or supine with the shoulder elevated
- Head is placed in Mayfield pin fixation
- Unlike the position for standard temporal lobectomy, the head is turned so that the malar eminence is the highest point, making the sylvian fissure approximately vertical
Incision and Craniotomy
- A semilunar incision is used, extending from anterior to the tragus to the frontal area.
- The craniotomy extends superior to the sylvian fissure by ~1.5 cm (smaller than that used for a standard temporal lobectomy).
- The sphenoid ridge is flattened with the drill fairly deep to allow optimal dural retraction.
Dural Opening, Sylvian Fissure Dissection, and Entry into the Temporal Horn
- The dura is opened in semicircular fashion and reflected across the sphenoid ridge and orbit
- For transsylvian approach, the Sylvian fissure is opened from the carotid bifurcation through the MCA bifurcation and ~2.5 cm more distally, exposing the ascending M1 branch, the limen insulae, the anterior third of the insular cortex and associated M2 branches, and the mesial surface of the uncus and temporal pole. The positions of the lateral M2 branches–including temporopolar and anterior temporal arteries–are noted. The inferior circular sulcus is identified, which separates the temporal operculum from the insular cortex.
- An incision into the anterior temporal stem is made reaching back ~15 mm from the level of the limen insulae; opening of the temporal horn posteriorly is accomplished by carrying this incision ~12 to 15 mm down to the roof of the ventricle.
- Alternatively, the temporal horn may be found anteriorly after emptying the uncus and carrying the resection more posterior until the tip of the temporal horn is entered.
- For transcortical approach, the temporal horn may be entered via the MTG or by first opening the superior or middle temporal sulcus.
- A subtemporal approach to the lateral ventricle for SAH is another option.
Mesial Resection
- The uncus is emptied with the ultrasonic aspirator, taking care to set low values for suction and amplitude to leave the arachnoid intact.
- The bulging portion of the amygdala just opposite the head of the hippocampus along the CP–LI line can be identified grossly by its speckled brown color and resected with the ultrasonic aspirator or dissector; together with this, the entorhinal cortex (anterior extent of PHG) is resected.
- The temporal horn is opened further to better visualize the choroid plexus and choroidal fissure marking the mesial boundary of the hippocampal dissection; a disconnection is then made lateral to the hippocampus along the ventricular border lateral to the collateral eminence, using a dissector or an aspirator in the anteroposterior direction, aiming approximately to the level of the collateral sulcus.
- The fimbria hippocampi is disconnected mesially by gentle dissection of the taenia fimbriae attaching to the choroidal fissure, and the medial aspect of the PHG (subiculum) can then be subpially elevated with a dissector.
- Identification, coagulation, and transection of the hippocampal vessels in the hippocampal fissure is performed, with great care taken to preserve the larger trunks of the anterior choroidal artery and P2 segment of the PCA.
- The deeper arachnoid layer in the hippocampal fissure is cut over the PHG, allowing subpial dissection and elevation of the PHG.
- Finally, the combined hippocampus/PHG can be disconnected posteriorly by mediolateral transverse section with the ultrasonic aspirator, and can be freed from its arachnoidal cover either by rolling it from mesial to lateral or vice versa; the specimen can be removed en bloc if desired.
- Hemostasis is accomplished with oxidized cellulose (Surgicel), and the wound is closed in standard fashion.
♦ Postoperative
- Patient brought to the intensive care unit and extubated when fully awake
- Resumption of preoperative anticonvulsant doses (or per epilepsy neurology service)
- Patient is monitored for seizures with attention to known preoperative semiology
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue







