The Anatomy of the Neural Arch of the Lumbar Spine, with References to Spondylolysis, Spondylolisthesis, and Degenerative Spondylolisthesis
Van P. Roy
E. Barbaix
M. De Maeseneer
C. Pouders
J. P. Clarys
In spondylolysis, a local bony defect at the level of the pars interarticularis tends to create and may finally lead to an uni- or bilateral cleft within the neural arch. In a complete bilateral pars defect, spondylolysis may lead to spondylolisthesis, whereby the vertebral body together with the pedicles, the transverse processes, and the upper articular facets are separated from the laminae, the spinous process, and the inferior articular facets. In children and adolescents, spondylolytic changes result from overloading, probably with stress fractures as a precursor factor (1) and facilitated by a possible hereditary predisposition (2). This contrasts with degenerative spondylolisthesis in middle-aged or elderly patients, whereby degenerative changes of facet joints and intervertebral discs produce instability, which at a certain point may induce ventral slip of the upper vertebra of a vertebral motion segment without pars defect. Consequently, the morphology of the neuroforamen becomes irregular and flattened (3), compromising the normal topography of its content. The nerve root canal normally has an inverted teardrop- or ear-shaped section and is more oval toward its exit zone (3,4). Its widest part is situated in the subpedicular notch of the upper vertebra. The L5 lateral neurovascular canal is particularly long compared to higher lumbar levels (4) (Fig. 1.1 A,B). The morphology of the lateral neurovascular canal depends on the condition of the adjacent apophyseal rings, the endplates and the interposed intervertebral disc anteriorly, the pars interarticularis of the superior vertebra, the superior articular facet of the vertebra below and the ligamentum flavum posteriorly, as well as on the condition of the pedicles of the motion segment under consideration. A bony indentation originating from the pars defect may provide a bilobulated aspect of the neuroforamen with enlarged horizontal diameter. Transforaminal or corporotransverse ligaments may influence the morphology of the lateral neurovascular canal at its exit zone, reducing the superoinferior diameter or forcing the neurovascular content to pass through the available space within the lateral canal, depending on the localization of the ligaments (5). Besides a general classification of the ligaments related to the intervertebral canal, Amonoo-Kuofi and El-Badawi (6) presented a detailed classification and description of the ligaments at the exit zone, making a clear distinction between the topography of the L5 lateral canal and higher lumbar lateral canals. Some of these ligaments may contribute to entrapment when the neuroforamen becomes flattened in spondylolisthesis.
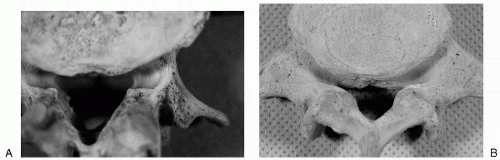 FIG. 1.1. A: Typical lateral neurovascular canal at upper lumbar levels. B: Typical lateral neurovascular canal at the L5 level. |
Spondylolysis, spondylolisthesis, and degenerative spondylolisthesis occur predominantly in the lower lumbar spine (3,7), irrespective of the different underlying mechanisms in isthmic spondylolysis and degenerative spondylolisthesis. This raises the question whether the lower lumbar spine presents a morphology that is more prone to spondylolytic and spondylolisthetic processes and/or is subjected to higher loading than higher lumbar levels. One of the most apparent anatomical differences is the spatial
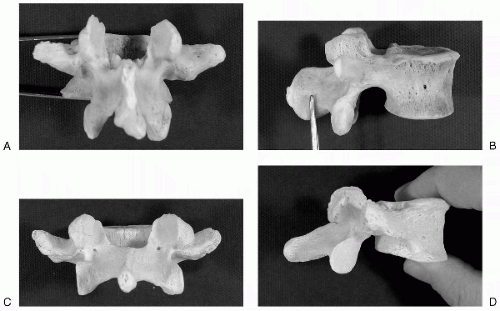
distribution of the superior and inferior facets with respect to their laminae. The height of the quadrangle resulting from an outline connecting the lateral margins of the four articular facets of the first lumbar vertebra is much larger than its width, whereas the opposite can be observed at the L5 level (8,9). The four facets of the upper two lumbar vertebrae fit in a trapezium, those of L4 in a square configuration, and those of L5 in a parallelogram whose long sides are horizontally oriented. As a result of a different spatial configuration of the facet joints, depending on their level, the height of the pars interarticularis decreases at lower lumbar levels (10), as does the distance between the transverse processes and the adjacent inferior facets (Fig. 1.2 A-D).
distribution of the superior and inferior facets with respect to their laminae. The height of the quadrangle resulting from an outline connecting the lateral margins of the four articular facets of the first lumbar vertebra is much larger than its width, whereas the opposite can be observed at the L5 level (8,9). The four facets of the upper two lumbar vertebrae fit in a trapezium, those of L4 in a square configuration, and those of L5 in a parallelogram whose long sides are horizontally oriented. As a result of a different spatial configuration of the facet joints, depending on their level, the height of the pars interarticularis decreases at lower lumbar levels (10), as does the distance between the transverse processes and the adjacent inferior facets (Fig. 1.2 A-D).
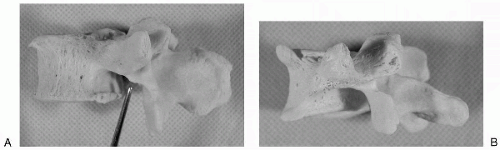 FIG. 1.3. A: The stronger lateral buttress* at higher lumbar levels. B: The lesser developed lateral buttress* at lower lumbar levels. |
Weiner et al. (11) described “the lateral buttress” of a lumbar vertebra, representing a bony bridge between the superolateral edge of the inferior articular facet and the inferior aspect of the junction between the pedicle and the processus costarius. In the upper lumbar spine, the presence of a larger lateral buttress at the cranial aspect of the lateral foramen provides a stronger bony reinforcement of the pars interarticularis than at lower levels (Fig. 1.3 A,B). Whereas cross-sectional areas of the pars gradually increase from L1 to L4 levels, only a slight increase is observed between L4 and L5 levels (12). However, remarkable local width differences with adjacent levels can be found (13).
DEVELOPMENT OF THE PARS INTERARTICULARIS
The entire lumbar vertebra develops from five ossification centers: one for the vertebral body, two for the apophyseal rings, and two for the neural arch. For a long time it was believed that each half of the neural arch develops from two ossification centers; then Willis (14) illustrated that overlooking the presence of a thin isthmus in these ossification centers caused the misconception. In the upper lumbar segments, the ossification centers appear somewhat earlier than in the lower segments: at 7 to 9 weeks versus 8 to 9 weeks of gestation (15). Endochondral ossification of the pars interarticularis starts at 12 to 13 weeks of gestation. In the upper lumbar segments, the ossification centers of the neural arch originate at the end of the pedicle and result in an isotropic configuration of the trabeculae and cortical bone in the region of the pars interarticularis. In lower lumbar segments, the ossification centers originate in the region of the pars interarticularis and
lead to an anisotropic configuration of trabecular and cortical bone in this region. Less densely trabeculated pedicles of smaller caliber appear in lower lumbar segments and the superior articular processes reveal a lesser trabecular density compared to the inferior articular processes (15). Cortical layers are thickest in the narrowest region of the pars, with the anterolateral aspect being thicker than the posteromedial one; the thickening is probably related to the amount of stress this part of the neural arch is subjected to during movement (1). Observations of trabecular and cortical bone at the cervicothoracic transition indicated that a layered morphology of the cortical bone of the neural arch and pars articularis deserves attention, especially in case of a poor or heterogeneous trabecular network (16).
lead to an anisotropic configuration of trabecular and cortical bone in this region. Less densely trabeculated pedicles of smaller caliber appear in lower lumbar segments and the superior articular processes reveal a lesser trabecular density compared to the inferior articular processes (15). Cortical layers are thickest in the narrowest region of the pars, with the anterolateral aspect being thicker than the posteromedial one; the thickening is probably related to the amount of stress this part of the neural arch is subjected to during movement (1). Observations of trabecular and cortical bone at the cervicothoracic transition indicated that a layered morphology of the cortical bone of the neural arch and pars articularis deserves attention, especially in case of a poor or heterogeneous trabecular network (16).
Although several congenital clefts of the posterior elements of lumbar vertebrae may occur (retrosomatic cleft, retroisthmic cleft, spina bifida), pars defect reveals a birth incidence of zero (15,17). Changes of the signal intensity of bone marrow on magnetic resonance (MR) images in lumbar pedicles are an ancillary sign of spondylolysis (18) and are often seen in degenerative joint disease (19).
BONY VARIANTS OF LUMBAR VERTEBRAE IN RELATION TO SPONDYLOLYSIS, SPONDYLOLISTHESIS, AND DEGENERATIVE SPONDYLOLISTHESIS
Variants of the Facet Joint Morphology
The shape, inclination, and curvature of lumbar articular facets may reveal important intra- and interindividual differences. The upper articular joint facets often have a C- or J-shaped configuration; others are flat. Corresponding differences exist in the inferior facets, which are usually slightly longer than the superior facets of the underlying vertebra. Curved superior facets can be seen as parts of cylindrical tubes, providing mainly upward and downward gliding of the corresponding inferior facets and thus allowing flexion, extension, and lateral bending but only limited axial rotation. Lateral bending is realized by downward gliding of the ipsilateral inferior facet and upward gliding of the contralateral inferior facet with respect to their articulating counterparts.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree