The Arteries of the Posterior Fossa
Key Points
Perforator branches of the brainstem are difficult to see angiographically but injury to them can be the mechanism of devastating ischemic deficits to the patient.
The proximal segments of the cerebellar arteries frequently give important perforator and circumflex branches to the brainstem before reaching the cerebellum itself.
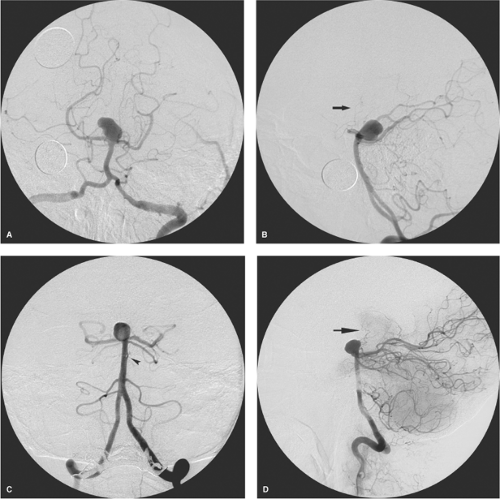
The basilar artery forms by fusion of the left and right vertebral arteries. It runs from the vertebrobasilar junction at the pontomedullary sulcus to the interpeduncular cistern, where it bifurcates behind the dorsum sellae. The level of the basilar bifurcation in reference to the posterior clinoid processes can have an important bearing on the surgical approach to basilar tip aneurysms (Fig. 15-1). More than 70% of basilar bifurcations lie level with or above the posterior clinoid processes (1). The other major anatomic determinant of surgical difficulty in approaching a basilar tip aneurysm is the attitude of the aneurysm to the artery in terms of whether it inclines anteriorly or posteriorly. An anteriorly pointing basilar tip aneurysm high above the clinoidal level is more favorable for surgical access. Aneurysms at a low basilar bifurcation or those that point posteriorly are considered inaccessible or hazardous.
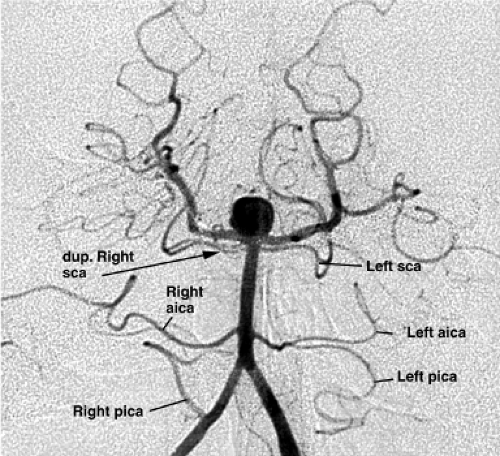
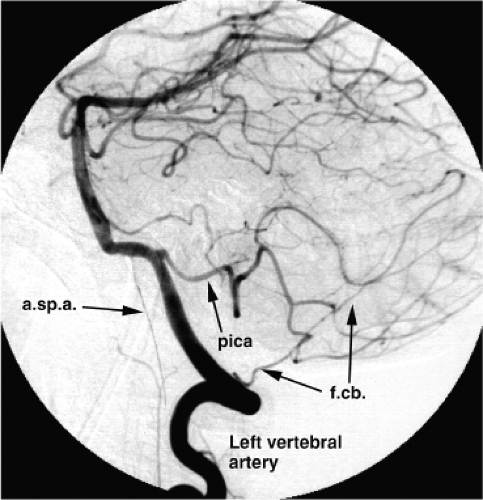
The vertebrobasilar system gives vascular supply to the posterior cerebral arteries and three pairs of named branches to the cerebellum. Smaller perforating and circumflex branches throughout its length supply the upper spine, medulla, pons, midbrain, and thalamus (Figs. 15-2–15-4). The posterior circulation is more prone than the anterior to demonstrate developmental anomalies or variants that can frequently be of clinical significance in the genesis of vascular pathology or during therapeutic procedures.
Intracranial Segment of the Vertebral Artery
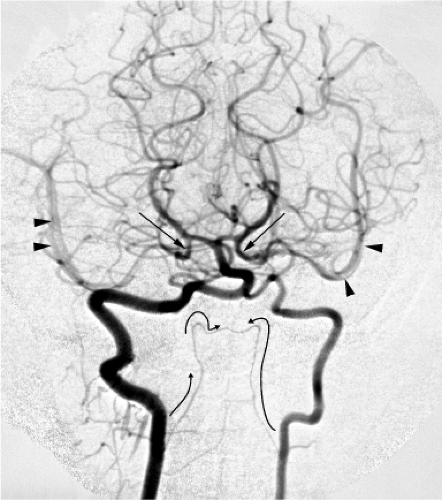
In approximately 60% of cases, the left vertebral artery is “dominant” or significantly larger than the right. Hypoplasia of the distal nondominant vertebral artery can be seen in varying degrees in approximately 5% to 10% of cases, underscoring the need to check the intracranial runoff before doing a full-volume power injection in a vertebral artery (Fig. 15-3). After traversing the atlanto-occipital membrane, the vertebral artery pierces the dura and enters the subarachnoid space usually in the lateral medullary cistern.
From the lateral medullary cistern, the vertebral arteries on their respective sides wind around the medulla oblongata anteriorly into the premedullary cistern. They fuse close to the midline with an angle of incidence between 30 and 90 degrees. Their meeting is most commonly at or within a few millimeters of the pontomedullary junction (2,3). The blood supply of the medulla is therefore predominantly from the intracranial segment of the vertebral arteries proximal to the vertebrobasilar junction, and to a lesser extent from small recurrent basilar artery branches that loop inferiorly.
Medially directed branches of the intracranial segment of the vertebral arteries supply the anterior medulla and pyramid. The most prominent of these vessels is the anterior spinal artery (Figs. 15-5–15-7), directed inferiorly along the anterior median sulcus (3). The anterior spinal artery is absent unilaterally in approximately 20% of postmortem angiograms (4). Moreover, the ideal appearance of bilateral symmetric spinal arteries fusing in the anterior median sulcus is frequently replaced by the configuration of a dominant vessel from one side supplying the major portion of flow. A connecting vessel between the left and right anterior spinal arteries can be seen occasionally at dissection and is termed the anterior spinal communicating artery.
The foramen cecum, also known as the Schwalbe foramen or the foramen of Vicq d’Azyr, is a median triangle-shaped fossicle on the anterior surface of the medulla at the pontomedullary junction at the superior end of the ventral median sulcus (5). This fossa fills a role analogous to that played by the anterior and posterior perforated substance at the base of the brain, in that it is traversed by a number of small (<1 mm) perforator vessels. These vessels penetrate the brainstem to provide vascular supply as far back as the tegmentum and floor of the IV ventricle. The brainstem perforators observe a sharp demarcation of the midline and do not give bilateral supply. Compromise of these vessels is responsible for the long tract or nuclear substrate
of brainstem syndromes associated with occlusive infarcts there.
of brainstem syndromes associated with occlusive infarcts there.
The lateral branches of the intracranial segment of the vertebral artery include the posterior inferior cerebellar artery and circumferential branches to the inferior cerebellar peduncle, lateral medulla, and the olivary structures. The posterior inferior cerebellar artery usually arises from the vertebral artery at the level of the olive, but may be either absent, hypoplastic, or arise from the basilar artery. It may alternatively arise more proximally from the vertebral artery as low as the C2 vertebral body and have an initially extradural course. Rarely, the posterior inferior cerebellar artery may arise from an alternative source in the suboccipital region such as the occipital artery or ascending pharyngeal artery, or from the internal carotid artery as a remnant of the trigeminal artery (6,7,8,9). The medullary segment of the posterior inferior cerebellar artery also gives medullary branches, which anastomose with those arising directly from the vertebral artery.
The lateral spinal artery of the upper cervical cord may take origin from the intradural segment of the vertebral artery or from the posterior inferior cerebellar artery posterior to the medulla (8). The lateral spinal artery is usually
small and difficult to see during angiography. Augmentation of the vascular territory of the lateral spinal artery can be seen in congenital diminutive variations of the suboccipital vertebral artery and of the posterior inferior cerebellar artery origin. This vessel usually runs caudally posterior to the dentate ligament and anterior to the posterior nerve roots of the upper four cervical levels. Below this point, it joins or is replaced by the posterior spinal artery.
small and difficult to see during angiography. Augmentation of the vascular territory of the lateral spinal artery can be seen in congenital diminutive variations of the suboccipital vertebral artery and of the posterior inferior cerebellar artery origin. This vessel usually runs caudally posterior to the dentate ligament and anterior to the posterior nerve roots of the upper four cervical levels. Below this point, it joins or is replaced by the posterior spinal artery.
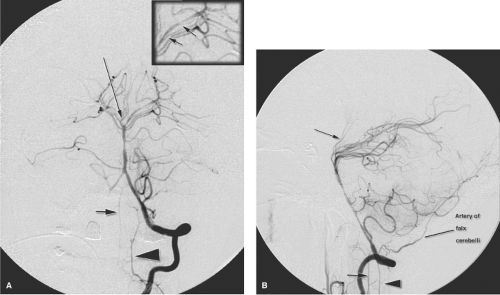
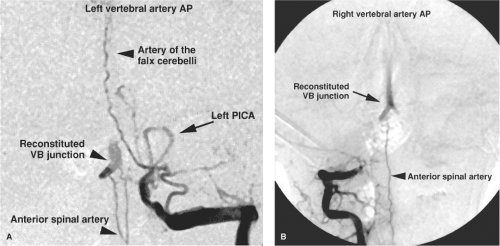 Figure 15-6. (A–B) Anterior spinal artery collateral flow to the basilar artery. PA views of the left vertebral artery (A) and right vertebral artery (B) in a patient with bilateral distal vertebral artery occlusions and ischemia of the basilar artery territory. The left vertebral artery is occluded distal to the origin of the left posterior inferior cerebellar artery. However, the artery of cervical enlargement lower in the neck opacifies the anterior spinal artery, which has collateralized the vertebrobasilar junction. The midline course of the artery of the falx cerebelli is well seen. The right vertebral artery (B) is occluded just proximal to the dural margin. The anterior spinal artery is seen again from this side flowing retrogradely to opacify the intracranial circulation.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|